胆总管结石在我国发病率高,患者分布广泛,是普外科常见疾病。其治疗方法种类繁多,技术手段也日新月异。目前以腹腔镜下胆总管探查(laparoscopic common bile duct exploration,L C B D E)+T管引流术为主要治疗手段,然而T管引流会带来电解质流失,住院时间延长,医疗费用增加等弊端,所以,不放置T管的胆总管探查为现阶段胆道外科研究的新方向[1]。目前,不放置T管的治疗方法包括经胆囊管胆总管探查术(laparoscopic transcystic common bile duct exploration,LTCBDE)、LCBDE+胆道一期缝合术、内镜逆行性胰胆管造影(endoscopic retrograde cholangiopancreatography,ERCP)+内镜乳头括约肌切开术(endoscopic sphincterotomy,EST)等[2-3]。我院于2013年1月—2015年12月,应用LTCBDE和LCBDE+胆道一期缝合术两种方法治疗胆囊结石合并胆总管结石104例。本文针对这两种手术方式予以对比分析。
1 资料与方法
1.1 一般资料
选取2013年1月—2015年12月在我院接受微创手术治疗的胆总管结石患者共131例,共有27例患者因胆道炎症较重、结石难以一次取尽、胆道狭窄等原因改行L C B D E+T管引流术。其余104例患者,男42例,女62例;平均年龄50.8岁。按手术方式不同分为两组:5 0例行L T C B D E(LTCBDE组),54例行LCBDE+胆道一期缝合术(LCBDE+一期缝合组)。根据患者病史、临床症状、体征、B超、MRCP、肝功能等评估术前情况,均满足以下条件:⑴ 排除肝内胆管结石、胆道恶性肿瘤;⑵ 胆总管直径≥8 mm,胆囊管直径≥3 mm,胆管无狭窄、畸形等病变;⑶ 既往无胆道手术及ERCP史,本次发病胆管炎症较轻。取成功完成手术的两组病例,比较其性别、年龄、病程、胆总管直径、胆囊管直径、胆总管内结石数量以及术前出现黄疸或肝酶异常的例数等一般情况。两组患者一般资料差异均无统计学意义(均P>0.05),具有可比性(表1)。
1.2 方法
1.2.1 手术方法 全身麻醉,取头高足低位,按四孔法置入Trocar,常规游离胆囊三角。分离并暴露胆囊管与胆总管交汇处,钛夹夹闭胆囊管远端,防止术中结石和胆汁进入胆总管或腹腔。⑴LTCBDE(LTCBDE组):于胆囊管前壁距汇入部约10 mm剪开1/2周径,用分离钳或胆道探子扩张胆囊管。从胆囊管切开处置入胆道镜,经胆囊管进入胆总管,边缓慢注水,边探查胆总管并取石。取石完毕后确认胆总管下段注水通畅,无结石残留。退出胆道镜,于胆囊管切口下方近汇入部上Hem-o-lok 1枚,离断胆囊管,顺行切除胆囊。若因胆囊管狭窄或解剖变异等原因,胆道镜进入胆囊管困难,可继续纵向扩大切口(3~5 mm)至汇入部,置入胆道镜探查,此法探查取石完毕后,汇合部的切口用4-0可吸收缝线行双层缝合,缝合至距离汇入部5 mm以上时,用Hem-o-lok夹闭胆囊管并切除胆囊。