乳腺癌是全世界女性最常见的恶性肿瘤,其发病率有逐年上升趋势[1]。早期乳腺癌保乳手术的肿瘤学安全性已得到广泛认可,在I~II期乳腺癌患者中,保乳术+放疗与改良根治术治疗效果相当,两者的远处转移率和生存率的差异均无统计学意义[2];最近一项来自荷兰的大宗回顾性研究甚至显示接受保乳手术的患者的预后优于全乳切除的患者[3]。部分患者因肿瘤较大或肿瘤所在部位限制,施行传统保乳术不能获得满意的美学效果,进而放弃保乳。整形保乳术将整形外科的理念和技术应用于传统保乳术,切除肿瘤的同时,尽可能维持术后乳房外形的美观。与传统保乳术比较,整形保乳术在保证切缘阴性的前提下,具有更好的外形及对称性[4]。目前关于肿瘤整形保乳术的文献报道多见于具有较大乳房的欧美患者,在较小乳房的亚洲人群中的应用韩国有少量报道[5-6],国内也有小样本量的报道[7-12]。我中心自2011年8月—2016年8月应用肿瘤整形技术施行早期乳腺癌的保乳手术139例,取得良好效果,现报告如下。
1 资料与方法
1.1 一般资料
139例乳腺癌患者均经彩超、钼靶及核磁共振检查证实为单发病灶,无广泛沙粒样钙化灶存在,无放疗禁忌证。同期施行改良根治术的1 271例I~II期乳腺癌,其中包含2个及2个以上病灶的患者和广泛沙粒样钙化灶的患者。所有病例均为女性,均无远处转移,术前均经空芯针穿刺或微创活检病理证实,术前未行放、化疗。两组患者在年龄、月经状况、肿瘤大小、部位及激素受体表达等方面差异无统计学意义(均P>0.05)(表1)。
1.2 手术治疗
1.2.1 切口设计及肿瘤原发灶切除 根据肿块大小、部位、乳房大小、下垂度以及健侧乳房是否愿意接受整形手术等方面综合考虑,选择不同的手术方式并设计切口。首先切开皮肤及皮下组织后,向四周游离乳腺组织,肿瘤原发灶切除范围包括肿瘤、肿瘤周围1~2 cm乳腺组织及肿瘤深部的胸大肌筋膜,活检穿刺针道、活检残腔及活检切口皮肤瘢痕应包括在切除范围内,如肿瘤位置较深,临床判断未累及皮肤,可不切除肿瘤表面皮肤。
1.2.2 运用整形技术进行缺损修复 术中冷冻确认切缘阴性后,放置钛夹标记瘤区。运用肿瘤整形技术修复乳腺缺损,对于切除组织较少和/或乳房较大的患者,采用体积易位技术(局部腺体瓣转移修补法),游离残腔周围腺体,将乳腺内腺体组织瓣经旋转、移位及缝合以关闭残腔,重新塑形。对于切除组织较多和/或乳腺较小的患者,采用体积置换技术(自体组织移植修补法),获取适量带血管蒂的背阔肌组织瓣,通过皮下隧道将组织瓣转位至缺损区域,修复乳腺缺损。
1.2.3 腋窝淋巴结处理 依据术前腋窝情况及患者、家属意愿,行腋窝淋巴结清扫术或前哨淋巴结活检术;施行前哨淋巴结活检术的患者,联合应用美蓝和放射性同位素双标定位法,术中冷冻前哨淋巴结阳性则行腋窝淋巴结清扫术;如果术中冷冻前哨淋巴结阴性,术后病理前哨淋巴结阳性则补行腋窝淋巴结清扫术。
