先天性胆总管囊肿是一种较少见的胆管树异常扩张的疾病,一般在婴幼儿期被发现,而成人较少见,女性高发(女:男=4:1)[1-4],其具有较高的癌变率,且随着年龄的增长,癌变率逐渐增加[5];另外先天性胆总管囊肿可引起胆道结石、胆管狭窄、胆管炎、胰腺炎等并发症,因此,手术切除胆总管囊肿为目前唯一的根治方法[6];自1995年首先报道了腹腔镜胆总管囊肿切除+胆管空肠吻合术[7],腹腔镜手术开始应用于先天性胆总管囊肿的治疗。本文回顾性分析了昆明医科大学第一附属医院2014年5月—2016年5月12例腹腔镜下胆总管囊肿手术治疗的临床资料,现报告如下。
1 资料与方法
1.1 临床资料
12例患者因先天性胆总管囊肿于2014年5月—2016年5月期间先后入住我院,其中女10例,男2例;年龄在20~65岁,中位年龄35岁;病史1个月至10年;10例患者均有腹痛症状,其中4例伴有黄疸,4例患者合并有胆囊结石,2例患者合并有胆总管结石,1例患者既往有腹股沟斜疝手术史,其余患者均无手术史。术前均行腹部彩超、CT、MRI、MRCP证实为先天性胆总管囊肿诊断,囊肿直径4.5~8.4cm,Todani分型:10例为I型,2例为IV型。
1.2 手术方法及步骤
全麻成功后,常规消毒铺单,患者取头高脚低、左侧倾斜卧位,腔镜显示器位于患者右侧靠头;先做肚脐上缘横切口12 mm,进入气腹针,建立气腹,维持气腹压力14 mmHg(1 mmHg=0.133 kPa),以四孔法操作,其它三孔分别位于剑突下2cm,右侧锁骨中线肋缘下2cm,右侧腋前线肋缘下4cm,置入腹腔镜及各种腔镜器械。首先常规探查腹腔内各脏器、胆总管及其与周围组织粘连情况。仔细分离扩张的胆总管与周围组织的粘连,辨认出左右肝管、门静脉、肝右动脉;解剖胆囊三角,游离出胆囊动脉,2-0可吸收线结扎离断,在浆膜下逆行将胆囊从胆囊床上剥离出,完全游离出肝门部肝总管,吊带,在肝总管与囊肿交界处下0.5cm处切断肝总管,肝总管残端修剪成敞口状,稍微外翻,备用;以超声刀紧贴囊肿壁由上而下剥离囊肿至胆总管突然变细处(图1A),予以单向倒刺线即3-0 V-lock180(Covidien)线缝扎后切除胆总管囊肿及胆囊(图1B),移除标本;如果囊肿巨大(直径8cm及以上)或术前证实胆总管结石,建议先切开减压、胆道镜探查取石[8];在屈氏韧带远端15cm处,使用超声刀自空肠系膜根部切开肠系膜,要确保肠系膜两端血运良好,用45 mm Endo-GIA横断空肠(图1C),在远端空肠距断端约40cm处与近端空肠以60 mm Endo-GIA行系膜对系膜肠肠侧侧吻合(图1D),残留小口及系膜裂孔以2-0可吸收线间断缝合;将旷置的远端空肠袢经结肠后上提至肝十二指肠韧带旁(图1E),确认没有扭转、牵拉、张力,在距断端4~5cm处系膜对侧空肠上开一大小与肝管断面直径一致的小口,以3-0 