主动脉夹层是指由于血管内膜局部撕裂后受到血液冲击,使内膜逐步剥离,在主动脉内形成真假两腔的血管病变。由于主动脉夹层起病隐匿,如未得到及时有效的处理,发生主动脉破裂的风险较大,由此引起的病死率也较高[1]。
目前临床治疗主动脉夹层方法包括药物治疗、外科手术治疗和腔内隔绝术治疗。其中药物治疗的效果并不十分理想,外科手术的创伤大,患者耐受性差,而腔内隔绝术不仅疗效确切,而且创伤小、恢复快,在主动脉夹层的治疗中占有较大的优势[2]。常规的腔内隔绝术多采用股动脉切开置入管鞘,放置人工血管,使病变扩张的主动脉壁与血流隔绝。近年来预置血管缝合器的使用使得该术式更加微创,通过置入管鞘前在穿刺部位启动缝合器,术毕收紧缝线完成缝合,在拔除输送装置的同时完成打结止血,对周围组织的损伤较小[3]。笔者分析对比109例B型主动脉夹层患者采取不同治疗方式的手术疗效,探讨预置血管缝合器行B型主动脉夹层腔内隔绝术的效果,现将结果报告如下。
1 资料与方法
1.1 一般资料
选取本院收治的109例B型主动脉夹层患者根据入院顺序分为观察组和对照组。观察组55例患者,其中男40例,女15例;年龄29~65岁,平均年龄44.5岁;合并基础疾病:糖尿病21例,高血压28例,外周动脉粥样硬化11例;既往具有吸烟史27例;体质量指数(BMI)(23.5±1.7)kg/m2。对照组54例患者,其中男36例,女18例;年龄33~65岁,平均年龄47.0岁;合并基础疾病:糖尿病20例,高血压24例,外周动脉粥样硬化8例;既往具有吸烟史22例;BMI(23.3±2.0)kg/m2。对比两组患者的基线资料比较,差异无统计学意义(均P>0.05)。
1.2 纳入排除标准
纳入标准:⑴ 符合B主型动脉夹层腔内隔绝术的手术适应证;⑵ 术前超声等检查显示患者至少有一侧股主动脉未出现钙化、狭窄、畸形等原因;⑶ 股主动脉管径不低于7 mm;⑷由我院同一组具有3年以上该手术经验的医师完成手术;⑸ 治疗前获得患者的知情同意并签订协议书。排除标准:⑴ 合并严重的心肺功能障碍患者;⑵ 近期合并严重的感染性疾病的患者;⑶ 合并凝血功能严重障碍的患者;⑷ 合并腹股沟疝、斜疝的患者。
1.3 治疗方法
观察组患者采取预置2把ProGilde血管缝合器进行术后修复穿刺点,于腹股沟区域分离股主动脉,穿刺置入管鞘,插入导丝后拔除管鞘。沿导丝送入缝合器鞘管端,退出导丝。将操作杆旋转至与皮肤呈45°,与股动脉走向平行。观察孔搏动性喷血时,张开缝合翼。固定缝合装置,按下穿针器。拉出1根蓝线,绕于剪线口切断。收回缝合翼,退出缝合器至2根缝线露出。将蓝线收紧,以止血钳固定。从导丝交换孔送入短导丝,退出第1套缝合装置。经导丝送入第2套缝合装置,操作步骤同前。完成腔内隔绝术后依次处理缝合装置,拉紧1号蓝线,经打结盒打一渔夫结,退出修整器后同时勾住蓝、白线,在血管壁上将线结推紧后剪线。同法处理第2套缝合装置。
对照组采取传统缝合修复的方法,于腹股沟区域分离股主动脉,穿刺股动脉后置入管鞘,插入导丝后拔除管鞘,对穿刺点预扩张,行主动脉腔内隔绝术。术毕撤出输送器,阻断穿刺点血流,行连续水平褥式外翻缝合,缝合完毕后撤出恢复血流,排空缝合段血管内气体后打结。缝合皮下组织和皮肤。