1.2.4 健侧乳房处理 在患者及家属同意的前提下,同时对中-重度下垂的健侧乳房进行上提手术或缩乳术,以保持双侧乳房的对称性。
表1 整形保乳术组和改良根治术组一般资料比较[n(%)]
Table 1 Comparison of the general data between patients undergoing oncoplastic breast-conserving surgery and modified radical mastectomy [n (%)]
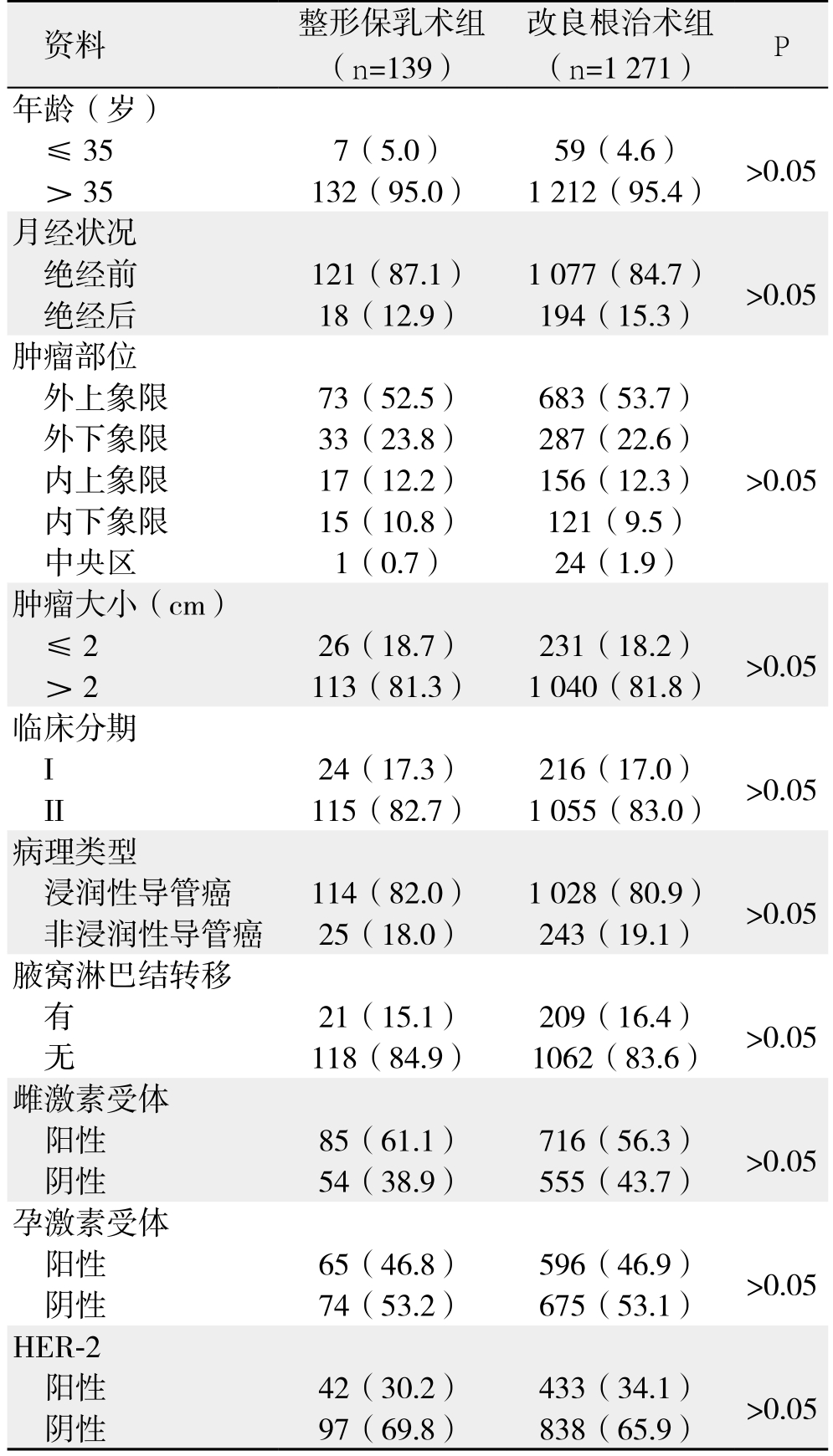
资料 整形保乳术组(n=139)改良根治术组(n=1 271) P年龄(岁)≤35 7(5.0) 59(4.6) >0.05> 35 132(95.0) 1 212(95.4)月经状况绝经前 121(87.1) 1 077(84.7) >0.05绝经后 18(12.9) 194(15.3)肿瘤部位外上象限 73(52.5) 683(53.7)>0.05外下象限 33(23.8) 287(22.6)内上象限 17(12.2) 156(12.3)内下象限 15(10.8) 121(9.5)中央区 1(0.7) 24(1.9)肿瘤大小(cm)≤2 26(18.7) 231(18.2) >0.05> 2 113(81.3) 1 040(81.8)临床分期I 24(17.3) 216(17.0) >0.05 II 115(82.7) 1 055(83.0)病理类型浸润性导管癌 114(82.0) 1 028(80.9) >0.05非浸润性导管癌 25(18.0) 243(19.1)腋窝淋巴结转移有21(15.1) 209(16.4) >0.05无118(84.9) 1062(83.6)雌激素受体阳性 85(61.1) 716(56.3) >0.05阴性 54(38.9) 555(43.7)孕激素受体阳性 65(46.8) 596(46.9) >0.05阴性 74(53.2) 675(53.1)HER-2阳性 42(30.2) 433(34.1) >0.05阴性 97(69.8) 838(65.9)
1.3 术后综合治疗
参照NCCN指南及中国抗癌协会乳腺癌诊治指南及规范,根据术后病理结果及病理分期,进行化疗、放疗、内分泌治疗及靶向治疗等综合治疗。
1.4 美容效果评价