V-lock180(Covidien)线连续、全层、外翻行肝管-空肠端侧吻合(图1F),以3-0 Prolene线将吻合口左右的肠壁与肝十二指肠韧带分别固定1针,以减少吻合口张力;若胆管炎症较重,则留置经吻合口T管;仔细检查,腹腔内确切止血后,冲洗腹腔,明确无活动性出血及胆漏,于胆肠吻合口后方放置腹腔引流管1根,清点器械无误后取出腔镜器械,切口行可吸收线皮下缝合。
2 结 果
2.1 手术及术中情况
12例患者均在完全腹腔镜下完成胆总管囊肿切除+肝管空肠吻合术,其中1例为减少手术费用在腹腔外实行手工肠肠吻合;手术时间为240~310 min,平均280 min;术中出血20~150mL,平均60mL(出血150mL的为笔者开展的第1例患者,未使用超声刀)。
2.2 术后及随访情况
术后第1天拔出胃管及导尿管,并开始下床活动;术后2~3 d肛门排气,进食流质;术后3~4 d拔除胆肠吻合口下引流管;术后住院5~7 d,平均住院6.5 d;2例带T管的患者术后2个月拔除T管;所有患者术后随访2~12个月,无胆瘘及其他并发症出现,无死亡病例。
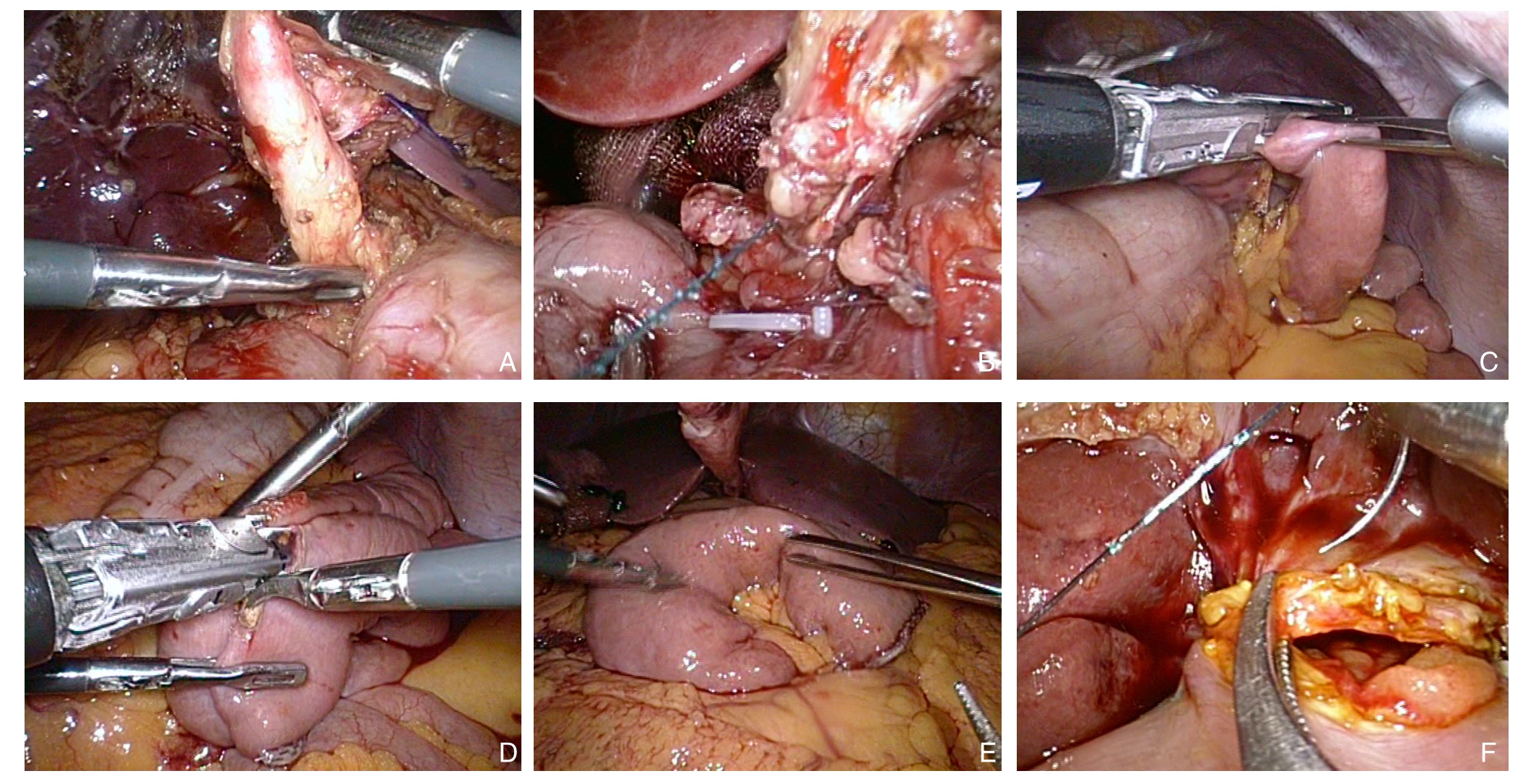
图1 术中照片 A:剥离胆总管囊肿;B:倒刺线缝扎囊肿下段;C:Endo-GIA离断空肠;D:肠肠侧侧吻合;E:结肠后上提远端空肠;F:倒刺线肝肠吻合
Figure 1 Intraoperative views A: Dissociation of the choledochus cyst; B: Suturing the inferior segment of the cyst with barbed suture;C: Division of the jejunum by Endo-GIA; D: Side-to side enteroenterostomy; E: Pulling the distal jejunum from the posterior side of the colon; F: Hepatoenterostomy with barbed suture
3 讨 论
随着腹腔镜设备及技术不断更新及发展,肝胆胰外科疾病越来越多的使用腹腔镜手术治疗[9],先天性胆总管囊肿也不例外,早在1995年,Farello等[7]首先报道了腹腔镜胆总管囊肿切除+胆管空肠吻合术,证明了该术式可行性,目前国内很多大型医院也开展了腹腔镜下胆总管囊肿切除+肝管-空肠Roux-en-Y吻合术;本组资料中患者均采用腹腔镜下胆总管囊肿+肝管-空肠Roux-en-Y吻合术,手术疗效甚佳。
