腹腔镜胆囊切除术(LC)自1986年首次应用,为越来越多的医生和患者所接受,成为治疗胆囊结石等胆囊良性疾病的金标准[1-3],LC相对于开腹胆囊切除术(open cholecystectomy,OC)具有创伤小、疼痛小、术后恢复快等优势。但因胆囊疾病复杂,镜下处理困难时,需中转开腹确保手术全完成[4]。本研究通过对我院近6年来LC中转开腹手术患者中转开腹率、中转开腹的原因及时期等临床资料分析,以指导术中干预。
1 资料与方法
1.1 一般资料
我院2010年1月—2015年12月收治3 849例拟行LC患者,男1 422例,女2 427例,中转开腹39例,其中男28例,女11例。纳入标准:⑴ B超确诊为胆囊结石或胆囊炎;⑵ 胆囊病变直径>10 mm,且近期出现增大,伴有或无手术指征的良性炎性病变,例如胆固醇性息肉、腺瘤或是有症状的炎性息肉。排除标准:同时需要其他组织或是器官切除术的。
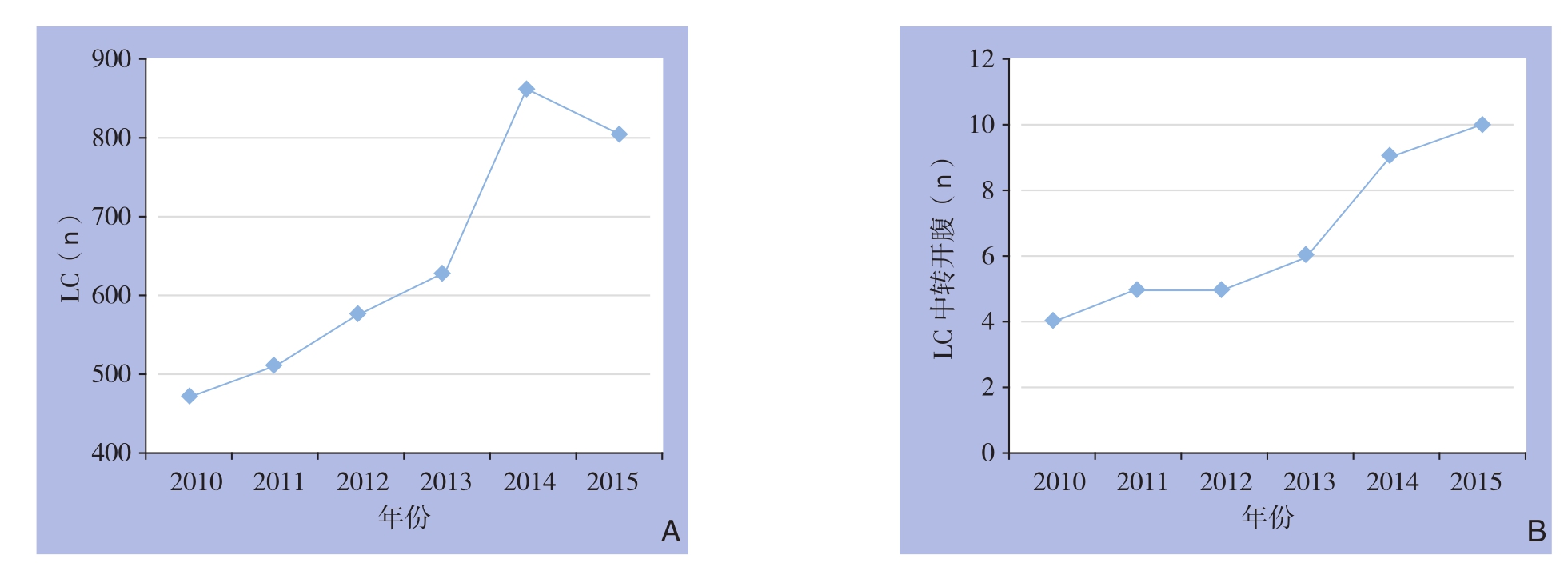
图1 2010—2015年LC例数、中转开腹例数变化趋势 A: LC;B: LC中转开腹
Figure 1 Changing tendency in number of LC and open conversion from 2010 to 2015 A: LC; B: Open conversion of LC
1.2 手术方法
均在全麻下行LC,采用常规三孔法或四孔法进行操作,如出现镜下无法处理的情况,即中转开腹;中转开腹取右肋缘下斜切口,切除胆囊,术后均送检行病理学检查以证实诊断。
1.3 观察指标
术前:性别、年龄、病程;术中:中转开腹原因、中转开腹的时机及中转开腹率、手术主刀医生职称;术后:诊断、术后并发症及随访。
1.4 统计学处理
采用SPSS 22.0统计软件对收集的数据进行分析,计量资料以均数±标准差![]() 表示,不同组别比较用χ2检验,P<0.05为差异有统计学意义。
表示,不同组别比较用χ2检验,P<0.05为差异有统计学意义。
2 结 果
2.1 LC中转开腹率
3 8 4 9例L C中,中转开腹3 9例,中转率1.01%。2010—2015年LC例数、中转开腹例数变化趋势见图1;各年度LC中转率差异无统计学意义(P=0.982)(表1)。
表1 2010—2015年LC中转率比较
Table 1 comparison among the rate of conversion from 2010 to 2015
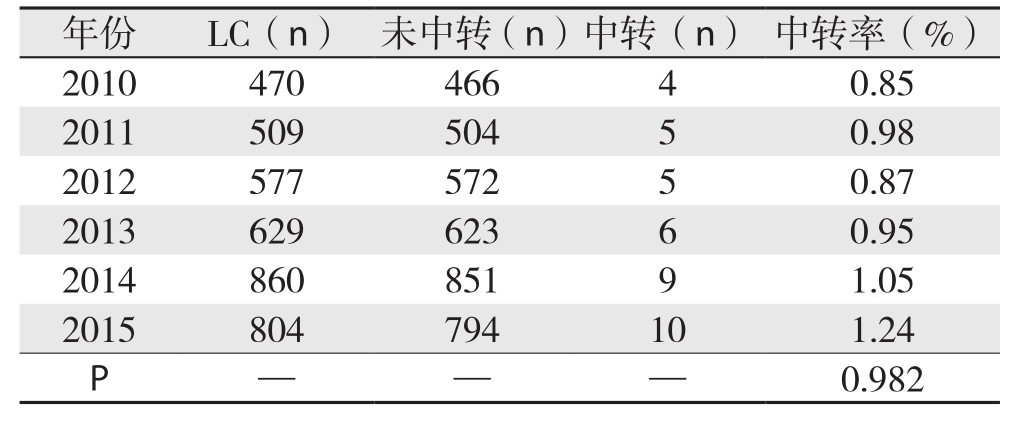
年份 LC(n) 未中转(n)中转(n) 中转率(%)2010 470 466 4 0.85 2011 509 504 5 0.98 2012 577 572 5 0.87 2013 629 623 6 0.95 2014 860 851 9 1.05 2015 804 794 10 1.24 P— —0.982
2.2 LC中转开腹原因
中转开腹的原因包括胆囊三角解剖困难(16例),腹腔、胆囊粘连致密(14例)(包括胆囊周围底部、体部粘连致密、胆囊颈部与十二指肠粘连紧密、腹腔粘连严重或胆囊包埋),Mirrizi综合征(3例)、胆囊动脉出血(2例),胆汁漏、胆总管损伤、胆囊十二指肠瘘、胆囊癌(各1例)(表2)。
表2 中转开腹原因
Table 2 Reasons for open conversion

原因 n(%)胆囊三角解剖困难 16(41.0)腹腔、胆囊周围粘连严重 14(35.9)胆囊周围(底体部)粘连致密 5(12.8)胆囊颈部与十二指肠粘连致密 4(10.3)腹腔粘连严重或广泛 3(7.7)胆囊包埋(未现) 2(5.1)Mirrizi综合征 3(7.7)胆囊动脉出血 2(5.1)胆汁漏 1(2.6)胆总管损伤 1(2.6)胆囊十二指肠内瘘 1(2.6)疑胆囊癌 1(2.6)合计 39(100.0)
2.3 早期、中晚期中转开腹并发症
本研究将中转开腹的时机分为早期(进入腹腔、显露胆囊)、中期(胆囊蒂解剖)、晚期(胆囊切除)。早期中转开腹33例,中期中转开腹5例,晚期中转开腹1例;中期4例因发生并发症(2例胆囊动脉出血、1例胆囊破裂导致胆囊三角结构不清,1例胆总管损伤)而中转开腹,晚期1例因发生胆汁漏而中转开腹,而早期中转开腹33例均非并发症原因,两者差异有统计学意义(P<0.001)(表3)。