⑵ LCBDE+胆道一期缝合术(LCBDE+一期缝合组):切开胆囊管汇入部下2cm内胆总管前壁,见胆汁流出后,用剪刀纵向延长切口,约1.0~1.5cm。置入胆道镜探查胆总管并取石。取石完毕后确认胆总管下段通畅,无结石残留。用4-0可吸收缝线间断缝合胆总管切口。于胆囊管近端距胆总管0.5cm处上Hem-o-lok 1枚,远端离断,顺行切除胆囊。两种探查术后均于小网膜孔放置引流管,观察引流液体积、性状。
1.2.2 观察指标及术后随访 观察两组患者的手术时间、术中出血量、术后引流量、带管时间、住院天数、术后胆汁漏、术后胆道出血等指标进行对比分析。所有患者出院后接受定期的电话随访,若患者出现腹痛、发热、黄疸等症状,则进一步门诊随访,行B超、肝功能等检查,确认有无胆道狭窄、胆道感染等并发症并对比分析。随访时间1~36个月。
表1 两组患者一般资料比较
Table 1 Comparison of the general data of the two groups of patients
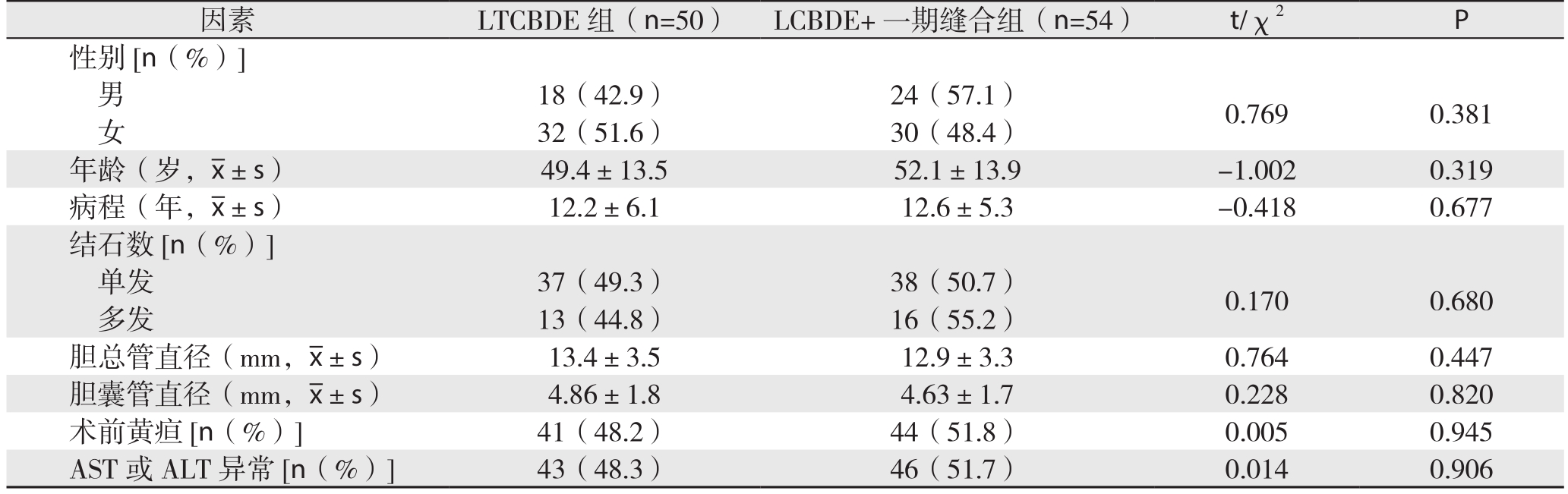
因素 LTCBDE组(n=50) LCBDE+一期缝合组(n=54) t/χ2 P性别[n(%)]男18(42.9) 24(57.1) 0.769 0.381女32(51.6) 30(48.4)年龄(岁,x±s) 49.4±13.5 52.1±13.9 -1.002 0.319病程(年,x±s) 12.2±6.1 12.6±5.3 -0.418 0.677结石数[n(%)]单发 37(49.3) 38(50.7) 0.170 0.680多发 13(44.8) 16(55.2)胆总管直径(mm,x±s) 13.4±3.5 12.9±3.3 0.764 0.447胆囊管直径(mm,x±s) 4.86±1.8 4.63±1.7 0.228 0.820术前黄疸[n(%)] 41(48.2) 44(51.8) 0.005 0.945 AST或ALT异常[n(%)] 43(48.3) 46(51.7) 0.014 0.906
1.3 统计学处理
采用SPSS 13.0软件。计量资料以均数±标准差![]() 表示,采用两独立样本t检验;计数资料用n表示,采用χ2检验。P<0.05为差异有统计学意义。
表示,采用两独立样本t检验;计数资料用n表示,采用χ2检验。P<0.05为差异有统计学意义。
2 结 果
2.1 两组术中与术后情况
与LCBDE+一期缝合组比较,LTCBDE组手术时间更短、术中出血量更少,术后引流量、带管时间及住院天数也明显减少,差异均有统计学意义(均P<0.05)(表2)。
2.2 两组术后随访结果及并发症的比较
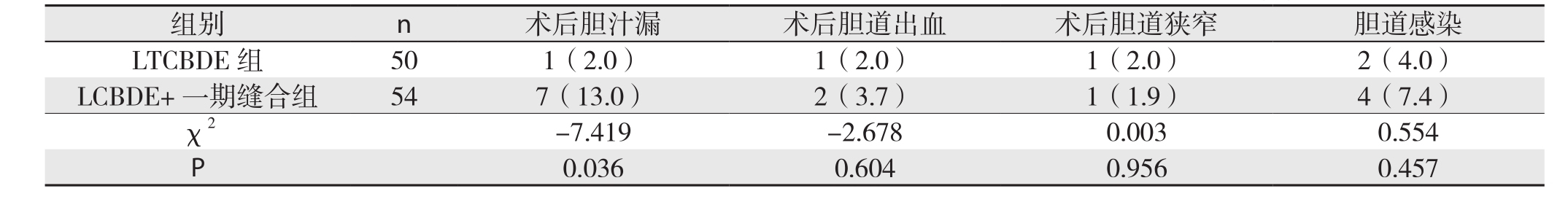
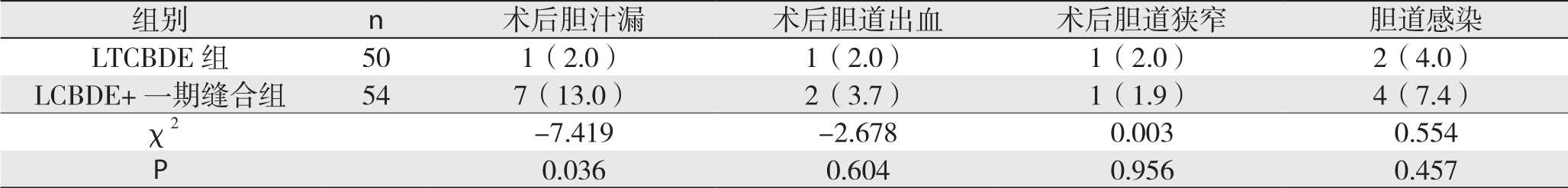