腹腔镜胆总管囊肿切除术具有很多技术难题,囊肿完全切除难度高,如囊肿周围炎症粘连严重将增加肝动脉、门静脉损伤风险,并增加术后创面滲血的发生率[10],如果囊肿下段被胰腺包裹,分离过程中则容易损伤胰管,出现胰瘘[11];同时在完全腹腔镜下消化道重建又是一大难点,腔镜下肝管空肠吻合技术难度高,容易出现胆瘘或者吻合口狭窄等手术并发症[12],要求术者在腔镜下缝合非常熟练;而笔者的经验是:借助腹腔镜下缝合打结技术和切割吻合器的应用,完全腹腔镜手术进行胆总管切除肝肠吻合手术是可行的。尤其是腔镜下直线切割闭合器的使用,大大缩短了腔镜下行肝管-空肠Roux-en-Y吻合术的时间,同时也明显降低了术后出现肠粘连梗阻等并发症的几率[13];但对于基层医院,若基于条件限制,无法使用腔镜下直线切割闭合器,则也可采用延长剑突下Trocar至3cm,将空肠牵拉至腔外行肠肠侧侧吻合,吻合后再回拉至腹腔内行腔镜下肝管-空肠吻合,手术时间无明显差异,本组有1例患者因费用问题,采取此法,效果良好。
胆总管囊壁的剥离为手术的难点,笔者的经验是使用超声刀,在助手的提拉下由上而下完整剥离,若囊肿较大,影响暴露,可以先切开减压[14],再顺行剥除,使用超声刀可以明显减少囊壁的渗血[15],本组第一台腔镜下胆总管囊肿切除手术时,使用电钩剥离,剥离后创面渗血较多,耽误较多的手术时间在创面止血上;关于创面止血笔者的经验是从下而上逐步荷包缝合加压止血,荷包内可内包凝胶海绵,这样止血效果较好。
目前主流观点认为胆总管囊肿的形成主要是由于胰胆管合流异常[16]及Oddi括约肌功能障碍等各种原因导致胰液返流侵蚀胆管内壁,其内的胰蛋白酶及弹力纤维酶等会破坏胆管壁[17],使其变薄弱,最后形成囊肿,囊肿下段与胰腺的胰管距离极近;故在分离胆总管囊肿胰腺段时,切记勿追求完全切除,否则损伤胰管可能性较大,容易造成胰瘘等手术并发症,笔者的经验是术前仔细阅片,评估囊肿与胰腺的关系,在囊肿下段突然变细时横断囊肿,使用3-0 V-lock180(Covidien)线缝扎,仔细检查,切勿损伤胰腺;同样,对于IVa型囊肿患者也釆用肝外胆管囊肿切除+肝管空肠Roux-en-Y吻合术,切勿追求囊肿全部切除。
空肠的离断及肠肠吻合均可使用腔镜下直线切割闭合器(Endo-GIA),可明显缩短吻合时间;另外其中有一病例(该患者来自云南山区,家境贫寒),为减少手术费用,笔者采用的是延长剑突下Trocar至3cm,把空肠拉至腹腔外行肠肠侧侧吻合。
肝管-空肠吻合为手术的又一个难点,手术切除囊肿时不要追求高位离断,可预留少量囊壁组织,修剪使其成敞口状,稍微外翻,吻合时采用单向倒刺即3-0 V-lock180(Covidien)线连续全层缝合,单向倒刺线吻合优点在于整个吻合过程均无需打结,且收紧线后不会滑脱,可明显缩减吻合时间,当然使用倒刺线缝合必须注意,在缝合结束时,缝回1~2针,残留线紧贴组织剪除,防止残留线割伤肠管,引起炎症粘连可能[18];缝合后在吻合口左右两边各缝合1针,连接肠壁及肝门部纤维组织,以减少吻合口张力,并由此可减少吻合口瘘的发生几率。
