缺乏远端流出道的股腘动脉狭窄或闭塞病变在下肢动脉硬化闭塞症中较为常见且治疗难度大,尤其是糖尿病下肢缺血患者[1-5]。对于以重度间歇跛行为主要症状的该类病变患者如果片面追求开通膝下动脉往往存在手术时间增加、对比剂用量及射线暴露时间增加,而临床收益不大的顾虑,尤其对于高危患者;如果不开通膝下动脉则存在只能应用单纯球囊扩张、中远期疗效差的弊端[6-8]。斑块切除术可以切除靶血管内的硬化斑块恢复管腔的通畅性[9];同时因无异物的植入对于远端流出道的要求较低。斑块切除术在治疗缺乏远端流出道的股腘动脉狭窄/闭塞病变中具有一定的优势。
首都医科大学宣武医院血管外科2014年7月—2015年6月应用斑块切除术治疗以重度间歇跛行为主要症状,靶血管病变为缺乏远端流出道的股腘动脉狭窄患者21例,并进行随访,现报告如下。
1 资料与方法
1.1 一般资料
我科从2014年7月—2015年6月治疗以重度间歇跛行(跛行距离<200 m)为主要症状、靶血管病变为股腘动脉重度狭窄、膝下缺乏远端流出道(胫前、胫后及腓动脉均闭塞)的患者21例。术前通过下肢动脉CTA或血管造影证实腹主及髂动脉正常或轻度狭窄;股浅动脉远段重度狭窄(8例)、腘动脉重度狭窄(13例)。 本组患者男15例,女6例;年龄72~81岁,平均(75.4±3.5)岁;均为动脉硬化闭塞性疾病患者,其中合并糖尿病17例,合并高血压12例,合并高脂血症12例,吸烟11例。
1.2 方法
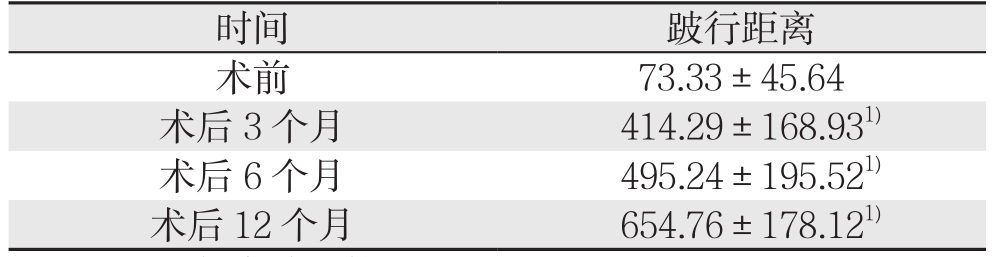
同侧股总动脉顺行穿刺,经造影证实病变部位及程度(图1),导丝通过病变部位。 路图下应用L型斑块切除导管 (SilverHawk)对病变部位进行多角度切除(图2),切除完毕退出斑块切除导管后造影(图3),改换投照角度90°后再次造影,证实靶血管残余狭窄<30%后结束手术 。由于本组患者均为无远端流出道,不存在远端主干流出道栓塞可能,故均未使用远端保护装置。本组出现靶血管夹层2例,但均未限制血流及未造成管腔明显狭窄,其中1例采用普通球囊低压成形;未出现靶血管急性血栓形成及闭塞。患者术前3 d开始应用拜阿司匹林100 mg,每天1次,术后应用低分子肝素或普通肝素进行抗凝3 d,长期服用拜阿司匹林。术后第2天复查踝肱指数(ankle/brachial index,ABI),术后3、6、12个月门诊随访,记录跛行距离并复查ABI和血管超声。
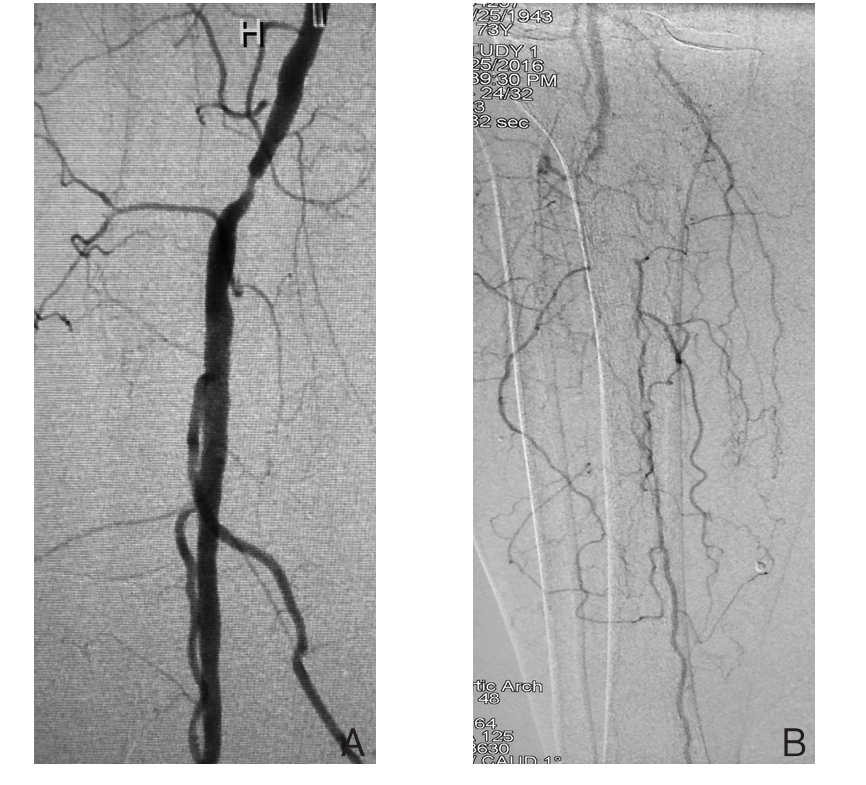
图1 术前DSA A:腘动脉P1段重度狭窄;B:膝下3支动脉均闭塞
Figure 1 Preoperative DSA images A: Severe stenosis in P1 segment of the popliteal artery; B: Occlusion of all three infrapopliteal arteries