采用美国放射治疗肿瘤协会(Radiation Therapy Oncology Group,RTOG)美容等级量表(2版)评定美容效果。优秀:患侧乳房大小、形状与健侧乳房无差别或只有微小差别;良好:患侧乳房大小、形状与健侧乳房存在轻度差别;一般:≤1/4患侧乳房在大小和形状方面存在明显改变;差:>1/4患侧乳房在大小和形状方面存在明显改变[12]。
1.5 随访
所有患者均进行电话和/或门诊随访,首次随访时间为术后1个月,2年内每3个月随访1次,其后每6个月随访1次。失访患者自失访之日起视为死亡。随访内容包括生存情况、复发转移情况、美容效果评估、生活质量评估、一般生化检查、肿瘤标志物、影像学检查评估等。
1.6 统计学处理
所有数据采用SPSS 18.0统计软件进行统计学处理,计量资料采用χ2检验,P<0.05为差异有统计学意义。
2 结 果
2.1 保乳手术情况
139例患者中133例患者采用体积易位技术(局部腺体瓣转移修补法),选择弧形切口、双环切口(图1)、网球拍状切口(图2A)、蝙蝠翼切口及垂直切口最常见(表2);其中45例同时接受对侧乳房手术(图2B),其中30例上提术,15例缩乳术。6例患者采用体积置换技术(自体组织移植修补法),选择背阔肌组织瓣修补缺损(图2C)。139例乳腺癌中78例患者行前哨淋巴结活检术,61例患者接受腋窝淋巴结清扫术(其中11例患者术中前哨淋巴结活检阳性,改行腋窝淋巴结清扫术)。139例患者切除组织标本重30~187 g,平均69.5 g;其中有9例患者术中首次病理冷冻结果示切缘阳性,再次切取切缘送术中冷冻及石蜡病理检查均证实为阴性;1例中央区乳腺癌因乳头深面切缘阳性行乳头乳晕复合体(nipple areola complex,NAC)切除。

图1 右乳内上肿瘤双环法保乳 A:术前;B:术后1周;C:术后3个月
Figure 1 Breast-conserving surgery with double curvilinear incision for breast cancer at right upper inner quadrant A: Preoperative view;B: Postoperative one-week view; C: Postoperative 3 month view
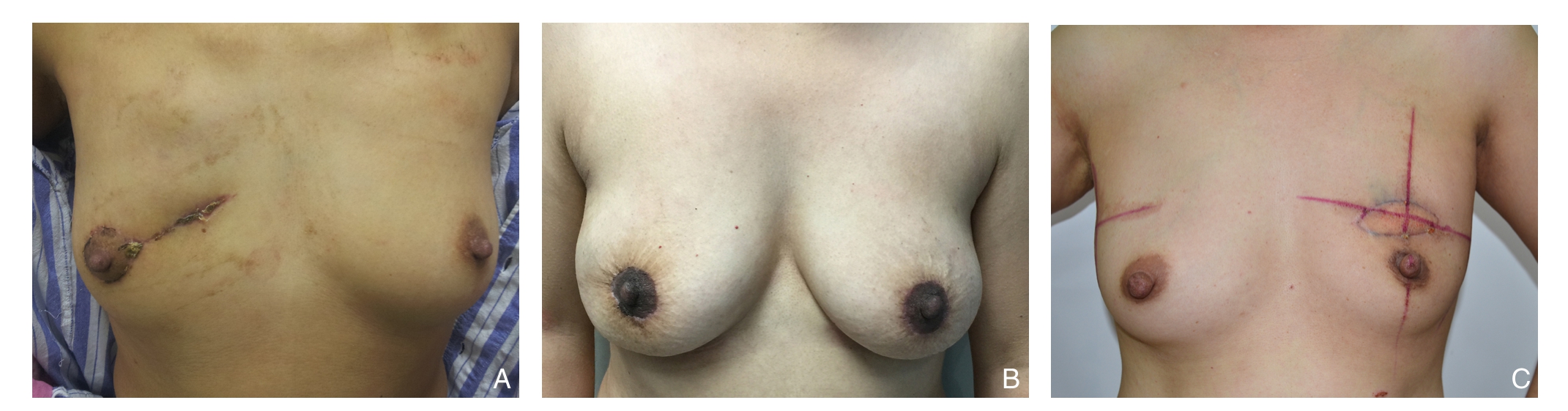
图2 其他切口与手术方式 A:右乳内上肿瘤球拍状切口保乳;B:右乳癌双环切口保乳,左乳双环切口缩乳;C:左乳癌,肿瘤位于乳头上方,背阔肌填充保乳