相比于传统开腹胆总管囊肿切除术,完全腹腔镜下胆总管囊肿切除+肝管空肠Roux-en-Y吻合术,视野灵活全面,且腹腔镜具有放大功能,将组织放大至4~8倍后,可以清晰显示囊肿周围的血管结构,便于术中精确操作、减少出血及其他副损伤[19];且手术创伤小、疼痛轻、对胃肠道影响少[20-21],术后美观生活质量明显提高,术后肛门排气早、进食早,平均住院时间短,符合快速康复外科(ERAS)理念[22-23]。从目前随访来看,本组资料12例患者术后均恢复良好,无明显手术并发症发生,当然,由于随访时间较短,有待于进一步观察疗效。因此,该术式是安全可行且具有很大优势,可进一步推广[24-25],基层医院也可依情况施行,但必须有较扎实的腔镜技术及非常熟悉肝胆胰解剖,且严格把握手术指征。
参考文献
[1]Singham J,Yoshida EM,Scudamore CH.Choledochal cysts:part 1 of 3: classification and pathogenesis[J].Can J Surg,2009,52(5):434–440.
[2]Tan SS,Tan NC,Ibrahim S,et al.Management of adult choledochal cyst[J].Singapore Med J,2007,48(6):524–527.
[3]Jang JY,Yoon YS,Kang MJ,et al.Laparoscopic excision of a choledochal cyst in 82 consecutive patients[J].Surg Endosc,2013,27(5):1648–1652.doi: 10.1007/s00464–012–2646–0.
[4]段小辉,蒋波,毛先海,等.完全腹腔镜在先天性胆总管囊肿手术中的应用[J].中国普通外科杂志,2013,22(8):1057–1060.doi:10.7659/j.issn.1005–6947.2013.08.021.Duan XH,Jiang B,Mao XH,et al.Total laparoscopic technique for congenital choledochal cyst[J].Chinese Journal of General Surgery,2013,22(8):1057–1060.doi:10.7659/j.issn.1005–6947.2013.08.021.
[5]Søreide K,Søreide JA.Bile duct cyst as precursor to biliary tract cancer[J].Ann Surg Oncol,2007,14(3):1200–1211.