1.4 术后处理
穿刺点局部加压包扎,术侧下肢制动,严密监测血压、心率、血氧饱和度等,应用扩血管药物、降压药物等控制血压、心率,预防性应用抗生素。肾病高危患者适当采用水化治疗。
1.5 观察指标
对比两组患者的手术时间、入路建立时间、下肢制动时间、退鞘后血管处理时间、住院时间的差异;比较两组患者的手术成功率(手术成功的标准:成功实施主动脉夹层腔内隔绝术,达到完全隔绝,患者生命体征稳定)、术后3个月手术部位的血管直径差异;比较两组患者的手术并发症(局部血肿、局部渗血、感染、迷走神经反射、术后伤口不适感等)。
1.6 统计学处理
数据分析在SAS 9.3软件包中处理,正态分布的计量指标采用均数±标准差( ±s)表示,计量资料的组间比较采用t假设检验;百分率、构成比组间比较采用χ2检验;P<0.05为差异有统计学意义。
±s)表示,计量资料的组间比较采用t假设检验;百分率、构成比组间比较采用χ2检验;P<0.05为差异有统计学意义。
2 结 果
2.1 两组患者的围手术期指标比较
与对照组比较,观察组手术时间[(98.2±21.7)min vs.(140.8±28.5)min]、退鞘后血管处理时间[(4.3±0.9)min vs.(9.1±1.8)m i n]、住院时间[(4.4±1.6)d v s.(5.9±1.8)d]均明显减少(均P<0.05),但观察组的住院费[(8.4±0.8)万元 vs.(8.1±0.6)万元]用高于对照组(P<0.05);观察组与对照组的下肢制动时间差异无统计学意义(P>0.05)(表1)。
表1 两组患者的围手术期指标比较( ±s)
±s)
Table 1 Comparison of the perioperative variables between the two groups of patients ( ±s)
±s)
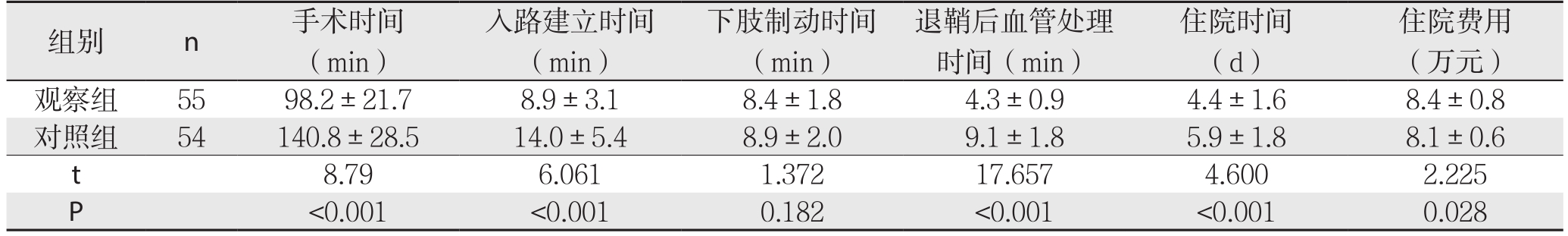
住院费用(万元)观察组 55 98.2±21.7 8.9±3.1 8.4±1.8 4.3±0.9 4.4±1.6 8.4±0.8对照组 54 140.8±28.5 14.0±5.4 8.9±2.0 9.1±1.8 5.9±1.8 8.1±0.6 t 8.79 6.061 1.372 17.657 4.600 2.225 P<0.001 <0.001 0.182 <0.001 <0.001 0.028组别 n 手术时间(min)入路建立时间(min)下肢制动时间(min)退鞘后血管处理时间(min)住院时间(d)
2.2 两组患者的手术成功率、术后3个月手术部位的血管直径比较
观察组与对照组的手术成功率、术后3个月手术部位的血管直径差异均无统计学意义(均P>0.05)(表2)。
表2 两组患者的手术成功率、术后3个月手术部位的血管直径比较
Table 2 Comparison of the surgical success rates and blood vessel diameters at the surgical site 3 months after operation between the two groups of patients