LTCBDE组有1例患者在术后第3天出现胆汁漏,持续腹腔引流10 d后治愈,LCBDE+一期缝合组共有7例患者出现胆汁漏,发生在术后3~7 d,均在持续腹腔引流7~15 d后治愈。LTCBDE组和LCBDE+一期缝合组分别有1例和2例患者出现术后胆道出血,于术后第2~3天出现,均在持续腹腔引流和促凝血治疗后缓解。LTCBDE组和LCBDE+一期缝合组各有1例患者分别于术后1个月和2个月出现胆道狭窄,均在反复球囊扩张后治愈。LTCBDE组和LCBDE+一期缝合组分别有2例和4例患者出现术后胆道感染,发生在术后2~4 d,均在升级抗生素治疗后好转。在术后胆道出血、胆道狭窄、胆道感染上,LTCBDE组略少于LCBDE+一期缝合组,但无统计学差异(均P>0.05)。在术后胆汁漏LTCBDE组明显少于LCBDE+一期缝合组,差异有统计学意义(P<0.05)(表3)。
表2 两组患者术中与术后指标比较( ±s)
±s)
Table 2 Comparison of the intra- and postoperative variables between the two groups (x±s)
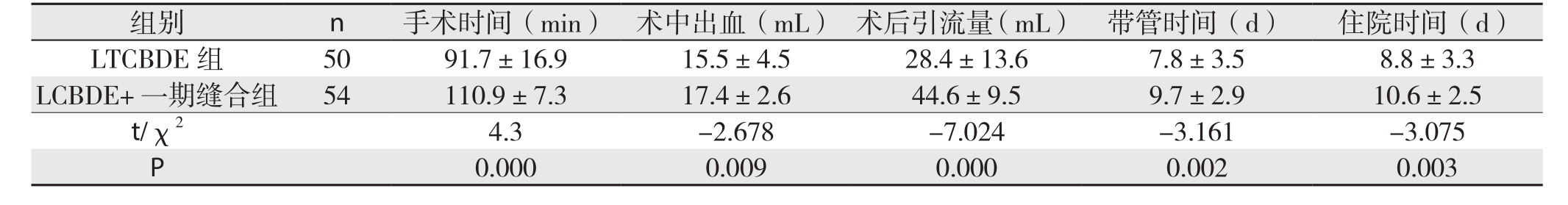
组别 n 手术时间(min) 术中出血(mL) 术后引流量(mL) 带管时间(d) 住院时间(d)LTCBDE 组 50 91.7±16.9 15.5±4.5 28.4±13.6 7.8±3.5 8.8±3.3 LCBDE+ 一期缝合组 54 110.9±7.3 17.4±2.6 44.6±9.5 9.7±2.9 10.6±2.5 t/χ2 4.3 -2.678 -7.024 -3.161 -3.075 P 0.000 0.009 0.000 0.002 0.003
表3 两组患者术后并发症比较[n(%)]
Table 3 Comparison of the postoperative complications between the two groups [n (%)]
3 讨 论
早期的开腹胆总管切开探查+T管引流术是治疗胆总管结石最为经典的术式。随着内镜技术的成熟,ERCP+EST发展迅速。然而,内镜下乳头括约肌切开取石会损伤Oddi括约肌的功能,引起反流性胆管炎,且技术要求高,医疗费用大,故长期以来饱受争议[4-5]。目前,基于微创技术进步的LCBDE逐渐普及,是治疗胆总管结石主流的手术方式[6],但常规切开胆总管后放置的T管会带来诸多问题[7-8],如术后电解质、消化液、消化酶的大量流失,长期带管出院可能引起胆道感染,患者生活质量下降,治疗时间延长,医疗费用增加等,所以,为避免放置T管所带来的弊端,LCBDE+胆道一期缝合术与LTCBDE应运而生[9-10]。
3.1 两种术式适应证和禁忌证的对比
目前,学术界对LTCBDE和LCBDE+胆道一期缝合术尚无确定的适应证,根据笔者临床经验并结合该研究的结果,两者共同的适应证归纳总结如下[11-16]:⑴ 术前MRCP确认为胆总管结石,无肝内胆管结石;⑵ 胆总管直径≥8 mm,无胆管狭窄或胆道肿瘤存在,胆管壁无明显充血水肿,无化脓性胆管炎;⑶ 胆总管结石直径≤1.5cm,数量<10枚;⑷ 取石后胆总管无结石残余且下段通畅,Oddi括约肌功能正常;⑸ 无胆道手术史及胰腺炎病史;⑹ 全身情况良好,无营养不良及低蛋白血症。