[6]王钊,王群,王佳辰,等.完全腹腔镜下改良胆肠襻式吻合与Roux-en-Y吻合治疗成人Ⅰ型胆总管囊肿[J].中华普通外科杂志,2016,31(1):4–7.doi:10.3760/cma.j.issn.1007–631X.2016.01.002.Wang Z,Wang Q,Wang JC,et al.Modified uncut jejunal loop vs Roux-en-Y hepaticojejunostomy in totally laparoscopic treatment for type Ⅰ adult choledochal cyst[J].Zhong Hua Pu Tong Wai Ke Za Zhi,2016,31(1):4–7.doi:10.3760/cma.j.issn.1007–631X.2016.01.002.
[7]Farello GA,Cerofolini A,Rebonato M,et al.Congenital choledochal cyst: video-guided laparoscopic treatment[J].Surg Laparosc Endosc,1995,5(5):354–358.
[8]孙强,常晓健,胡泽民,等.完全腹腔镜下胆肠Roux-en-Y吻合术的应用:附25例报告[J].中国普通外科杂志,2015,24(2):226–230.doi:10.3978/j.issn.1005–6947.2015.02.014.Sun Q,Chang XJ,Hu ZM,et al.Application of modified totally laparoscopic Roux-en-Y hepaticojejunostomy: a report of 25 cases[J].Chinese Journal of General Surgery,2015,24(2):226–230.doi:10.3978/j.issn.1005–6947.2015.02.014.
[9]Choi SB,Choi SY.Current status and future perspective of laparoscopic surgery in hepatobiliary disease[J].Kaohsiung J Med Sci,2016,32(6):281–291.doi: 10.1016/j.kjms.2016.05.006.
[10]李龙,余奇志,刘刚,等.经腹腔镜行先天性胆总管囊肿根治切除术的技术要点[J].中华普通外科杂志,2002,17(8):473–475.doi:10.3760/j.issn:1007–631X.2002.08.010.Li L,Yu QZ,Liu G,et al.Laparoscopic total cyst excision with Roux-Y hepatoenterostomy for choledochal Cyst[J].Zhong Hua Pu Tong Wai Ke Za Zhi,2002,17(8):473–475.doi:10.3760/j.issn:1007–631X.2002.08.010.
[11]Lima M,Gargano T,Ruggeri G,et al.Laparoscopic treatment of congenital choledochal cyst and hepaticojejunostomy with extracorporeal Roux-en-Y anastomosis: technical aspects and early experience with three cases[J].Pediatr Med Chir,2016,38(2):125.doi: 10.4081/pmc.2016.125.
[12]Urushihara N,Fukumoto K,Fukuzawa H,et al.Long-term outcomes after excision of choledochal cysts in a single institution:operative procedures and late complications[J].J Pediatr Surg,2012,47(12):2169–2174.doi: 10.1016/j.jpedsurg.2012.09.001.
[13]Laje P,Questa H,Bailez M.Laparoscopic leak-free technique for the treatment of choledochal cysts[J].J Laparoendosc Adv Surg Tech A,2007,17(4):519–521.
[14]Abbas HM,Yassin NA,Ammori BJ.Laparoscopic resection of type I choledochal cyst in an adult and Roux-en-Y hepaticojejunostomy:a case report and literature review[J].Surg Laparosc Endosc Percutan Tech,2006,16(6):439–444.
[15]贾钧,李龙,刘钢,等.腹腔镜下应用超声刀行胆总管囊肿切除术[J].中华外科杂志,2004,42(17):1056–1059.doi:10.3760/j:issn:0529–5815.2004.17.009.Jia J,Li L,Liu G,et al.Total cyst exicision with ultrasonic scalpel under the laparoscope for choledochal cyst[J].Chinese Journal of Surgery,2004,42(17):1056–1059.doi:10.3760/j:issn:0529–5815.2004.17.009.
[16]许圣献,单礼成,范西红,等.先天性胰胆管合流异常[J].中国普通外科杂志,1998,7(3):133–135.Xu SX,Shan LC,Fan XH,et al.Congenital Pancreaticobiliary Maljunction[J].Chinese Journal of General Surgery,1998,7(3):133–135.