表3 并发症原因所致的中转开腹在不同时期中转患者间的比较[n(%)]
Table 3 Comparison of the complication-caused open conversions between patients undergoing conversion at different stages [n (%)]
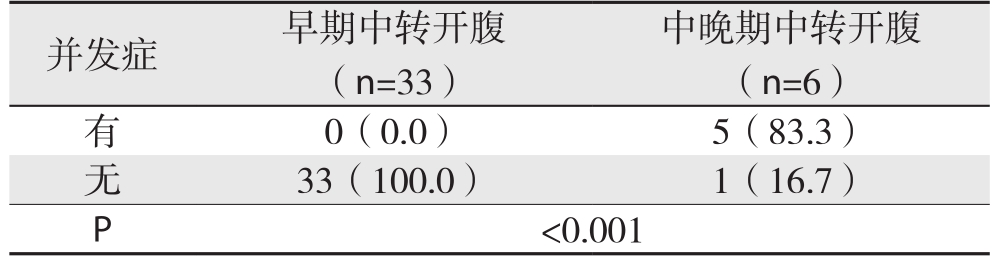
并发症 早期中转开腹(n=33)中晚期中转开腹(n=6)有0(0.0) 5(83.3)无33(100.0) 1(16.7)P<0.001
2.4 LC中转开腹相关危险因素
中转开腹39例中,男28例,女11例,两者差异有统计学意义(P<0.001);年龄(28~82岁),平均(54.8±10.6)岁,其中年龄≥50岁 27例,年龄<5 0岁1 2例,两者差异有统计学意义(P=0.0 0 7);病程3 h至2 0年,平均(2.8 3±0.7 3)年,其中病程>1个月2 6例,病程≤1个月1 3例),两者差异有统计学意义(P=0.006)(表4)。
表4 中转开腹相关危险因素分析[n(%)]
Table 4 Analysis of risks for open conversion [n (%)]
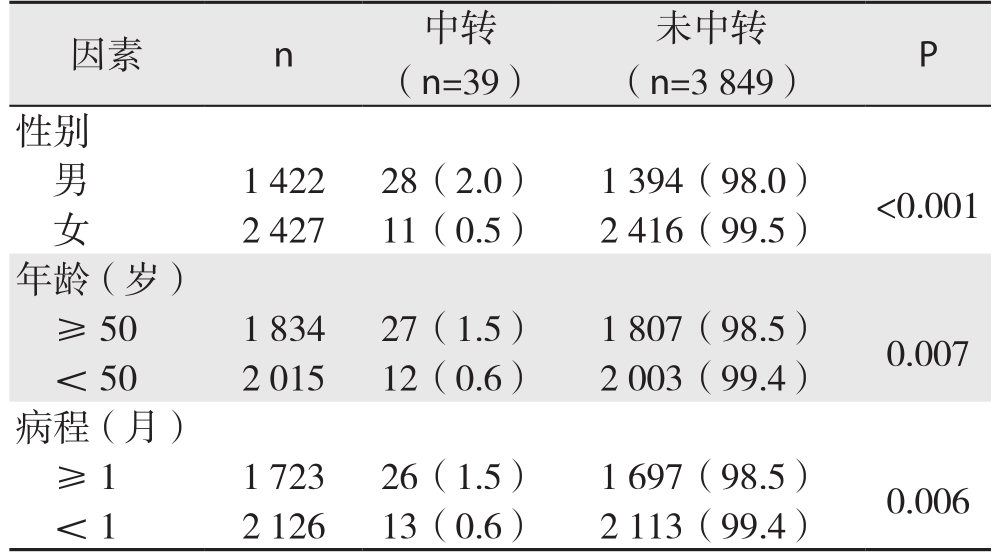
因素 n 中转(n=39)未中转(n=3 849) P性别男 1 422 28(2.0) 1 394(98.0) <0.001女 2 427 11(0.5) 2 416(99.5)年龄(岁)≥50 1 834 27(1.5) 1 807(98.5) 0.007< 50 2 015 12(0.6) 2 003(99.4)病程(月)≥1 1 723 26(1.5) 1 697(98.5) 0.006< 1 2 126 13(0.6) 2 113(99.4)
2.5 诊断及合并症
中转开腹39例中,诊断主要为胆囊结石并慢性胆囊炎14例,胆囊结石并急性胆囊炎或慢性胆囊炎急性发作11例,胆囊结石并急性坏疽性胆囊炎5例),胆囊结石并急性化脓性胆囊炎3例,Mirrizi综合征3例,胆囊息肉2例,胆囊癌(1例,术前B超考虑胆囊息肉)。合并胆囊颈部或壶腹部结石15例(术中证实),合并胆源性胰腺炎4例,合并糖尿病、高血压、冠心病等基础疾病13例(表5)。
表5 诊断及合并疾病
Table 5 Diagnosis and concomitant disease
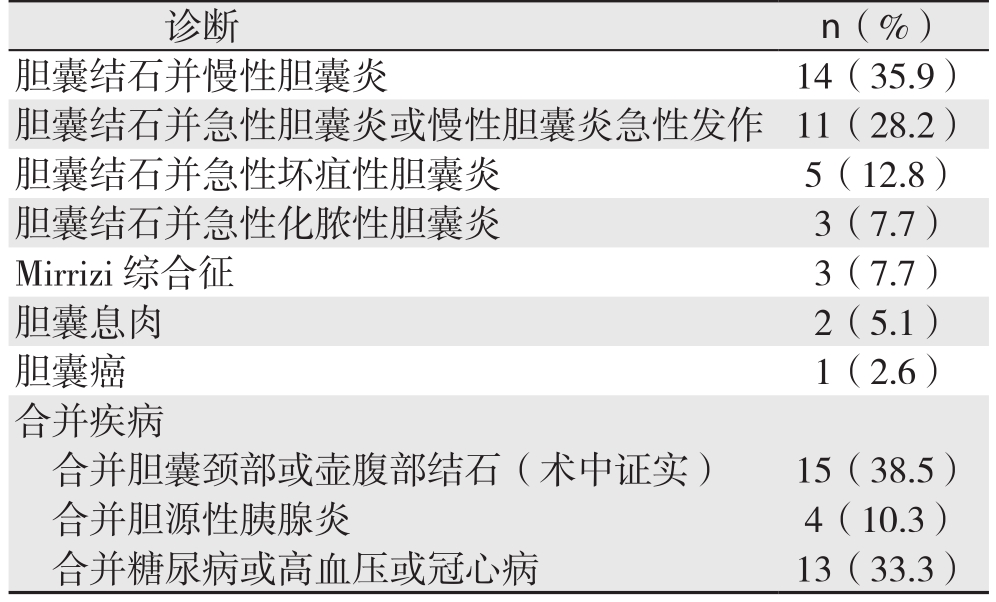
诊断 n(%)胆囊结石并慢性胆囊炎 14(35.9)胆囊结石并急性胆囊炎或慢性胆囊炎急性发作 11(28.2)胆囊结石并急性坏疽性胆囊炎 5(12.8)胆囊结石并急性化脓性胆囊炎 3(7.7)Mirrizi综合征 3(7.7)胆囊息肉 2(5.1)胆囊癌 1(2.6)合并疾病合并胆囊颈部或壶腹部结石(术中证实) 15(38.5)合并胆源性胰腺炎 4(10.3)合并糖尿病或高血压或冠心病 13(33.3)
2.6 不同技术职称术者中转开腹近期并发症
术后近期(住院期间)并发症8例,胆囊窝积液5例,胆汁漏1例,不完全性小肠梗阻1例,肠瘘1例。中转开腹39例中,主治医生术者9例(胆囊窝积液4例),副教授术者22例(1例胆囊窝积液+1例不完全性肠梗阻+1例肠瘘),教授术者8例(1例胆汁漏)(表6),不同技术职称中转开腹近期并发症发生率差异有统计学意义(P=0.043)。
表6 不同技术职称术者实施的中转开腹近期并发症发生率比较[n(%)]
Table 6 Comparison of incidence of short-term postoperative complications of open conversion performed by surgeons of different technical titles [n (%)]
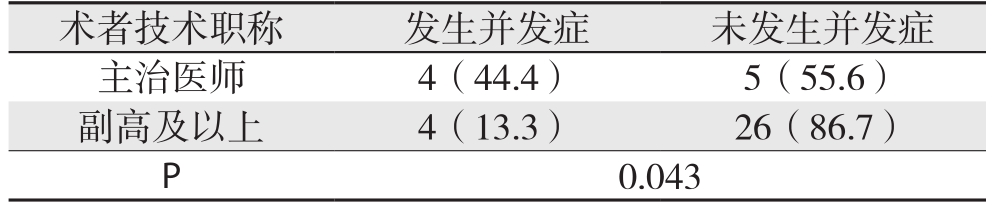
术者技术职称 发生并发症 未发生并发症主治医师 4(44.4) 5(55.6)副高及以上 4(13.3) 26(86.7)P 0.043
2.7 随访