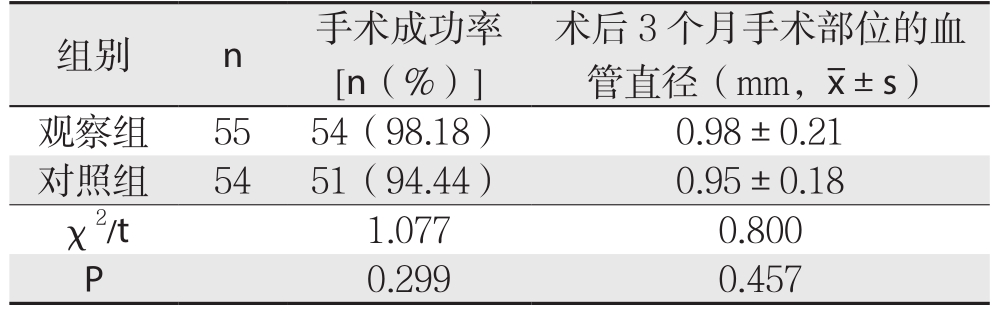
 观察组 55 54(98.18) 0.98±0.21对照组 54 51(94.44) 0.95±0.18 χ2/t 1.077 0.800 P 0.299 0.457
观察组 55 54(98.18) 0.98±0.21对照组 54 51(94.44) 0.95±0.18 χ2/t 1.077 0.800 P 0.299 0.457
2.3 两组患者的手术并发症比较
观察组4例患者出现术后并发症,对照组13例出现术后并发症,观察组的总并发症发生率明显低于对照组(7.27% vs.24.07%,P<0.05);对照组3例、观察组有1例因发生内漏实施二次手术(表3)。
表3 两组患者的手术并发症比较[n(%)]
Table 3 Comparison of the postoperative complications between the two groups of patients [n (%)]
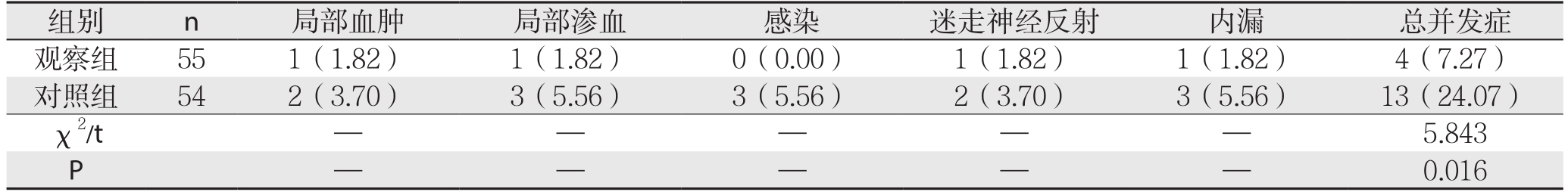
 观察组 55 1(1.82) 1(1.82) 0(0.00) 1(1.82) 1(1.82) 4(7.27)对照组 54 2(3.70) 3(5.56) 3(5.56) 2(3.70) 3(5.56) 13(24.07)χ2/t — — — — —5.843 P——0.016
观察组 55 1(1.82) 1(1.82) 0(0.00) 1(1.82) 1(1.82) 4(7.27)对照组 54 2(3.70) 3(5.56) 3(5.56) 2(3.70) 3(5.56) 13(24.07)χ2/t — — — — —5.843 P——0.016
3 讨 论
主动脉夹层的临床发病率并不高,以中老年人比较常见,男性患者多于女性患者[4]。由于患者的主动脉壁中层裂开,有流动或凝固的血液存在,病情十分凶险,如不及时处理,多数患者可在发病1周内死亡[5]。因此一旦发现主动脉夹层,应立即给予积极治疗。近年来,随着介入手术技术的发展和完善,腔内隔绝术已成为Stanford B型主动脉夹层的首选治疗方案[6]。传统的腔内隔绝术需要切开股动脉,完成对病变血管的处理后需要再缝合股动脉切口,需要麻醉科、血管外科等多科室共同协作[7]。术后可引起血肿、假性动脉瘤等血管并发症,给患者造成较大的痛苦[8]。
血管缝合器是一种新型的针对穿刺点局部的缝合装置,可减轻血管损伤,提高缝合效果[9]。近年来,血管缝合器在临床的适用领域越来越广泛,在心血管介入术、神经介入术等手术中应用血管缝合器封闭穿刺入路均起到了良好的效果[10-12]。在腔内隔绝术中预置血管缝合器的方法可行完全穿刺途径,大大简化了手术方式,受到临床的一致好评[13-14]。有研究[15]发现,在对12 F以下的穿刺口进行封闭时,应用1把ProGilde血管缝合器即可获得满意的封闭效果,对12~24 F直径的缝合伤口则需要2把ProGilde血管血管缝合器。如遇穿刺部位血管条件欠佳,钙化灶较多者,则考虑3把ProGilde血管血管缝合器[16]。需要注意的是,对于过度肥胖、血管钙化、血管弯曲等患者,血管缝合器的置入封闭效果较差,因而建议采用手术切开治疗[17]。