Figure 2 Other incisions and procedures A: Breast-conserving surgery with acket-shaped incision for breast cancer at right upper inner quadrant; B: Breast-conserving surgery with double curvilinear incision for right breast cancer and breast reduction surgery for left breast; C: Breast-conserving surgery with latissimus dorsi muscle flap filling for left breast cancer above the nipple
2.2 术后并发症及美容效果评估
18例患者出现局部皮下积液,2例患者出现切口裂开,2例患者出现局部感染,3例患者出现NAC部分缺血,经对症处理后痊愈。其余患者伤口愈合良好,无皮下出血、感染、皮瓣坏死、NAC坏死等并发症。
RTOG美容等级量表评定结果为:优秀79例(56.8%),良好47例(33.8%),一般10例(7.2%),差3例(2.2%)。评价为一般等级的患者中,8例患者认为手术瘢痕较大,1例患者认为乳房不对称,1例中央区乳腺癌患者未能保留NAC;美容效果评价为差的原因是患者拒绝对健侧乳房进行整形,造成双侧乳房明显不对称。
2.3 随访
139例行肿瘤整形保乳术患者术后随访3~63个月,平均28.8个月,局部复发6例,远处转移8例(骨转移2例,肝转移3例,肺转移1例,颈部淋巴结转移1例,合并肝骨转移1例),死亡3例,失访3例;术后2年局部复发率4.3%,总生存率95.7%,无病生存率85.6%。同期1 271例行乳腺癌改良根治术的I~II乳腺癌患者,术后局部复发52例,远处转移78例,死亡21例,失访36例;术后局部复发率4.1%,总生存率95.5%,无病生存率85.3%,两组差异无统计学意义(表2)。
表2 肿瘤整形保乳术与改良根治术患者预后比较(%)
Table 2 Comparison of outcomes between patients undergoing oncoplastic breast-conserving surgery and modified radical mastectomy (%)
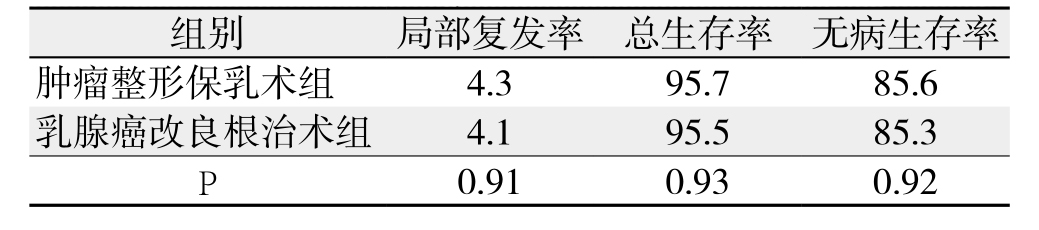
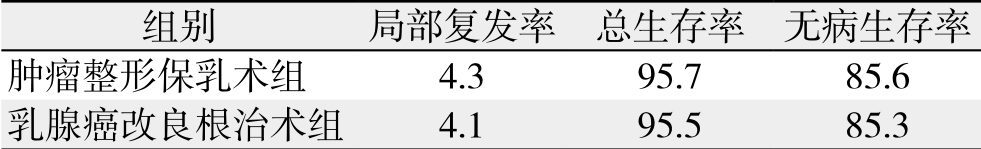 P 0.91 0.93 0.92
P 0.91 0.93 0.92
3 讨 论
3.1 肿瘤整形保乳术的肿瘤学安全性
肿瘤整形外科,是将整形外科的原则和技术用于癌症患者的治疗,在切除肿瘤的同时尽可能地恢复因手术遭到破坏的功能和外观。乳腺癌整形保乳术在保乳的同时取得了良好的美容效果,扩大了保乳手术的适应证,使肿块>4 cm的患者也能在保乳的同时不影响生存期[13]。