采取电话、微信等方式随访26例,随访率66.7%,随访时间为3个月至5年。有复查者13例,患者复查率33.3%,其中在术后1~3个月内复查1次11例,2例在术后1年后复查1次。远期并发症6例,发生率15.4%,其中右上腹、腹胀痛不适2例,长期腹泻3例,1例于术后3年因肺癌死亡。
3 讨 论
3.1 对中转开腹及中转开腹率的认识
国内外对LC的中转率报道差异较大,可能与LC操作、患者病情及术者技术水平与经验等诸多因素相关。LC中转开腹发生率为1.04%~10.71%[4-7]。我院LC中转率为1.01%,与相关报道基本接近。本研究发现2010—2015年随着年份的增加,行LC、中转开腹的数量都在增加,但近6年中转开腹率维持在一个相对稳定的水平。其原因可能:LC术广泛开展、手术适应证拓宽、复杂病例数的增加(如胆囊急性炎症期如化脓性或坏疽性胆囊炎、Mirrizi综合征、胆囊颈部结石嵌顿等胆道复杂情况及合并胰腺炎发作或糖尿病、高血压、冠心病等基础疾病)使LC例数、中转开腹例数的增加,而我院术者的经验、技术水平提高及手术设备更新等使中转开腹率维持在相对稳定的水平。中转开腹手术不是手术并发症,也不是手术失败,而是手术方式的改变,是预防血管、脏器、胆道损伤等严重并发症的明智选择[8]。因此,LC并不能完全替代的OC地位,OC始终是LC的坚强后盾[9]。
3.2 中转开腹的原因
3.2.1 胆囊三角解剖结构不清 本组中胆囊三角解剖结构不清、难以辨认造成胆囊三角处理困难占41.0%,是中转开腹的最主要的原因。胆囊三角是LC主要目标区域,解剖分离胆囊三角区以达到安全切除胆囊的手术目的。Yajima等[10]指出因胆囊三角粘连严重、处理困难而被迫中转开腹率占51.1%,而提出如果胆囊三角处理困难应当中转开腹以确保手术安全,有的中心比例甚至高达占61.9%[11]。急性胆囊炎三角区组织炎症渗出、充血水肿严重,解剖时容易出血,造成手术视野模糊;慢性胆囊炎反复发作,三角区炎症浸润,致组织纤维化,甚至呈“冰冻样”粘连[12];或胆囊与大网膜、肠管粘连严重,胆囊三角区无间隙粘连,无法显露胆囊三角之间的关系。本组的经验是术中对于胆囊三角结构不清或处理困难的,立即中转开腹,操作时可采取逆行切除、钝性分离相结合的方式,以确保手术安全完成。
3.2.2 腹腔、胆囊周围粘连严重 本组中腹腔、胆囊周围粘连严重占35.9%,是中转开腹的第二大原因。游离暴露胆囊与周围组织的粘连是LC的重要步骤。粘连可导致手术时间延长,使出血和胆囊破裂等危险增加,因而有学者[12-13]提出当镜下探查腹腔有致密粘连或胆囊周围粘连严重,中转开腹应该是首选的治疗方案。粘连主要包括:⑴ 胆囊与周围组织脏器织粘连致密(5例),胆囊急性炎症发作胆囊周围粘连包裹;慢性胆囊炎反复发作,胆囊周围粘连致密,最终导致纤维化[14],使胆囊与周围组织界限不清。⑵ 胆囊颈部与十二指肠粘连致密(4例),强行分离容易损伤十二指肠;本组中1例十二指肠半包裹胆囊颈部,无法游离,强行游离极有可能损伤十二指肠,遂中转开腹;3例胆囊与十二指肠壁有粘连无法分离,切除大部分胆囊壁,残留少许无法分离粘连十二指肠的胆囊壁。⑶ 腹腔粘连广泛、严重(3例)或胆囊包埋(2例),多与炎症反应有关,如慢性胆囊炎反复发作,合并胰腺炎发作或糖尿病、上腹部手术史等。炎症渗出引起腹腔内脏器之间以、脏器与腹壁发生严重粘连,影响胆囊、三角区的暴露、分离及正常气腹的建立。本组腹腔粘连严重,气腹下视野狭小,试行分离后仍难以达到暴露胆囊的目标,遂中转开腹。
3.2.3 Mirizzi综合征 研究[15-17]显示Mirrizi综合征的发生率0.3%~1.21%。Mirizzi综合征合并局部结石梗阻就足以引起慢性炎症[14],尤其是胆囊颈部结石嵌顿,慢性胆囊炎合并Mirrizi综合征,一般病程较长(本组病程3年2例,10年1例),长期炎症反复发作形成冰冻样粘连(2例),甚至形成胆囊-胆总管瘘(1例),造成胆囊三角无法解剖。急性胆囊炎合并Mirrizi综合征,胆囊周围容易形成冰冻三角[18]。LC在Mirrizi综合征中技术上具有挑战性,使胆管损伤的风险增加。及时中转开腹,采取逆行+顺行切除胆囊,可依次结扎胆囊动脉后、胆囊管,明确三角关系,再行胆道探查术。