有研究[18]表明,在腔内隔绝术中预置血管缝合器可简化手术操作,使手术时间大大缩短。本研究的结果也充分印证了这一点,观察组患者的手术时间、退鞘后血管处理时间均显著的低于对照组患者。而观察组患者术后住院时间显著的低于对照组患者,这一结果提示,在腔内隔绝术中预置血管缝合器可促进术后康复进程[19]。观察组和对照组的下肢制动时间比较差异无统计学意义,但在数值上,观察组患者下肢制动时间略低于对照组患者,这一结果提示,在腔内隔绝术中预置血管缝合器有可能缩短下肢制动时间,但尚有待于进一步的研究证实。观察组患者和对照组患者的手术成功率、术后3个月手术部位的血管直径差异均无统计学意义,这一结果提示,预置血管缝合器行B型主动脉夹层腔内隔绝术对手术效果并无明显影响。观察组患者有4例患者出现术后并发症,对照组有13例患者出现术后并发症,观察组的手术并发症率7.27%显著的低于对照组的24.07%且差异具有统计学意义,这一结果提示预置血管缝合器行B型主动脉夹层腔内隔绝术的并发症更少,其优势也主要体现在这一点上。上述结果也与已有的临床研究结果一致[20]。本研究中对照组有3例患者、观察组有1例患者因发生内漏实施二次手术。
需要注意的是,预置血管缝合器的方法并不适用于所有人群[21]。过度肥胖、血管钙化、血管弯曲等患者均不宜采用本方法,因此术前应严格掌握适应证,以防缝合失败[22-23]。此外,由于血管缝合器价格昂贵,在临床的推广受到一定的限制[24]。在临床工作中可向患者宣传血管缝合器的优势,促进其在临床的推广应用[25]。
本研究结果表明,预置血管缝合器行B型主动脉夹层腔内隔绝术具有安全高效、手术效果可靠、术后并发症少的优点。
参考文献
[1]Peng LQ, Yang ZG, Yu JQ, et al.Isolated interrupted aortic arch accompanied by type B aortic dissection and extensive collateral arteries diagnosed with MDCT angiography[J].Clin Imaging, 2012,36(5):602–605.doi: 10.1016/j.clinimag.2011.12.021.
[2]毛文凯, 王黎明, 祁国荣, 等.主动脉覆膜支架腔内隔绝术治疗成人巨大动脉导管未闭[J].中国胸心血管外科临床杂志, 2012,19(2):202–204.Mao WK, Wang LM, Qi GR, et al.Endovascular exclusion with covered stent in treatment of adult large patent ductus arteriosus[J].Chinese Journal of Clinical Thoracic and Cardiovascular Surgery,2012, 19(2):202–204.