图2 应用斑块切除导管进行斑块切除
Figure 2 Atherectomy with an atherectomy catheter
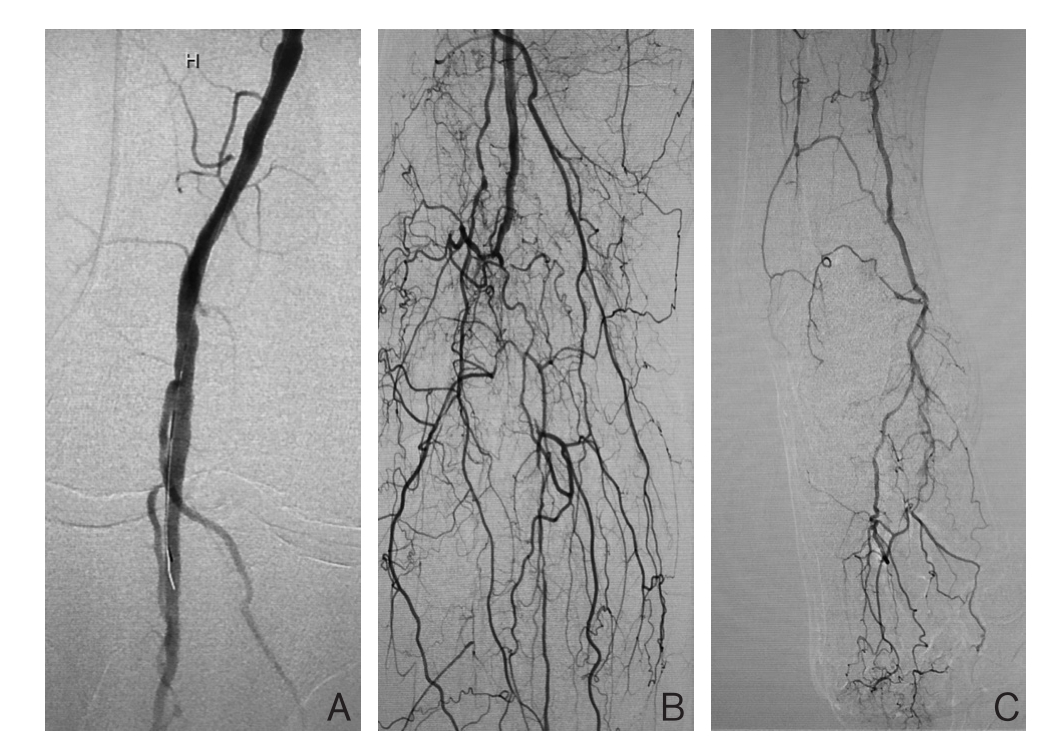
图3 术后DSA A:腘动脉狭窄消失;B:膝下侧枝血管显影较术前丰富;C:胫后动脉远端主干显影及流速明显改善
Figure 3 Postoperative DSA images A: Disappearance of the stenosis in the popliteal artery; B: Presence of more abundant infrapopliteal branches than that before operation; C: Presence of the distal main trunk of the posterior tibial artery and significantly improvedflow velocity
2 结 果
2.1 跛行距离变化
本组21例患者均接受术后12个月随访。患者术后3、6、12个月跛行距离较术前均明显且逐渐增加,差异均有统计学意义(均P<0.05)(表1)。
表1 患者不同时间跛行距离(m, ±s)
±s)
Table 1 Claudication distances of the patients at different timer points (m,  ±s)
±s)
注:1)与术前比较,P<0.05
Note: 1) P<0.05 vs. preoperative value
2.2 ABI的变化
患者术后第2天及3、6、1 2个月的A B I较术前均明显增加,具差异均有统计学意义(均P<0.05)(表2)。
表2 患者不同时间ABI( ±s)
±s)
Table 2 The ABI values of the patients at different time points( ±s)
±s)
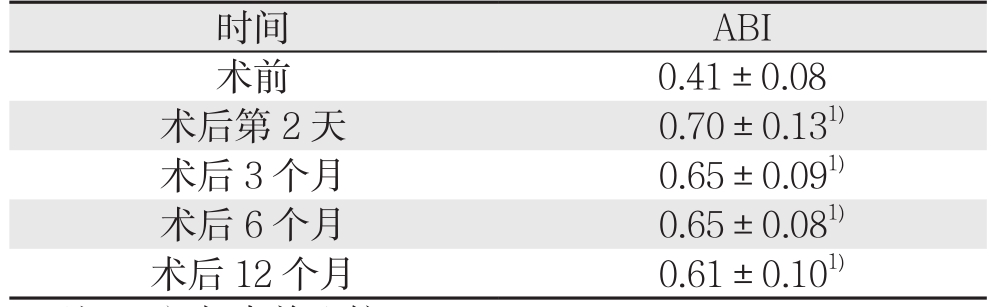
注:1)与术前比较,P<0.05
Note:1) P<0.05 vs. preoperative value
2.3 靶血管通畅情况
术后3、6、12个月进行门诊随访复查血管超声。术后3个月无靶血管再狭窄,术后6个月发现靶血管再狭窄1例(1/21),术后12个月发现靶血管再狭窄2例(包括术后6个月再狭窄1例)(2/21),为中度再狭窄,患者间歇跛行距离无明显缩短,未予外科干预,密切随访。
3 讨 论
在下肢缺血患者的诊治过程中,是否进行外科干预及治疗方式的选择主要取决于患者的症状[10]。如果患者表现为肢体的溃疡或坏疽,首先要处理可能存在的髂、股、腘动脉等近端病变,若存在膝下动脉病变则要按照Angiosome概念进行膝下动脉的重建[11];如果患者表现为静息痛,也应该尽量开通膝下动脉,改善患者的肢体重度缺血;而对于以间歇跛行为主要症状的患者,改善存在的股腘动脉病变即达到症状缓解的目的,而追求膝下动脉重建则会增加手术时间、增加射线暴露、增加对比剂用量,尤其对于高龄、慢性肾功能不全等高危患者开通膝下动脉复杂病变的确存在一定的风险。