长期随访研究表明:对于早期乳腺癌患者,肿瘤整形保乳术与传统保乳术、全乳切除之间,在局部复发率、总生存期、无病生存期上没有显著差异[14-16]。Calì Cassi等 [17]的研究显示,整形保乳术组的再次手术切除率明显低于传统保乳术组,并且两组间局部复发率及生存期差异无统计学意义,笔者认为早期乳腺癌中整形保乳术可以有效地替代传统保乳术。De La Cruz等[18]纳入55篇文章进行系统的文献回顾,共计6 011例接受肿瘤整形保乳术的T1~T2乳腺癌患者,总生存率为95.0%,无病生存率为90.0%,局部复发率为3.2%,远处复发率为8.7 %,研究结果显示在T1~T2乳腺癌中,肿瘤整形保乳术具有很好的肿瘤学安全性。并且有研究显示,因应用肿瘤整形技术后,切除的组织可以相对较多,更容易获得阴性病理切缘,局部复发率相对较低[19-20]。以上结果证实了肿瘤整形保乳手术的可行性及肿瘤学安全性。本组研究资料也显示,与接受乳腺癌改良根治术的患者比较,接受整形保乳手术患者的局部复发率、总生存率以及无病生存率差异无统计学意义。
3.2 肿瘤整形技术的选择
体积易位指乳腺病灶切除后利用周围腺体、皮肤腺体瓣移位并转移到切除后的缺损区[21] 。一般用于肿瘤原发灶切除后小或中等量腺体缺失的患者,创伤较小,为整形保乳手术的首选。体积置换指自远处获得自体组织移植到切除后的缺损区,修复切除的乳腺组织缺损[21],最常用的组织为背阔肌组织瓣。主要用于乳房体积相对较小而切除组织量较大的患者,新增供区瘢痕,手术创伤较大。
本组资料中133例(88.5%)患者采用体积易位技术,其中45例(39.8%)同时接受对侧乳房手术,以保持对称性。6例(11.5%)患者采用体积置换技术,均采用背阔肌组织瓣修补缺损。
3.3 手术切口设计
肿瘤整形保乳术的切口设计应综合考虑肿瘤大小、部位、距NAC的距离及乳房大小、下垂度等因素。Iwuchukwu等[22]对于乳房不同部位的肿瘤进行整形保乳术的切口选择进行了文献回顾。
本组资料选择弧形切口、网球拍状切口、双环切口、蝙蝠翼切口及垂直切口等,均能达到较为满意的美容效果。沿皮纹方向或平行于乳晕的同心圆线的弧形切口是我们最常使用的切口,适用于切除组织量较小的患者。中国女性乳房大多为中小乳房,弧形切口、网球拍状切口、双环切口适用于大多数患者,美容效果较好。对于乳房较大且下垂明显的患者,可以选择倒T形切口或垂直切口。
3.4 肿瘤整形保乳术的病例选择