由于LTCBDE是经胆囊管入路,对胆囊管的解剖条件要求苛刻。胆囊管闭塞、扭曲,管径过细(直径<3 mm),汇入异常,胆囊管炎症较重,管壁薄而脆弱,胆囊三角粘连较重无法分离出胆囊管等为LTCBDE的禁忌证。另外,由于胆囊管通常以锐角向下汇入胆总管,经胆囊管入路时胆道镜很难观察肝管及以上胆管,所以,术前必须通过MRCP等检查确定胆管内结石的位置。相较于LCBDE+胆道一期缝合术,LTCBDE更加突出对胆囊管的要求,其适应证相对严格,术前一定要加强检查,谨慎把握手术适应证。
3.2 两种术式术中情况和术后并发症的对比
比较两组患者的手术方式,LCBDE+一期缝合组所有患者均行胆总管切开,探查后再行一期缝合,与之相比,LTCBDE组直接经胆囊管置入胆道镜行胆总管探查的病例数为35例,剩余15例患者行汇合部微切开,探查后行汇合部缝合。所以,LTCBDE组大部分患者(70%)不需要行胆道切开及探查后的胆道缝合,而经汇合部切开的患者,虽然汇合部的缝合用时较长,但在熟练的腹腔镜操作技术下,并未延长总的手术时间。综合LTCBDE组的两部分患者,在手术操作上,LTCBDE对胆道的切开、缝合更少,对人体损伤更小,所以,LTCBDE组患者手术时间、术中出血、术后引流量、带管时间和住院时间均较LCBDE+一期缝合组明显减少,使治疗更加微创、有效,加速患者康复,提高患者生活质量。在术后并发症方面,两组患者术后胆道狭窄、胆管炎和胆道出血的发生都较少,没有明显差异。相比而言,胆汁漏还是胆总管探查的主要并发症[17]。LCBDE+一期缝合组共有7例患者出现术后胆汁漏,可能因为:⑴ 患者胆道炎症较重,管壁水肿或者管壁本身菲薄,缝合效果降低;⑵ 术中一期缝合时,反复加针,针距较密,打结用力过大,造成胆管壁切割。而LTCBDE组有1例患者出现术后胆汁漏,排除术中操作的原因后,笔者认为可能与患者肝功能不良,术后低蛋白有关。总结笔者经验,若患者胆管壁条件或全身情况不佳,不适合行LCBDE+胆道一期缝合术及LTCBDE,应及时改行腹腔镜下胆总管探查+T管引流术,避免术后胆汁漏的发生。对比两组患者,LTCBDE组术后胆汁漏的发生较LCBDE+一期缝合组明显减少,可见,LTCBDE在减少术后胆汁漏方面更具优势,主要因为[18]:⑴ 经胆囊管探查胆总管并取石,最大限度地避免了胆总管的损伤,保持了胆总管的完整性,从而减少与胆总管损伤直接相关的胆汁漏、狭窄、炎症的发生,加速患者康复;⑵ 术中取石完毕后,对于汇合部微切开取石的患者,由于在解剖上,胆囊与肝总管汇合时形成了一个膨大,从而为此处切开的胆总管行双层缝合创造了可能,即胆道黏膜连续缝合+胆道浆肌层间断缝合的双层缝合法。由于第二层缝合将第一层包埋,相当于对第一层缝合的加强和保护,当胆总管压力上升时,双层缝合有效地降低了胆汁漏的发生率而并不增加胆道狭窄的发生[19]。