3.2.4 胆囊动脉出血 LC因出血中转开腹的发生率0%~1.9%[10],最主要为胆囊动脉出血,胆囊动脉是LC或传统胆囊切除术中分离、结扎的关键组织结构[19-20],在寻找、分离、及结扎胆囊动脉常伴随出血等并发症,术中出血量的多少与腔镜手术难易程度、顺利与否密切相关。本组2例均为分离胆囊三角时胆囊动脉出血,出血量分别1 000、1 300mL。1例出血较多,手术视野模糊,腹腔镜下难以继续操作完成手术,1例为镜下无法钳夹止血立即中转开腹。因镜下视野的局限,且胆囊动脉常有变异,(自肝固有动脉或其左支、胃十二指肠动脉或具有双胆囊动脉),这些变异的动脉有时会被忽视而误伤出血。胆囊动脉处理不当容易造成大出血,所以应当熟悉这种胆囊动脉起源及走形等解剖异常,术中精细操作,如胆囊动脉出血过多,镜下难以有效及时止血时应立即中转开腹以确保手术安全。
3.2.5 胆汁漏 术中发现胆汁漏应立即予以修复[21]。本组1例,切除胆囊后,发现有胆汁外漏,镜下无法探查到胆汁外漏处,遂中转开腹发现胆囊床处有胆汁外漏,予以压迫缝扎,将干净白纱垫放置于手术创面5 min后取出,观察敷料是否黄染,按此方法确认无胆汁泄露后关腹。术中胆汁漏患者,术后尽早予以营养支持、保持引流管通畅。
3.2.6 胆管损伤 胆管损伤是LC较为严重的并发症,发生率较开腹手术时代明显上升并维持在一定水平,发生率为0.25%~0.5%[22-25],主要与胆囊三角结构辨认不清、术者的经验水平和局部解剖异常密切相关[26]。本组1例,镜下向胆总管分离时,胆管出血,进一步探查发现胆总管右侧壁有一小破口,立即中转开腹,予以胆道探查+T管引流。因此,分离胆囊三角时应尽可能明确结构、操作精细、钝性分离,避免过多的使用电凝,如果一旦明确胆管损伤,应立即中转开腹。
3.2.7 胆囊十二指肠内瘘 胆囊十二指肠内瘘在胆囊结石患者中发病率为0.3%~5.0%[27]。发生机制[28-29]是胆囊壁在结石长期、持续、反复的刺激下,血运循环障碍,局部黏膜、浆膜慢性坏死;十二指肠粘连包裹胆囊后,胆囊局部渗液的消化,形成内瘘穿透胆囊壁。本组例1例,病程7年余,复查CT不排除胆囊十二指肠球部瘘可能,术中证实胆囊十二指肠内瘘,立即中转开腹,修补十二指肠瘘口。术前检查怀疑胆囊内瘘可能的患者,术前应充分评估相关风险及中转开腹的可能性,术中一旦怀疑胆肠内瘘应立即中转开腹以确保手术安全。
3.2.8 胆囊癌 随着LC的开展,意外胆囊癌发生率不断上升,约0.19%~2.8%[30-35]。LC术中如胆囊疑有恶变,应立即中转开腹根治手术以期获得较好预后[33-36]。LC治疗胆囊癌困境在于腔镜下肿瘤细胞腹腔播散率、切口种植率高及能否达到根治切除[37]。本组1例,62岁,术前B超考虑胆囊息肉,1个月内复查B超发现息肉明显增大,腔镜下见壶腹部一大小2cm×2cm质硬肿块,怀疑胆囊癌变,立即予以中转开腹行胆囊切除术。术中快速病检提示腺瘤样增生,不典型性改变,待石蜡切片待删癌,未做根治处理,术后病理检查示胆囊中分化腺癌,于术后11 d再次行胆囊癌根治术。术中冷冻切片的信息不全面,术中切开胆囊进行认真的视诊和触诊,对于及时发现术中胆囊癌非常重要[38]。此例术中快速未确诊癌,致术后二次开腹手术。所以,对此类病例术者应提高对术中胆囊病变的认识,重视术中剖视标本,注意观察黏膜面及触摸胆囊壁,准确行快速切片检查,在术中将怀疑的胆囊癌达到确诊,以期在同次手术中达到相应的根治术,改善胆囊癌的预后[39]。
3.3 中转开腹的时机
有学者[10]指出胆囊三角如果在30 min内无法游离暴露,LC术与中转开腹胆囊切除术在手术时间上基本没有差异,此种情况下,应当中转开腹,且尽早中转开腹可减少手术总时间和并发症的发生率。有学者[40]把LC分为4个步骤:进入腹腔、显露胆囊、胆囊蒂解剖、胆囊切除;每个步骤分别赋予0、1、2、3不同分值,然后相加,分值越大,难度系数越高。随着手术的进程,手术风险增加。据此,本研究将中转开腹的时机分为早期(进入腹腔、显露胆囊)、中期(胆囊蒂解剖)、晚期(胆囊切除)。本组中1例胆囊破裂导致胆囊三角结构不清,1例胆总管损伤,2例胆囊动脉出血,1例胆汁外漏等并发症均发生在中晚期开腹,早期中转开腹未见并发症。因此,若术中发现胆囊三角处理困难或腹腔、胆囊周围解剖结构不清或术者犹豫不觉无法保证继续安全完成LC时应当立即中转开腹,即在早期中转开腹,有助于预防胆道损伤、出血等严重并发症的发生,确保手术安全完成。这也为相关文献论述[31]所支持,其认为在腹腔镜下处理困难时尽早、低门槛采取中转开腹能够避免危及生命的并发症。LC手术强调的是手术的安全性和预防并发症,而不是手术的完成[1,10,41]。在严重的并发症发生之前尽早中转开腹,单纯的追求LC成功率造成严重的并发症时再被迫中转手术,就失去了LC的价值。