[3]袁慧锋, 韩新巍, 任建庄, 等.头臂动脉旁路手术联合腔内隔绝术治疗主动脉弓夹层 (附10例报告)[J].山东医药, 2015, 55(27):58–59.doi:10.3969/j.issn.1002–266X.2015.27.023.Yuan HF, Han XW, Ren JZ, et al.Brachiocephalic artery bypass surgery combine with endovascular exclusion for aortic arch dissection (a report of 10 cases)[J].Shandong Medical Journal,2015, 55(27):58–59.doi:10.3969/j.issn.1002–266X.2015.27.023.
[4]龙超, 万毅, 吴明正, 等.腔内隔绝术治疗胸主动脉夹层的诊疗策略[J].重庆医学, 2015, 44(18):2509–2511.doi:10.3969/j.issn.1671–8348.2015.18.022.Long C, Wan Y, Wu MZ, et al.The strategy of diagnosis and treatment of endovascular graft exclusion in treating thoracic aortic dissection[J].Chongqing Medicine, 2015, 44(18):2509–2511.doi:10.3969/j.issn.1671–8348.2015.18.022.
[5]肖华, 杨洁莲, 彭丹丹, 等.不同术式入路对B型主动脉夹层腔内隔绝术的影响[J].介入放射学杂志, 2013, 22(9):730–733.doi:10.3969/j.issn.1008–794X.2013.09.007.Xiao H, Yang JL, Peng DD, et al.The effect of different approach on thoracic endovascular aortic repair for Stanford B type aortic dissection[J].Journal of Interventional Radiology, 2013, 22(9):730–733.doi:10.3969/j.issn.1008–794X.2013.09.007.
[6]邢丽, 袁婵娟, 陈茹妹, 等.主动脉夹层覆膜支架腔内隔绝术的手术配合[J].介入放射学杂志, 2014, 23(3):264–266.doi:10.3969/j.issn.1008–794X.2014.03.021.Xing L, Yuan CJ, Chen RM, et al.Nursing cooperation in endovascular aneurysm repair treatment for aortic dissection[J].Journal of Interventional Radiology, 2014, 23(3):264–266.doi:10.3969/j.issn.1008–794X.2014.03.021.
[7]王晓天, 胡何节, 邓福生, 等.腔内隔绝术在胸主动脉夹层及动脉瘤中的应用[J].安徽医科大学学报, 2013, 48(9):1127–1129.Wang XT, Hu HJ, Deng FS, et al.Application of endovascular graft exclusion in the thoracic aortic dissection and arterial aneurysm[J].Acta Universitatis Medicinalis Anhui, 2013, 48(9):1127–1129.
[8]廖凯兵, 席仁刚, 郑传胜, 等.腹主动脉瘤腔内隔绝术与外科开放手术的临床对比研究[J].放射学实践, 2012, 27(12):1382–1386.doi:10.3969/j.issn.1000–0313.2012.12.028.Liao KB, Xi RG, Zheng CS, et al.A comparative study of endovascular aortic repair and surgical open operation in the treatment of abdominal aortic aneurysm[J].Radiologic Practice, 2012, 27(12):1382–1386.doi:10.3969/j.issn.1000–0313.2012.12.028.
[9]王燕.腔内隔绝术治疗Stanford B型主动脉夹层动脉瘤的观察及护理[J].护士进修杂志, 2012, 27(20):1858–1860.doi:10.3969/j.issn.1002–6975.2012.20.015.Wang Y.Observation and nursing of endovascular exclusion for Stanford type B aortic dissection[J].Journal of Nurses Training, 2012, 27(20):1858–1860.doi:10.3969/j.issn.1002–6975.2012.20.015.