综合两组患者术中情况及术后并发症的对比,LTCBDE较LCBDE+胆道一期缝合术效果更佳,如显著缩短手术时间,减少患者创伤,加快患者康复,减少术后并发症等。所以,当患者同时满足两种术式的适应证时,应优先选择LTCBDE,而LCBDE+胆道一期缝合术的适应证更为宽泛,操作相对简单,当LTCBDE因胆囊管解剖异常等原因操作失败时,LCBDE+胆道一期缝合术或放置T管引流可根据实际情况作为补救术式。
3.3 LTCBDE的手术技巧
总结研究经验和文献报道,笔者认为对胆道解剖结构的熟悉和对胆道变异高度的警惕是LTCBDE的核心,而术中仔细操作及娴熟的腹腔镜功底是手术成功的关键[20]。术者对胆道镜探查及网篮取石技术的熟练程度直接影响该术的成功率。手术中,因胆囊管本身直径小于胆总管,并且在胆总管梗阻,胆道扩张时,胆囊管扩张的程度也小于胆总管,所以LTCBDE成功的要点在于胆道镜能否经较细的胆囊管进入胆总管[21]。首先,术中充分解剖胆囊管,完全显露胆囊管全程直至汇合部,使扭曲的胆囊管变直,能更有效地扩张胆囊管,减小胆囊管汇入胆总管的角度,利于胆道镜的操作,还能看清胆囊管的走形,辨别有无胆囊管的变异,以决定下一步的手术方式。当胆道镜无法直接进入胆囊管时,可采用胆道探子、分离钳等扩张胆囊管[22],经网篮引导置入胆道镜,行胆囊管球囊扩张,使用超细胆道镜等方法[23]。如果以上操作仍无法置入胆道镜,则可以沿胆囊管向胆总管行汇合部微纵向切开3~5 mm[24],切口呈“T”形,缩短胆道镜走行路径、增加接触面。切开处顶端以4-0可吸收缝线间断缝合防止取石过程撕裂胆总管。当取石结束后,汇合部的切开行一期的双层缝合:先用4-0可吸收线连续缝合切开的胆总管、胆囊管黏膜层及螺旋瓣。再用5-0可吸收线行间断浆肌层缝合。缝合至距离汇入部5 mm以上时,用Hem-o-lok夹闭胆囊管。若术中怀疑左右肝管有结石,也应采用汇入部的微切开,以确保胆道镜能向上探查肝管,必要时可行经胆囊管造影来确保无结石残留。术后常规于小网膜孔防置腹腔负压引流3 d以上,以利于观察术后恢复情况和处理并发症。研究表明,持续的腹腔引流、术中轻柔、规范的操作和可靠的双层缝合能有效防治LTCBDE术后的胆汁漏、出血等[17,25]。
综上所述,LTCBDE是一种治疗胆总管结石的创新术式。它具有严格的适用范围,手术操作比LCBDE+胆道一期缝合术更加复杂,但其可根据患者的实际情况变换多种操作方式,技术可靠,对胆总管的损伤较小、术后恢复快、并发症少。所以,对于两者适应证均符合的患者,应优先选择LTCBDE。
参考文献
[1]Ahmed I,Pradhan C,Beckingham IJ,et al.Is a T-tube necessary after common bile duct exploration?[J].World J Surg,2008,32(7):1485–1488.doi: 10.1007/s00268–008–9475–2.