流出道在动脉腔内治疗中的意义众所周知[12],流出道往往决定腔内治疗方式的选择及腔内治疗的成败。对于缺乏良好流出道的股腘动脉狭窄或闭塞病变腔内治疗疗效差,采用股腘动脉单纯球囊成形通畅率低,而支架成形则是必须避免的[13-14],临床中因流出道差而导致支架早期血栓形成或闭塞的病例并不罕见。而斑块切除术因无异物的植入对于远端流出道的要求较低。
斑块切除术是采用腔内技术,应用斑块切除导管,切除动脉腔内的动脉硬化斑块或增生的内膜组织的一种腔内治疗方式[15-17]。目前较为常用的斑块切除导管主要有两种,分别为SilverHawk和TurboHawk斑块切除导管 。本组在研究期间可应用的斑块切除导管为SilverHawk,故患者均采用SilverHawk进行腔内斑块切除;两种斑块切除导管无论在产品设计和应用上具有一定的区别,尤其在处理严重钙化病变方面,TurboHawk较SilverHawk更具有优势,对于钙化严重病变要优先选择TurboHawk。腔内斑块切除技术在具体应用过程中首先要通过改变投照角度充分显露病变,然后根据靶血管直径选择合适规格的斑块切除导管,对于钙化严重病变、单支流出道病变和可疑存在血栓病变要应用远端保护装置。斑块切除过程中要注意多角度、多节段切除,切除后更换投照角度确认有无残留病变,必要时再次切除该节段,直至造影证实无明显残余狭窄或残余狭窄<30%、无限制血流夹层、无远端动脉栓塞[2,18-21]。腔内斑块切除术在腔内治疗中具有一定的优势,表现为:在多数病例可以避免支架的植入,尤其对于关节部位这点优势尤为突出;对于闭塞段靶血管可以最大限度的保留侧枝;斑块切除术通过高效效的管腔减容,能够提高后续药物涂层球囊应用后靶血管的通畅率 [22-24]。
对于以重度间歇跛行为主要症状、缺乏远端流出道的股腘动脉狭窄病变如果采用斑块切除术既可以减少开通膝下流出道所带来的风险(尤其对于部分高危患者),又改善了远端组织的灌注,还可以开通潜在的侧枝/分支血管,更主要的是避免了支架的植入及其后续支架近期血栓形成或闭塞的可能。本文总结的病例初步证实了斑块切除治疗该类型病变的优势,在目前文献中未见相关研究,但斑块切除后靶血管的远期通畅率及长期效果有待进一步证实。当然,远端流出道的情况对斑块切术后靶血管通畅率的影响有待进一步随访和临床研究。
参考文献
[1]Zeller T, Rastan A, Sixt S, et al. Long-term results after directional atherectomy of femoro-popliteal lesions[J]. J Am Coll Cardiol,2006, 48(8):1573–1578.