[10]王变丽, 施敏, 张丽娟, 等.腹主动脉瘤患者行覆膜支架腔内隔绝术的效果评价[J].中国实用护理杂志, 2012, 28(25):53–54.doi:10.3760/cma.j.issn.1672–7088.2012.25.025.Wang BL, Shi M, Zhang LJ, et al.Efficacy evaluation of endovascular exclusion with covered stent for patients with abdominal aortic aneurysm[J].Chinese Journal of Practical Nursing, 2012, 28(25):53–54.doi:10.3760/cma.j.issn.1672–7088.2012.25.025.
[11]杨帆, 王家平, 龙超, 等.带膜支架治疗Stanford B型胸主动脉夹层的疗效分析[J].介入放射学杂志, 2015, 24(3):197–199.doi:10.3969/j.issn.1008–794X.2015.03.004.Yang F, Wang JP, Long C, et al.Evaluation of endovascular covered-stent implantation in treating Stanford type B aortic dissection[J].Journal of Interventional Radiology, 2015, 24(3):197–199.doi:10.3969/j.issn.1008–794X.2015.03.004.
[12]李永东, 宫丽斌, 陈美俊, 等.人工压迫和Perclose血管缝合器的股动脉止血疗效比较[J].心血管康复医学杂志, 2014, 23(5):563–565.doi:10.3969/j.issn.1008–0074.2014.05.26.Li YD, Gong LB, Chen MJ, et al.Hemostasis effect comparison between artificial pressing and Perclose vascular closure device on femoral artery[J].Chinese Journal of Cardiovascular Rehabilitation Medicine, 2014, 23(5):563–565.doi:10.3969/j.issn.1008–0074.2014.05.26.
[13]王志伟, 王家祥, 管生, 等.近心端假腔血栓形成Stanford B型主动脉夹层的治疗[J].中国普通外科杂志, 2013, 22(12):1558–1561.doi:10.7659/j.issn.1005–6947.2013.12.007.Wang ZW, Wang JX, Guan S, et al.Management of Stanford type B aortic dissection with proximal false lumen thrombosis[J].Chinese Journal of General Surgery, 2013, 22(12):1558–1561.doi:10.7659/j.issn.1005–6947.2013.12.007.
[14]余维平, 景在平, 赵志青, 等.老年腹主动脉瘤腔内隔绝术围手术期脑保护的临床应用及意义[J].中国现代普通外科进展, 2014,17(4):328–329.doi:10.3969/j.iss.1009–9905.2014.04.025.Yu WP, Jing ZP, Zhao ZQ, et al.Clinical application and significance of cerebral protection in old patients undergoing endovascular aneurysm exclusion during perioperative period[J].Chinese Journal of Current Advances in General Surgery, 2014,17(4):328–329.doi:10.3969/j.iss.1009–9905.2014.04.025.
[15]许世宁, 王锋.全胸腔镜肺叶切除术中血管损伤致出血处理措施[J].现代仪器与医疗, 2015, 21(2):88–89.doi:10.11876/mimt201502033.Xu SN, Wang F.Treatment measures for bleeding due to vascular injury in total thoracoscopic lobectomy[J].Modern Instruments& Mediccal Treatment, 2015, 21(2):88–89.doi:10.11876/mimt201502033.
[16]叶鹏, 陈勇, 曾庆乐, 等.血管缝合器预缝合技术完全经皮穿刺途径完成主动脉腔内修复术后的股动脉中长期随访结果[J].南方医科大学学报, 2014, (5):747–750.doi:10.3969/j.issn.1673–4254.2014.05.33.Ye P, Chen Y, Zeng QL, et al.Long-term follow-up of the femoral artery after total percutaneous endovascular aortic repair with preclose technique using a vascular closure device[J].Journal of Southern Medical University, 2014, (5):747–750.doi:10.3969/j.issn.1673–4254.2014.05.33.