[2]van Dijk AH,Lamberts M,van Laarhoven CJ,et al.Laparoscopy in cholecysto-choledocholithiasis[J].Best Pract Res Clin Gastroenterol,2014,28(1):195–209.doi: 10.1016/j.bpg.2013.11.015.
[3]Bencini L,Tommasi C,Manetti R,et al.Modern approach to cholecysto-choledocholithiasis[J].World J Gastrointest Endosc,2014,6(2):32–40.doi: 10.4253/wjge.v6.i2.32.
[4]殷晓煜.胆道外科手术中Oddi括约肌保护的共识与争议[J].中国实用外科杂志,2015,35(1):46–48.Yin XY.Consensus and controversies on protection of sphincter of Oddi during biliary surgery[J].Chinese Journal of Practical Surgery,2015,35(1):46–48.
[5]Costi R,Gnocchi A,Di Mario F,et al.Diagnosis and management of choledocholithiasis in the golden age of imaging,endoscopy and laparoscopy[J].World J Gastroenterol,2014,20(37):13382–13401.doi: 10.3748/wjg.v20.i37.13382.
[6]Dasari BV,Tan CJ,Gurusamy KS,et al.Surgical versus endoscopic treatment of bile duct stones[J].Cochrane Database Syst Rev,2013,(9):CD003327.doi: 10.1002/14651858.CD003327.
[7]潘步建,徐迈宇,陈峰,等.腹腔镜下经胆囊管纤维胆道镜取石术治疗胆总管结石的临床研究[J].中华普通外科杂志,2015,30(6):485–486.doi:10.3760/cma.j.issn.1007–631X.2015.06.018.Pan BJ,Xu MY,Chen F,et al.Clinical study of laparoscopic transcystic duct stone extraction using fiber choledochoscope for common bile duct stones[J].Zhong Hua Pu Tong Wai Ke,2015,30(6):485–486.doi:10.3760/cma.j.issn.1007–631X.2015.06.018.