肿瘤整形保乳术的切缘阳性率为7%~10%,复发率为5%;年轻患者、肿瘤体积较大、导管内癌均是切缘阳性的危险因素[23]。选择合适的病例,是降低切缘阳性率及局部复发率的有效手段。目前国外也有局部晚期乳腺癌在新辅助化疗后,进行肿瘤整形保乳术的文献报道[24-25],在没有更多的大宗病例报道之前,应对其持谨慎态度。本研究的临床选择标准是单发病灶,原则上肿瘤原发灶<5 cm,无广泛沙粒样钙化灶存在的I~II期的乳腺癌,患者依从性好,无放疗禁忌症,但未对年龄加以严格的限制。
3.5 术后并发症及美容效果
整形保乳术后并发症的包括皮瓣坏死、NAC坏死、血肿形成、感染、皮下积液、伤口裂开等。Calì Cassi等[17]的研究显示,整形保乳术的术后并发症发生率稍高于传统保乳术组。有文献[4]显示严重并发症的出现可能会导致辅助治疗延迟,而Klit等[27]则认为乳腺肿瘤整形手术并没有延迟术后化疗的开始。本组资料术后并发症发生率为18.0%(25/139),无皮瓣及NAC坏死等严重并发症发生,均未延迟患者的辅助治疗。本组资料美容效果评定结果为:优秀79例(56.8%),良好47例(33.8%),一般10例(7.2%),差3例(2.2%)。满意率为90.6%,对于术后美容效果欠佳的患者,可以通过多次局部脂肪填充、乳头再造及乳晕刺青等方式加以改善。
参考文献
[1] Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013[J]. CA Cancer J Clin, 2013, 63(1):11–30. doi: 10.3322/caac.21166.
[2] Litière S, Werutsky G, Fentiman IS, et a1. Breast conserving therapy versus mastectomy for stage I-II breast cancer: 20 year follow-up of the EORTC 10801 phase 3 randomised trial[J]. Lancet Oncol, 2012, 13(4):412–419. doi: 10.1016/S1470–2045(12)70042–6.
[3] van Maaren MC, de Munck L, de Bock GH, et al. 10 year survival after breast-conserving surgery plus radiotherapy compared with mastectomy in early breast cancer in the Netherlands: a populationbased study[J]. Lancet Oncol, 2016, 17(8):1158–1170. doi: 10.1016/S1470–2045(16)30067–5.