3.4 其他
国内外的学者[1,6,13,42-45]将男性、年龄作为LC中转开腹的危险因素。本组研究中,男性、年龄>50岁、病程>1个月为LC中转开腹的危险因素。男性患者中转开腹率比女性患者较高的原因可能与男性患者胆囊结石病史较长,较少关注自身健康状况,且常于胆囊炎症或其他较重的情况时才入院诊治有关。年龄较大患者一般有较长的胆囊结石病史,炎症反复发作,且老年患者长期胆囊炎反复发作致粘连更重,急性发病时病情严重,容易发生化脓、坏疽及穿孔。
3.5 中转开腹并发症
中转开腹术后有一定的并发症,主要包括:不完全性肠梗阻、胆汁漏、胆囊窝积液、肠瘘。不完全性肠梗阻等予以对症处理后恢复正常。胆汁漏治疗的关键是充分引流[46],本组胆汁漏、胆囊窝积液均予以延长腹腔引流管留置时间等对症处理后恢复顺利。肠瘘患者予以再次开腹手术行肠穿孔修补空肠造瘘术。副高及以上职称术者中转开腹近期并发症发生率较低,手术经验水平是LC中转的独立影响因素[47]。笔者认为应加强对年轻医师的指导、培训和锻炼,提升技术水平,中转开腹及手术并发症会逐渐减少 。
3.6 随访
本组随访中远期并发症6例,其中右上腹、腹胀痛不适2例,长期腹泻3例,1例于术后3年因肺癌死亡。手术区域粘连可引起右上腹不适,而胆囊切除以后胆汁不停的向肠内流入致结肠内胆汁酸浓度增高可引起长期腹泻。本组复查13例,占33.3%,复查率偏低,患者术后复查的依从性较差,可能与患者本身术后复查意识不强、复查依从性较差、复查不方便等有关。因此,建立定期主动随访,及时将随诊资料统计分析反馈到临床的一套完整、可行的术后随访制度,对患者诊疗是非常有意义的。
LC中转开腹是手术方式的转变,是确保手术安全的明智选择,有一定的中转率是正常的,术前充分评估中转开腹潜在原因,根据术中情况选择早期中转开腹,及时处理并发症及完善随访制度,才能给医患带来最大的获益。
参考文献
[1]Tosun A,Hancerliogullari K O,Serifoglu I,et al.Role of preoperative sonography in predicting conversion from laparoscopic cholecystectomy to open surgery[J].Eur J Radiol,2015,84(3):346–349.doi: 10.1016/j.ejrad.2014.12.006.
[2]Ansaloni L,Pisano M,Coccolini F,et al.2016 WSES guidelines on acute calculous cholecystitis[J].World J Emerg Surg,2016,11:25.doi: 10.1186/s13017–016–0082–5.
[3]Coccolini F,Catena F,Pisano M,et al.Open versus laparoscopic cholecystectomy in acute cholecystitis.Systematic review and meta-analysis[J].Int J Surg,2015,18:196–204.doi: 10.1016/j.ijsu.2015.04.083.
[4]Goonawardena J,Gunnarsson R,de Costa A,et al.Predicting conversion from laparoscopic to open cholecystectomy presented as a probability nomogram based on preoperative patient risk factors[J].Am J Surg,2015,210(3):492–500.doi: 10.1016/j.amjsurg.2015.04.003.