[2]McKinsey JF, Goldstein L, Khan HU, et al. Novel treatment of patients with lower extremity ischemia: use of percutaneous atherectomy in 579 lesions[J]. Ann Surg, 2008, 248(4):519–528.doi: 10.1097/SLA.0b013e318188e1de.
[3]丁明超, 李芳, 王斌, 等. 无流出道显影的下肢动脉闭塞症腔内血管成形治疗的预探索[J]. 介入放射学杂志, 2015, 24(5):383–387.doi:10.3969/j.issn.1008–794X.2015.05.005.Ding MC, Li F, Wang B, et al. Percutaneous endovascular angioplasty for the treatment of arteriosclerosis obliterans of the lower extremities showing no outflow tract visualization: a preliminary exploration[J]. Journal of Interventional Radiology,2015, 24(5):383–387. doi:10.3969/j.issn.1008–794X.2015.05.005.
[4]谷涌泉. 下肢动脉硬化闭塞症腔内治疗的新进展[J]. 中国普通外科杂志, 2014, 23(6):719–723. doi:10.7659/j.issn.1005–6947.2014.06.002.Gu YQ. Endovascular treatment for arteriosclerosis obliterans of lower extremities: resent advances[J]. Chinese Journal of General Surgery, 2014, 23(6):719–723. doi:10.7659/j.issn.1005–6947.2014.06.002.
[5]Klein AJ, Ross CB. Endovascular treatment of lower extremity peripheral arterial disease[J]. Trends Cardiovasc Med, 2016,26(6):495–512. doi: 10.1016/j.tcm.2016.02.007.
[6]牛国晨, 邹英华. 腔内血管成形术治疗膝下动脉缺血性疾病[J].中国介入影像与治疗学, 2010, 7(2):196–199.Niu GC, Zou YH. Endovascular therapy in the treatment of infrapopliteal arterial occlusive disease[J]. Chinese Journal of Interventional Imaging and Therapy, 2010, 7(2):196–199.
[7]谷涌泉, 郭建明. 糖尿病膝下动脉病变腔内治疗的新进展[J]. 中国微创外科杂志, 2017, 17(4):289–293. doi:10.3969/j.issn.1009–6604.2017.04.001.Gu YQ, Guo JM. Noval Progress of Endovascular Treatment of Diabetic Below Knee Arteries Lesions [J]. Chinese Journal of Minimally Invasive Surgery, 2017, 17(4):289–293. doi:10.3969/j.issn.1009–6604.2017.04.001.
[8]Kokkinidis DG, Armstrong EJ. Emerging and Future Therapeutic Options for Femoropopliteal and Infrapopliteal Endovascular Intervention[J]. Interv Cardiol Clin, 2017, 6(2):279–295. doi:10.1016/j.iccl.2016.12.011.
[9]谷涌泉, 郭连瑞, 齐立行, 等. SilverHawk斑块切除治疗动脉粥样硬化导致的下肢缺血14例报告[J]. 中国微创外科杂志, 2011,11(11):1022–1024. doi:10.3969/j.issn.1009–6604.2011.11.021.Gu YQ, Guo LR, Qi LX, et al. Plaque Excision with SilverHawk Treating Atherosclerotic Lower Extremity Ischemia: Report of 14 Cases[J]. Chinese Journal of Minimally Invasive Surgery, 2011,11(11):1022–1024. doi:10.3969/j.issn.1009–6604.2011.11.021.