[4] Rose M, Manjer J, Ringberg A, et al. Surgical strategy, methods of reconstruction, surgical margins and postoperative complications in oncoplastic breast surgery[J]. Eur J Plast Surg, 2014, 37:205–214.
[5] Lee JW, Kim MC, Park HY, et al. Oncoplastic volume replacement techniques according to the excised volume and tumor location in small- to moderate-sized breasts[J]. Gland Surg, 2014, 3(1):14–21.doi: 10.3978/j.issn.2227–684X.2014.02.02.
[6] Park HC, Kim HY, Kim MC, et al. Partial breast reconstruction using various oncoplastic techniques for centrally located breast cancer[J]. Arch Plast Surg, 2014, 41(5):520–528. doi: 10.5999/aps.2014.41.5.520.
[7] Chen DR. An optimized technique for all quadrant oncoplasty in women with small- to medium-sized breasts [J]. Eur Rev Med Pharmacol Sci, 2014, 18(12):1748–1754.
[8] 刘安阳, 王会元, 王晓辉, 等. 乳腺癌保留乳房肿瘤整形术合并同期健侧乳房对称性整形手术10例分析[J]. 中华乳腺病杂志:电子版, 2015, 9(2):127–133. doi:10.3877/cma.j.issn.1674–0807.2015.02.014.Liu AY, Wang HY, Wang XH, et al. Oncoplastic breast-conserving breast cancer surgery with synchronous synchronous contralateral symmetry mammoplasty: an analysis of 10 cases[J]. Chinese Journal of Breast Disease: Electronic Version, 2015, 9(2):127–133.doi:10.3877/cma.j.issn.1674–0807.2015.02.014.
[9] 于芷晗, 常铁君, 曲岩, 等. 整形外科技术在早期乳腺癌保乳手术中的临床应用[J]. 医学与哲学, 2016, 37(4):51–52. doi:10.12014/j.issn.1002–0772.2016.02b.16.Yu ZH, Chang TJ, Qu Y, et al. Application of Plastic Surgery Technique in Breast Conserving Surgery for Early Breast Cancer Patients[J]. Medicine & Philosophy, 2016, 37(4):51–52.doi:10.12014/j.issn.1002–0772.2016.02b.16.
[10] 黄蕴, 卓睿, 凌文津, 等. 肿瘤整形技术在103例中小乳房乳腺癌保乳术中的应用初探[J]. 广西中医药大学学报, 2014, 17(2):46–48.Huang Y, Zhuo R, Ling WJ, et al. Preliminary study of using oncoplastic techniques in 103 breast cancer patients with small breasts[J]. Journal of Guangxi University of Chinese Medicine,2014, 17(2):46–48.
[11] 胡小戊, 章乐虹, 夏婷, 等. 肿瘤整形术联合背阔肌肌皮瓣在中-小型外侧象限乳腺癌保乳重建中的应用体会[J]. 岭南现代临床外科, 2015, 15(1):22–26. doi:10.3969/j.issn.1009–976X.2015.01.005.Hu XW, Zhang LH, Xia T, et al. Oncoplastic reconstruction combined with latissimus dorsi myocutaneous flap after lateral quadrant tumor resection in small to moderate-sized breasts[J].Lingnan Modern Clinics in Surgery, 2015, 15(1):22–26.doi:10.3969/j.issn.1009–976X.2015.01.005.
[12] 王文彦, 王昕, 王阳, 等. 肿瘤整形外科技术应用于早期乳腺癌保乳手术的临床分析[J]. 癌症进展, 2015, 13(6):627–631.doi:10.11877/j.issn.1672–1535.2015.13.06.14.Wang WY, Wang X, Wang Y, et al. Clinical analysis of oncoplastic surgical techniques applied in breast-conserving surgery of early stage breast cancer[J]. Oncology Progress, 2015, 13(6):627–631.doi:10.11877/j.issn.1672–1535.2015.13.06.14.