[5]姚青勋,范华英,向丽娜,等.腹腔镜中转开腹胆囊切除术临床分析[J].肝胆外科杂志,2015,23(3):194–196.Yao QX,Fan HY,Xiang LN,et al.Clinical analysis of 87 cases converted to open surgery during laparoscopic cholecystectomy[J].Journal of Hepatobiliary Surgery,2015,23(3):194–196.
[6]Licciardello A,Arena M,Nicosia A,et al.Preoperative risk factors for conversion from laparoscopic to open cholecystectomy[J].Eur Rev Med Pharmacol Sci,2014,18(2 Suppl):60–68.
[7]Goonawardena J,Gunnarsson R,de Costa A,et al.Predicting conversion from laparoscopic to open cholecystectomy presented as a probability nomogram based on preoperative patient risk factors[J].Am J Surg,2015,210(3):492–500.doi: 10.1016/j.amjsurg.2015.04.003.
[8]Beksac K,Turhan N,Karaagaoglu E,et al.Risk Factors for Conversion of Laparoscopic Cholecystectomy to Open Surgery: A New Predictive Statistical Model[J].J Laparoendosc Adv Surg Tech A,2016,26(9):693–696.doi: 10.1089/lap.2016.0008.
[9]吴品飞,刘杰凡,顾勇劲,等.腹腔镜胆囊切除术中转开腹200例危险因素分析[J].肝胆胰外科杂志,2016,28(4):329–331.doi:10.11952/j.issn.1007–1954.2016.04.019.Wu PF,Liu JF,Gu YJ,et al.Risk factors for conversion of laparoscopic to open cholecystectomy: analysis of 200 cases[J].Journal of Hepatopancreatobiliary Surgery,2016,28(4):329–331.doi:10.11952/j.issn.1007–1954.2016.04.019.
[10]卢铁成,周天民,房莉,等.腹腔镜胆囊切除术中转开腹相关因素分析[J].中国普外基础与临床杂志,2016,23(1):97–99.Lu TC,Zhou TM,Fang L,et al.Analysis of the relevant factors for conversion of laparoscopic to open cholecystectomy[J].Chinese Journal of Bases and Clinics In General Surgery,2016,23(1):97–99.
[11]Yajima H,Kanai H,Son K,et al.Reasons and risk factors for intraoperative conversion from laparoscopic to open cholecystectomy[J].Surg Today,2014,44(1):80–83.doi: 10.1007/s00595–012–0465–5.
[12]刘学礼,程平,刘安成,等.腹腔镜胆囊切除术中转开腹手术105例临床分析[J].肝胆外科杂志,2015,23(1):32–33.Liu XL,Cheng P,Liu AC,et al.The Analysis of conversion to open cholecystectomy undergoing laparoscopic cholecystectomy[J].Journal of Hepatobiliary Surgery,2015,23(1):32–33.