[10]Hicks CW, Najafian A, Farber A, et al. Diabetes does not worsen outcomes following infrageniculate bypass or endovascular intervention for patients with critical limb ischemia[J]. J Vasc Surg.2016, 64(6):1667–1674. doi: 10.1016/j.jvs.2016.07.107.
[11]Shishehbor MH, Jaff MR. Percutaneous Therapies for Peripheral Artery Disease[J]. Circulation, 2016, 134(24): 2008–2027.
[12]Ballotta E, Toniato A, Piatto G, et al. Lower extremity arterial reconstruction for critical limb ischemia in diabetes[J]. J Vasc Surg.2014, 59(3):708–719. doi: 10.1016/j.jvs.2013.08.103.
[13]胡骥琼, 王道明, 司春强, 等. 下肢动脉硬化闭塞症侧支循环流出道的解剖学特点及临床应用初探[J]. 中国修复重建外科杂志,2008, 22(5):571–574.Hu JQ, Wang DM, Si CQ, et al. Anatomy and clinical application of bypass circuit outflow tract of arterial sclerosis obstruction[J].Chinese Journal of Reparative and Reconstructive Surgery, 2008,22(5):571–574.
[14]Tsetis D, Belli AM. The role of infrapopliteal angioplasty[J]. Br J Radiol, 2004, 77(924):1007–1015.
[15]Shammas NW, Lam R, Mustapha J, et al. Comparison of orbital atherectomy plus balloon angioplasty vs. balloon angioplasty alone in patients with critical limb ischemia: results of the CALCIUM 360 randomized pilot trial[J]. J Endovasc Ther, 2012, 19(4):480–488.doi: 10.1583/JEVT–12–3815MR.1.
[16]Bunting TA, Garcia LA. Peripheral atherectomy: a critical review[J]. J Interv Cardiol, 2007, 20(6):417–424.
[17]Shafique S, Nachreiner RD, Murphy MP, et al. Recanalization of infrainguinal vessels: silverhawk, laser, and the remote superficial femoral artery endarterectomy[J]. Semin Vasc Surg, 2007, 20(1):29–36.
[18]Keeling WB, Shames ML, Stone PA, et al. Plaque excision with the Silverhawk catheter: early results in patients with claudication or critical limb ischemia[J]. J Vasc Surg, 2007, 45(1):25–31.
[19]Shrikhande GV, McKinsey JF. Use and abuse of atherectomy: where should it be used?[J]. Semin Vasc Surg, 2008, 21(4):204–209. doi:10.1053/j.semvascsurg.2008.11.007.
[20]Lin S, McKinsey JF. Plaque excision for the treatment of infrainguinal arterial occlusive disease[J]. Tech Vasc Interv Radiol,2005, 8(4):165–168.
[21]Rubin BG. Plaque excision in the treatment of peripheral arterial disease[J]. Perspect Vasc Surg Endovasc Ther, 2006, 18(1):47–52.
[22]郭建明, 谷涌泉, 郭连瑞, 等. Silverhawk斑块切除成形治疗严重膝下动脉硬化闭塞性病变[J]. 中国普通外科杂志, 2014,23(6):732–736. doi:10.7659/j.issn.1005–6947.2014.06.005.Guo JM, Gu YQ, Guo LR, et al. Silverhawk atherectomy and adjunctive angioplasty for severe arterial atherosclerotic occlusive disease below the knee[J]. Chinese Journal of General Surgery,2014, 23(6):732–736. doi:10.7659/j.issn.1005–6947.2014.06.005.
[23]谷涌泉, 郭连瑞, 佟铸, 等. SilverHawk治疗长段股总动脉和股浅动脉支架内再狭窄一例[J]. 中华普通外科杂志, 2011, 26(3):265–266. doi:10.3760/cma.j.issn.1007–631X.2011.03.037.Gu YQ, Guo LR, Tong Z, et al. SilverHawk treatment for one case with long-segment stenosis of the common femoral artery and instent restenosis of the superficial femoral artery[J]. Zhong Hua Pu Tong Wai Ke Za Zhi, 2011, 26(3):265–266. doi:10.3760/cma.j.issn.1007–631X.2011.03.037.
[24]Gu Y, Malas MB, Qi L, et al. A comparative study of percutaneous atherectomy for femoropopliteal arterial occlusive disease:experiences in 160 patients[J]. Int Angiol, 2017, doi: 10.23736/S0392–9590.17.03797–X. [Epub ahead of print]]