[8]吴胜,陈金锁,唐晓明,等.腹腔镜及选择性辅助小切口治疗胆囊结石合并肝外胆管结石的临床研究[J].重庆医学,2015,44(13):1807–1808.doi:10.3969/j.issn.1671–8348.2015.13.028.Wu S,Chen JS,Tang XM,et al.Study on laparoscopy and selective assisted small incision for treating cholecystolithiasis complicating extrahepatic bile duct stone[J].Chongqing Medicine,2015,44(13):1807–1808.doi:10.3969/j.issn.1671–8348.2015.13.028.
[9]陈学敏,杨春,孙冬林,等.腹腔镜指导下纤维胆道镜胆总管探查术的临床应用[J].中国普通外科杂志,2010,19(8):846–848.Chen XM,Yang C,Sun DL,et al.Clincal application of laparoscopic common bile duct exploration with fibercholedoscopy[J].Chinese Journal of General Surgery,2010,19(8):846–848.
[10]菅志远,沈先锋,黄林生,等.三种微创方式治疗胆囊结石合并胆总管结石的临床疗效分析[J].中国普通外科杂志,2015,24(2):275–279.doi:10.3978/j.issn.1005–6947.2015.02.023.Jian ZY,Shen XF,Huang LS,et al.Clinical therapeutic outcome of 3 different minimally invasive procedures for calculi of gallbladder associated with choledocholithiasis[J].Chinese Journal of General Surgery,2015,24(2):275–279.doi:10.3978/j.issn.1005–6947.2015.02.023.
[11]郭宝利,陶洪臣,李健,等.腹腔镜联合胆道镜胆总管切开取石并一期缝合胆总管治疗胆总管结石[J].医学临床研究,2010,27(12):2312–2313.doi:10.3969/j.issn.1671–7171.2010.12.052.Guo BL,Tao HC,Li J,et al.Common bile duct exploration with primary bile duct closure by combination use of laparoscope and choledochoscope for common bile duct stones[J].Journal of Clinical Research,2010,27(12):2312–2313.doi:10.3969/j.issn.1671–7171.2010.12.052.
[12]EI-Geidie AA.Is the use of T-tube necessary after laparoscopic choledochotomy?[J].J Gastrointest Surg,2010,14(5):844–848.doi:10.1007/s11605–009–1133–y.
[13]张雷达,别平,陈平,等.腹腔镜胆道探查术后胆管一期缝合与T管引流的疗效比较[J].中华外科杂志,2004,42(9):520–523.doi:10.3760/j:issn:0529–5815.2004.09.003.Zhang LD,Bie P,Chen P,et al.Primary duct closure versus T-tube drainage following laparoscopic choledochotomy[J].Chinese Journal of Surgery,2004,42(9):520–523.doi:10.3760/j:issn:0529–5815.2004.09.003.
[14]Lyass S,Phillips EH.Laparoscopic transcystic duct common bile duct exploration[J].Surg Endosc,2006,20( Supple 2):441–445.
[15]王博,程洁,袁志林,等.两种微创方法治疗胆囊结石合并胆总管结石的疗效比较[J].腹腔镜外科杂志,2010,15(5):379–381.doi:10.3969/j.issn.1009–6612.2010.05.025.Wang B,Cheng H,Yuan ZL,et al.Comparison of the therapeutic effect of two methods of minimally invasive treatment for cholecystolithiasis combined with choledocholithiasis[J].Journal of Laparoscopic Surgery,2010,15(5):379–381.doi:10.3969/j.issn.1009–6612.2010.05.025.
[16]尚培中,周凤桐,贾国洪,等.胆道镜经胆囊管行胆道探查147例[J].人民军医,2007,50(6):345–346.doi:10.3969/j.issn.1000–9736.2007.06.019.Shang PZ,Zhou FT,Jia GH,et al.Choledochoscopic transcystic duct bile tract exploration: a report of 147 cases[J].People's Military Surgeon,2007,50(6):345–346.doi:10.3969/j.issn.1000–9736.2007.06.019.