[17]王凤飚,王新超.胆总管囊肿诊治新进展[J].医学综述,2013,19(16):2950–2952.doi:10.3969/j.issn.1006–2084.2013.16.025.Wang FB,Wang XC.Recent Progress in Diagnosis and Treatment of Choledochal Cysts[J].Medical Recapitulate,2013,19(16):2950–2952.doi:10.3969/j.issn.1006–2084.2013.16.025.
[18]段键,夏仁品,林杰,等.单向倒刺线在腹腔镜肝叶切除联合术中胆道探查中的运用[J].中国普通外科杂志,2016,25(2):186–190.doi:10.3978/j.issn.1005–6947.2016.02.005.Duan J,Xia RP,Lin J,et al.Application of unidirectional barbed suture in laparoscopic hepatectomy with bile duct exploration[J].Chinese Journal of General Surgery,2016,25(2):186–190.doi:10.3978/j.issn.1005–6947.2016.02.005.
[19]Yamataka A,Lane G J,Cazares J.Laparoscopic surgery for biliary atresia and choledochal cyst[J].Semin Pediatr Surg,2012,21(3):201–210.doi: 10.1053/j.sempedsurg.2012.05.011.
[20]林洋,魏威,张晓辉,等.腹腔镜与开放肝总管空肠Roux-en-Y吻合术后并发症比较的Meta分析[J].临床肝胆病杂志,2016,32(10):1959–1963.doi:10.3969/j.issn.1001–5256.2016.10.029.Lin Y,Wei W,Zhang XH,et al.Postoperative complications of laparoscopic versus open common hepatic duct-jejunal Roux-en-Y anastomosis: a Meta-analysis[J].Journal of Clinical Hepatology,2016,32(10):1959–1963.doi:10.3969/j.issn.1001–5256.2016.10.029.
[21]Zhen C,Xia Z,Long L,et al.Laparoscopic excision versus open excision for the treatment of choledochal cysts: a systematic review and meta-analysis[J].Int Surg,2015,100(1):115–122.doi: 10.9738/INTSURG–D–14–00165.1.
[22]周庆.不同手术方式治疗成人先天性胆管扩张症的临床疗效研究[J].临床和实验医学杂志,2015,14(6):488–490.doi:10.3969/j.issn.1671–4695.2015.06.020.Zhou Q.Clinical study on efficacy of different operation procedures for treatment of adult congenital cholangiectasis[J].Journal of Clinical and Experimental Medicine,2015,14(6):488–490.doi:10.3969/j.issn.1671–4695.2015.06.020.
[23]柴悦,秦鸣放,赵宏志,等.腹腔镜下胆管囊肿切除、肝管空肠Roux-en-Y吻合术治疗成人CDBD效果观察[J].山东医药,2016,56(3):60–62.doi:10.3969/j.issn.1002–266X.2016.03.023.Chai Y,Qin MF,Zhao HZ,et al.Efficacy observation of laparoscopic choledochal cyst excision with Roux-en-Y hepaticojejunostomy in treatment of adult CDBD[J].Shandong Medical Journal,2016,56(3):60–62.doi:10.3969/j.issn.1002–266X.2016.03.023.
[24]Palanivelu C,Rangarajan M,Parthasarathi R,et al.Laparoscopic management of choledochal cysts: technique and outcomes--a retrospective study of 35 patients from a tertiary center[J].J Am Coll Surg,2008,207(6):839–846.doi: 10.1016/j.jamcollsurg.2008.08.004.
[25]曾帅丹,刘磊,王斌,等.腹腔镜与开放手术治疗胆总管囊肿临床效果的Meta分析[J].中国普通外科杂志,2014,23(2):153–159.doi:10.7659/j.issn.1005–6947.2014.02.003.Zeng SD,Liu L,WAng B,et al.Laparoscopic versus open surgery for choledochal cyst: a Meta-analysis[J].Chinese Journal of General Surgery,2014,23(2):153–159.doi:10.7659/j.issn.1005–6947.2014.02.003.