[17]熊斌, 郑传胜, 梁惠民, 等.Perclose Proglide血管缝合器在腹主动脉瘤腔内修复术中的应用分析[J].临床放射学杂志, 2013,32(9):1320–1323.Xiong B, Zheng CS, Liang HM, et al.Analysis of the Perclose Proglide Vascular Closure Devices in the Endovascular Abdominal Aortic Aneurysm Repair (EVAR)[J].Journal of Clinical Radiology,2013, 32(9):1320–1323.
[18]陈亮, 顾建平, 楼文胜, 等.覆膜支架腔内隔绝术治疗外周动脉瘤[J].介入放射学杂志, 2012, 21(2):107–110.doi:10.3969/j.issn.1008–794X.2012.02.005.Chen L, Gu JP, Lou WS, et al.Endovascular covered stent-graft exclusion of peripheral aneurysms[J].Journal of Interventional Radiology, 2012, 21(2):107–110.doi:10.3969/j.issn.1008–794X.2012.02.005.
[19]Chan WH, Huang YC, Weng HH, et al.Analysis of intimal extent and predictors of renal atrophy in patients with aortic dissection[J].Acta Radiol, 2012, 53(7):732–741.doi: 10.1258/ar.2012.110614.
[20]郭媛媛.多层裸支架腔内隔绝动脉瘤的研究现状及存在问题[J].中国普通外科杂志, 2012, 21(12):1566–1570.Guo YY.Current status and associated problems of multilayer bare stent in endovascular aneurysm exclusion[J].Chinese Journal of General Surgery, 2012, 21(12):1566–1570.
[21]李丹丹, 朱云峰, 葛红卫, 等.D-二聚体水平对急性主动脉夹层患者死亡预测价值的研究[J].中国普通外科杂志, 2016, 25(6):843–847.doi: 10.3978/j.issn.1005–6947.2016.06.011.Li DD, Zhu YF, Ge HW, et al.Value of D-dimer level for predicting death in patients with acute aortic dissection[J].Chinese Journal of General Surgery, 2016, 25(6):843–847.doi: 10.3978/j.issn.1005–6947.2016.06.011.
[22]戚悠飞, 舒畅, 罗明尧, 等.主动脉夹层患者升主动脉中层弹性蛋白与弹力纤维的变化[J].中国普通外科杂志, 2017, 26(6):729–734.doi:10.3978/j.issn.1005–6947.2017.06.010.Qi YF, Shu C, Luo MY, et al.Alterations of elastin and elastic fibers in tunica media of ascending aorta in patients with aortic dissection[J].Chinese Journal of General Surgery, 2017, 26(6):729–734.doi:10.3978/j.issn.1005–6947.2017.06.010.
[23]林长泼, 符伟国.主动脉夹层的治疗进展[J].中国普通外科杂志,2016, 25(6):790–794.doi: 10.3978/j.issn.1005–6947.2016.06.002.Lin CP, Fu WG.Advances in treatment of aortic dissection[J].Chinese Journal of General Surgery, 2016, 25(6):790–794.doi:10.3978/j.issn.1005–6947.2016.06.002.
[24]张喆, 陈学明, 李晨宇, 等.腔内治疗破口位于升主动脉的Stanford A型主动脉夹层[J].中国普通外科杂志, 2015,24(12):1649–1653.doi:10.3978/j.issn.1005–6947.2015.12.002.Zhang Z, Chen XM, Li CY, et al.Endovascular treatment for Stanford type A aortic dissection with entrance tear in ascending aorta[J].Chinese Journal of General Surgery, 2015, 24(12):1649–1653.doi:10.3978/j.issn.1005–6947.2015.12.002.
[25]张瑜, 朱健, 朱水波, 等.累及弓部主动脉夹层手术方式选择及疗效[J].中国普通外科杂志, 2016, 25(6):823–827.doi: 10.3978/j.issn.1005–6947.2016.06.007.Zhang Y, Zhu J, Zhu SB, et al.Selection of surgical procedures and efficacy analysis in treatment of aortic dissection involving aortic arch[J].Chinese Journal of General Surgery, 2016, 25(6):823–827.doi: 10.3978/j.issn.1005–6947.2016.06.007.