[17]李宇,仵正,姚英民,等.腹腔镜经胆囊管胆总管探查取石术的临床应用?[J].中国微创外科杂志,2016,16(1):47–49.doi:10.3969/j.issn.1009–6604.2016.01.013.Li Y,Wu Z,Yao YM,et al.Laparoscopic Trans-cystic Bile Duct Exploration in the Management of Choledocholithiasis[J].Chinese Journal of Minimally Invasive Surgery,2016,16(1):47–49.doi:10.3969/j.issn.1009–6604.2016.01.013.
[18]Zhu QD,Tao CL,Zhou MT,et al.Primary closure versus Ttube drainage after common bile duct exploration for choledocholithiasis[J].Langenbecks Arch Surg,2011,396(1):53–62.doi: 10.1007/s00423–010–0660–z.
[19]屠政斌,袁建毛.经胆囊管汇入部微切开与胆总管一期缝合在腹腔镜胆总管探查术中的应用比较[J].肝胆胰外科杂志,2015,27(5):402–405.doi:10.11952/j.issn.1007–1954.2015.05.015.Tu ZB,Yuan JM.Comparison of using mini-incision at the confluence of CBD and cystic duct and primary closure in laparoscopic common bile duct exproration[J].Journal of Hepatopancreatobiliary Surgery,2015,27(5):402–405.doi:10.11952/j.issn.1007–1954.2015.05.015.
[20]方路,邹书兵,王开阳,等.腹腔镜下联合胆道镜经胆囊管胆总管取石术的应用: 附82 例报告[J].中国普通外科杂志,2011,20(3):279–281.Fang L,Zou SB,Wang KY,et al.Combined laparoscopic and duodenoscopic transcystic duct for common bile duct stone extraction[J].Chinese Journal of General Surgery,2011,20(3):279–281.
[21]Chen XM,Zhang Y,Cai HH,et al.Transcystic approach with micro-incision of the cystic duct and its confluence part in laparoscopic common bile duct exploration[J].J Laparoendosc Adv Surg Tech A,2013,23(12):977–981.doi: 10.1089/lap.2013.0309.
[22]周永平,郭子健,戴途,等.腹腔镜下经胆囊管胆总管探查取石术的疗效分析[J].中国临床医学,2013,20(3):294–296.doi:10.3969/j.issn.1008–6358.2013.03.016.Zhou YP,Guo ZJ,Dai T,et al.Curative Effects of Laparoscopic Transcystic Common Bile Duct Exploration[J].Chinese Journal of Clinical Medicine,2013,20(3):294–296.doi:10.3969/j.issn.1008–6358.2013.03.016.
[23]Zhu JG,Han W,Zhang ZT,et al.Short-term outcomes of laparoscopic transcystic common bile duct exploration with discharge less than 24 hours[J].J Laparoendosc Adv Surg Tech A,2014,24(5):302–305.doi: 10.1089/lap.2013.0537.
[24]韩威,张忠涛,李建设,等.胆囊管汇入部微切开在腹腔镜胆道探查术中的应用[J].中国微创外科杂志,2011,11(11):970–972.doi:10.3969/j.issn.1009–6604.2011.11.004.Han W,Zhang ZT,Li JS,et al.Transcystic Approach with Micro-incision of the Cystic Duct and its Confluence Part in Laparoscopic Common Bile Duct Exploration[J].Chinese Journal of Minimally Invasive Surgery,2011,11(11):970–972.doi:10.3969/j.issn.1009–6604.2011.11.004.
[25]陈小勋,李强辉,张兆明,等.微创治疗胆总管结石的术式选择[J].中国普通外科杂志,2010,19(10):1135–1138.Chen XX,Li QH,Zhang ZM,et al.Minimally invasive surgical treatment of common bile duct stones[J].Chinese Journal of General Surgery,2010,19(10):1135–1138.