[13]Cwik G,Skoczylas T,Wyroślak-Najs J,et al.The value of percutaneous ultrasound in predicting conversion from laparoscopic to open cholecystectomy due to acute cholecystitis[J].Surgical Endoscopy,2013,27(7):2561–2568.doi: 10.1007/s00464–013–2787–9.
[14]Goh YL,Toumi Z,Mok KW,et al.Variation in conversion rates of laparoscopic cholecystectomy in different set-ups can be explained on the basis of C-reactive protein (CRP) values at index admission[J].Int J Surg,2015,15:38–39.doi: 10.1016/j.ijsu.2015.01.017.
[15]Su LS,Burke LH,Ertl CW.Conversion of laparoscopic cholecystectomy to open surgical procedure due to complete fi brosis of the gallbladder[J].BMJ Case Rep,2013,pii: bcr2013009406.doi: 10.1136/bcr–2013–009406.
[16]Kulkarni SS,Hotta M,Sher L,et al.Complicated gallstone disease:diagnosis and management of Mirizzi syndrome[J].Surg Endosc,2016.[Epub ahead of print]
[17]Nagorni EA,Kouklakis G,Tsaroucha A,et al.Post-laparoscopic cholecystectomy Mirizzi syndrome induced by polymeric surgical clips: a case report and review of the literature[J].J Med Case Rep,2016,10:135.doi: 10.1186/s13256–016–0932–5.
[18]Yetisir F,Sarer AE,Acar HZ,et al.Laparoscopic Treatment of Type III Mirizzi Syndrome by T-Tube Drainage[J].Case Rep Surg,2016,2016:1030358.doi: 10.1155/2016/1030358.
[19]冯一浮,莫经刚,陈建辉.急性胆囊炎腹腔镜胆囊切除术中转开腹相关风险因素的分析[J].中国普通外科杂志,2016,25(2):286–290.doi:10.3978/j.issn.1005–6947.2016.02.022.Feng YF,Mo JG,Chen JH.Analysis of factors related to conversion from laparoscopic cholecystectomy to laparotomy for acute cholecystitis[J].Chinese Journal of General Surgery,2016,25(2):286–290.doi:10.3978/j.issn.1005–6947.2016.02.022.
[20]Dandekar U,Dandekar K.Cystic Artery: Morphological Study and Surgical Signi fi cance[J].Anat Res Int,2016,2016:7201858.
[21]李建刚,王俊,李亮.探讨腹腔镜胆囊切除术中转开腹在临床中的情况[J].世界最新医学信息文摘:连续型电子期刊,2016,16(4):160–161.Li JG,Wang J,Li L.Conversion of laparoscopic to open cholecystectomy in clinical settings[J].World Latest Medicine Information,2016,16(4):160-161.
[22]Liu D,Cao F,Liu J,et al.Risk factors for bile leakage after primary closure following laparoscopic common bile duct exploration:a retrospective cohort study[J].BMC Surg,2017,17(1):1.doi:10.1186/s12893–016–0201–y.
[23]寇桂香,柴琛.医源性胆管损伤的临床诊治进展[J].中国普外基础与临床杂志,2014,21(10):1321–1324.Kou GX,Cai C.Advances in Clinical Diagnosis and Treatment of Iatrogenic Bile Duct Injury[J].Chinese Journal of Bases and Clinics In General Surgery,2014,21(10):1321–1324.
[24]中华医学会外科学分会胆道外科学组.胆管损伤的诊断和治疗指南(2013版)[J].中华消化外科杂志,2013,12(2):81–95.doi:10.3760/cma.j.issn.1673–9752.2013.02.001.Biliary Surgery Group of Surgery Branch of Chinese Medical Association.Practice guideline for diagnosis and treatment of bile duct injury (2013 edition)[J].Chinese Journal of Digestive Surgery,2013,12(2):81–95.doi:10.3760/cma.j.issn.1673–9752.2013.02.001.
[25]Luigiano C,Iabichino G,Mangiavillano B,et al.Endoscopic management of bile duct injury after hepatobiliary tract surgery: a comprehensive review[J].Minerva Chir,2016,71(6):398–406.
[26]张喜财,陈志敏,张乐超.腹腔镜胆囊切除术中胆管损伤的发生原因及防治措施[J].腹腔镜外科杂志,2016,21(2):137–140.doi:10.13499 /j.cnki.Fqjwkzz.2016.02.137.Zhang XC,Chen ZM,Zhang LC.Injury causes and prevention measures of bile duct injury during laparoscopic cholecystectomy[J].Journal of Laparoscopic Surgery,2016,21(2):137–140.doi:10.13499/j.cnki.Fqjwkzz.2016.02.137.
[27]王敏华,龙厚东,李文放.腹腔镜胆囊切除术肝外胆管损伤24例分析[J].肝胆外科杂志,2015,23(2):138–141.Wang MH,Long HD,Li WF.Analysis of 24 extrahepatic bile duct injury caused by laparoscopic cholecystectomy[J].Journal of Hepatobiliary Surgery,2015,23(2):138–141.
[28]张璐,赵家泉,吕纯业,等.胆囊十二指肠瘘26例诊断与治疗[J].江苏医药,2016,42(3):346–347.Zhang L,Zhao JQ,Lu CY,et al.Diagnosis and treatment of cholecystoduodenal fi stula in 26 cases[J].Jiangsu Medical Journal,2016,42(3):346–347.
[29]Beksac K,Erkan A,Kaynaroglu V.Double Incomplete Internal Biliary Fistula: Coexisting Cholecystogastric and Cholecystoduodenal Fistula[J].Case Rep Surg,2016,2016:5108471.doi: 10.1155/2016/5108471.
[30]Negi RS,Chandra M,Kapur R.Bouveret syndrome: Primary demonstration of cholecystoduodenal fistula on MR and MRCP study[J].Indian J Radiol Imaging,2015,25(1):31–34.doi:10.4103/0971–3026.150136.