[13] Chang EI, Peled AW, Foster RD, et a1. Evaluating the feasibility of extended partial mastectomy and immediate reduction mammoplastry reconstruction as an alternative to mastectomy[J]. Ann Surg, 2012, 255(6):1151–1157. doi: 10.1097/SLA.0b013e31824f9769.
[14] Fitoussi A, Berry MG, Couturaud B, et a1. Oncoplastic and Reconstructive Surgery for Breast Cancer[M]. France: Springer-Verlag. 2009:41.
[15] Carter SA, Lyons GR, Kuerer HM, et al. Operative and Oncologic Outcomes in 9861 Patients with Operable Breast Cancer: Single-Institution Analysis of Breast Conservation with Oncoplastic Reconstruction[J]. Ann Surg Oncol, 2016, 23(10):3190–3198. doi:10.1245/s10434–016–5407–9.
[16] Mansell J, Weiler-Mithoff E, Stallard S, et al. Oncoplastic breast conservation surgery is oncologically safe when compared to wide local excision and mastectomy[J]. Breast, 2017, 32:179–185. doi:10.1016/j.breast.2017.02.006.
[17] Calì Cassi L, Vanni G, Petrella G, et al. Comparative study of oncoplastic versus non-oncoplastic breast conserving surgery in a group of 211 breast cancer patients[J]. Eur Rev Med Pharmacol Sci,2016, 20(14):2950–2954.
[18] De La Cruz, Blankenship SA, Chatterjee A, et al. Outcomes After Oncoplastic Breast-Conserving Surgery in Breast Cancer Patients:A Systematic Literature Review[J]. Ann Surg Oncol, 2016,23(10):3247–3258. doi: 10.1245/s10434–016–5313–1.
[19] Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer[J]. N Engl J Med, 2002, 347(16):1233–1241.
[20] Veronesi U, Cascineli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer[J]. N Engl J Med 2002,347(16):1227–1232.
[21] Association of Breast Surgery at BASO, Association of Breast Surgery at BAPRAS, Training Interface Group in Breast Surgery,et a1. Oncoplastic breast surgery-a guide to good practice[J]. Eur J Surg Oneol, 2007, 33(Suppl 1):S1–23.
[22] Iwuchukwu OC, Harvey JR, Dordea M, e t al. The role of oncoplastic therapeutic mammoplasty in breast cancer surgery-a review[J]. Surg Oncol, 2012, 21(2):133–141. doi: 10.1016/j.suronc.2011.01.002.
[23] 尹健. 肿瘤整形外科在乳腺肿瘤治疗中的应用[J]. 中华普通外科学文献: 电子版, 2013, 7(4):255–257. doi:10.3877/cma.j.issn.1674–0793.2013.04.003.Yin J. Application of oncoplastic surgery in treatment of breast neoplasms[J]. Chinese Archives of General Surgery:Electronic Edition, 2013, 7(4):255–257. doi:10.3877/cma.j.issn.1674–0793.2013.04.003.
[24] Vieira RA, Carrara GF, Scapulatempo Neto C, et al. The role of oncoplastic breast conserving treatment for locally advanced breast tumors. A matching case-control study [J]. Ann Med Surg (Lond),2016, 10:61–68. doi: 10.1016/j.amsu.2016.08.001.
[25] Chirappapha P, Kongdan Y, Vassanasiri W, et al. Oncoplastic technique in breast conservative surgery for locally advanced breast cancer[J]. Gland Surg, 2014, 3(1):22–27. doi: 10.3978/j.issn.2227–684X.2014.01.01.
[26] Klit A, Tvedskov TF, Kroman N, et al. Oncoplastic breast surgery does not delay the onset of adjuvant chemotherapy: a population-based study[J]. Acta Oncol, 2017, 56(5):719–723. doi:10.1080/0284186X.2017.1281437.