[31]Cavallaro A,Piccolo G,Panebianco V,et al.Incidental gallbladder cancer during laparoscopic cholecystectomy: managing an unexpected fi nding[J].World J Gastroenterol,2012,18(30):4019–4027.doi: 10.3748/wjg.v18.i30.4019.
[32]Dorobisz T,Dorobisz K,Chabowski M,et al.Incidental gallbladder cancer after cholecystectomy: 1990 to 2014[J].Onco Targets Ther,2016,9:4913–4916.doi: 10.2147/OTT.S106580.
[33]Tian YH,Ji X,Liu B,et al.Surgical treatment of incidental gallbladder cancer discovered during or following laparoscopic cholecystectomy[J].World J Surg,2015,39(3):746–752.doi:10.1007/s00268–014–2864–9.
[34]Choi KS,Choi SB,Park P,et al.Clinical characteristics of incidental or unsuspected gallbladder cancers diagnosed during or after cholecystectomy: a systematic review and meta-analysis[J].World J Gastroenterol,2015,21(4):1315–1323.doi: 10.3748/wjg.v21.i4.1315.
[35]Hu L,Wang B,Liu X,et al.Unsuspected gallbladder cancer: a clinical retrospective study[J].Arch Iran Med,2013,16(11):631–635.doi: 0131611/AIM.004.
[36]Zhang WJ,Xu GF,Tian ZQ,et al.Surgical approach does not in fl uence the outcome of incidental gallbladder carcinoma[J].Int J Clin Exp Med,2015,8(1):869–875.
[37]Utsumi M,Aoki H,Kunitomo T,et al.Evaluation of surgical treatment for incidental gallbladder carcinoma diagnosed during or after laparoscopic cholecystectomy: single center results[J].BMC Res Notes,2017,10(1):56.doi: 10.1186/s13104–017–2387–1.
[38]Choi KS,Choi SB,Park P,et al.Clinical characteristics of incidental or unsuspected gallbladder cancers diagnosed during or after cholecystectomy: a systematic review and meta-analysis[J].World J Gastroenterol,2015,21(4):1315–1323.doi: 10.3748/wjg.v21.i4.1315.
[39]马静,陈琳光,陈志男,等.腹腔镜胆囊切除术术中或术后意外胆囊癌的处理对策[J].临床外科杂志,2014,22(5):338–340.doi:10.3969/j.issn.1005–6483.2014.05.013.Ma J,Chen LG,Chen ZN,et al.Treatment strategies for unsuspected gallbladder carcinoma during or after laparoscopic cholecys-tectomy[J].Journal of Clinical Surgery,2014,22(5):338–340.doi:10.3969/j.issn.1005–6483.2014.05.013.
[40]Swank HA,Mulder IM,Hop WC,et al.Routine histopathology for carcinoma in cholecystectomy specimens not evidence based: a systematic review[J].Surg Endosc,2013,27(12):4439–4448.doi:10.1007/s00464–013–3084–3.
[41]柴长鹏,徐广甍,宋晓伟,等.腹腔镜胆囊切除术中意外胆囊癌的诊治[J].中华肝胆外科杂志,2014,20(9):659–661.doi:10.3760/cma.j.issn.1007–8118.2014.09.010.Chai CP,Xu GM,Song XW,et al.Diagnosis and treatment of unexpected gallbladder carcinoma in laparoscopic cholecystectomy[J].Chinese Journal of Hepatobiliary Surgery,2014,20(9):659–661.doi:10.3760/cma.j.issn.1007–8118.2014.09.010.
[42]Meinero M,Melotti G,Mouret Ph,eds.Laparoscopic surgery[M].Italy: Masson S.p.A,Milano,1994:160–166.
[43]Malik AM.Dif fi cult laparoscopic cholecystectomies.Is conversion a sensible option?[J].J Pak Med Assoc,2015,65(7):698–700.
[44]Sippey M,Grzybowski M,Manwaring ML,et al.Acute cholecystitis: risk factors for conversion to an open procedure[J].J Surg Res,2015,199(2):357–361.doi: 10.1016/j.jss.2015.05.040.
[45]Oymaci E,Ucar AD,Aydogan S,et al.Evaluation of affecting factors for conversion to open cholecystectomy in acute cholecystitis[J].Prz Gastroenterol,2014,9(6):336–341.doi:10.5114/pg.2014.45491.
[46]郑奇志,张剑锋,谢湛荣,等.腹腔镜胆囊切除术中转开腹的影响因素分析[J].临床肝胆病杂志,2015,31(10):1671–1674.doi:10.3969/j.issn.1001–5256.2015.10.027.Zheng QZ,Zhang JF,Xie ZR,et al.Analysis of in fl uencing factors for conversion of laparoscopic cholecystectomy to open surgery[J].Journal of Clinical Hepatology,2015,31(10):1671–1674.doi:10.3969/j.issn.1001–5256.2015.10.027.
[47]Philip Rothman J,Burcharth J,Pommergaard HC,et al.Preoperative Risk Factors for Conversion of Laparoscopic Cholecystectomy to Open Surgery - A Systematic Review and Meta-Analysis of Observational Studies[J].Dig Surg,2016,33(5):414–423.doi:10.1159/000445505.
[48]陈大红,汪泳,王健,等.急性胆囊炎行腹腔镜胆囊切除术中转开腹的危险因素分析[J].安徽医药,2016,20(8):1527–1529.doi:10.3969/j.issn.1009–6469.2016.08.029.Chen DH,Wang Y,Wang J,et al.Risk factors for conversion of laparoscopic cholecystectomy to open cholecystectomy in patients with acute cholecystitis[J].Anhui Medical and Pharmaceutical Journal,2016,20(8):1527–1529.doi:10.3969/j.issn.1009–6469.2016.08.029.