肝囊性淋巴管瘤为临床罕见的肝良性肿瘤,成人肝巨大囊性淋巴管瘤更为罕见[1]。肝囊性淋巴管瘤临床表现及影像学表现无特征性,临床易误诊。现总结我科收治的2例成人肝囊性淋巴管瘤患者的临床资料,同时结合国内相关文献报道情况对该病的发病特点、临床表现及诊疗方法进行总结分析,旨在提高大家对成人肝囊性淋巴管瘤的诊疗水平。
1 临床资料
病例1 女性,40岁,因“无症状性腹部膨隆半个月”入院。既往史:否认有外伤、高血压、糖尿病、肝炎及结核等传染病。家族史:父亲30多年前因胃癌去逝;母亲20多年前因胰腺癌去逝。入院血常规、生化检查及肿瘤学标志物:AFP、CA19-9、CEA均正常。乙肝表面抗原(HBsAg)阴性。彩色多普勒超声:上腹部巨大囊性占位,性质待定,宫颈囊肿。CT:中上腹巨大多房囊状低密度影,考虑为良性病变,囊腺瘤可能性大,来源倾向肝脏,不除外来源于胰腺或肠系膜。完善相关检查,排除手术禁忌证后全麻下行剖腹探查:行上腹正中绕脐切口,切开各层探查腹腔,未见腹水,肝质地正常,囊性肿物有完整包膜,向外呈膨胀性生长,大小约为18 cm×22 cm,由肝脏面向下生长,囊壁表面可见扩张血管,囊壁薄、透亮,有分房;囊肿占据整个右侧腹腔,囊肿底端下至右侧髂前上棘平面,肠管被挤向左侧腹腔;向上分离粘连,见囊肿来源于肝脏,根部位于右肝脏面,胆囊窝右侧。囊肿与胆囊、十二指肠球部及胃窦部有粘连;因囊肿与胆囊粘连严重无法分离,为确保囊肿完整切除,遂切除胆囊。在距囊肿根部切除0.5 cm肝组织后,整体移走标本。术中切开囊壁,约有3 200 mL淡黄色液体流出,探查囊内壁呈乳白色,内膜光滑,未见结节。标本送术中冷冻检查,提示肝脏良性病变,遂放置引流管关腹术毕。送检囊液Rivalta试验阳性、细菌培养阴性及囊液离心未找到癌细胞。术后行抗感染、护肝对症治疗,患者恢复良好,术后8 d拆线,痊愈出院。术后病理提示:肝巨大囊性占位,结合免疫组化结果符合肝巨大囊性淋巴管瘤。免疫组化结果:CD31(+)、D2-40(+)、Vimentin(+)、CK5/(-)、MC(-)/CR(-);慢性胆囊炎。术后患者随访至2016年10月15日,ALT 11.8 U/L,AST 7.2 U/L,TBIL 5.3 μmmol/L;彩色多普勒超声提示:肝脏形态正常,胆囊缺如,胆总管内径0.8 cm,盆腔少量积液,前后径约为2.0 cm;术后恢复满意,未见复发。患者术前CT及术后病理见图1-2。
病例2 女性,41岁,因“体检发现胆囊息肉1年”入院。患者1年前彩色多普勒超声体检提示胆囊多发息肉(最大为0.5 cm×0.6 cm),肝囊性占位:肝囊肿。后因复查发现息肉进行性增大,遂住院治疗。患者否认有外伤、肝炎及结核等传染病,无家族性肿瘤病史。入院血常规、生化检查及肿瘤学标志物:AFP、CA19-9、CEA均正常。乙肝表面抗原(HBsAg)阴性。腹部彩色多普勒超声:提示胆囊多发息肉;肝左外叶无回声区大小约为3.0 cm×2.0 cm,考虑肝囊肿。完善相关检查,排除手术禁忌证后在全麻下行腹腔镜胆囊切除+左外叶部分切除术(术中见胆囊形态、大小正常,壁不厚,切开胆囊见内壁数块隆起物,最大直径约为1 cm;肝囊性肿物位于S2段,肝边缘处,部分囊壁位于膈面,遂沿囊肿壁1.0 cm行肝部分切除,切开标本囊内有淡黄色清亮的液体约5 mL,囊壁完整光滑、色白;术后行抗感染、护肝对症治疗,患者恢复良好,术后2 d,痊愈出院。术后病理提示:慢性胆囊炎并发性胆固醇性息肉;肝囊性占位,结合免疫组化结果符合肝囊性淋巴管瘤。免疫组化结果:CD31(+),D2-40(+),CK5/6(-),Vimentin(+),MC(-)/CR(-)。术后患者随访至2017年3月17日,ALT 18.6 U/L,AST 28.9 U/L,TBIL 15.3 μmmol/L,彩色多普勒超声提示:肝脏形态正常,胆囊及肝左外叶部分缺如,胆总管内径0.7 cm;术后恢复满意。患者手术前彩超及术后病理见图3-4。
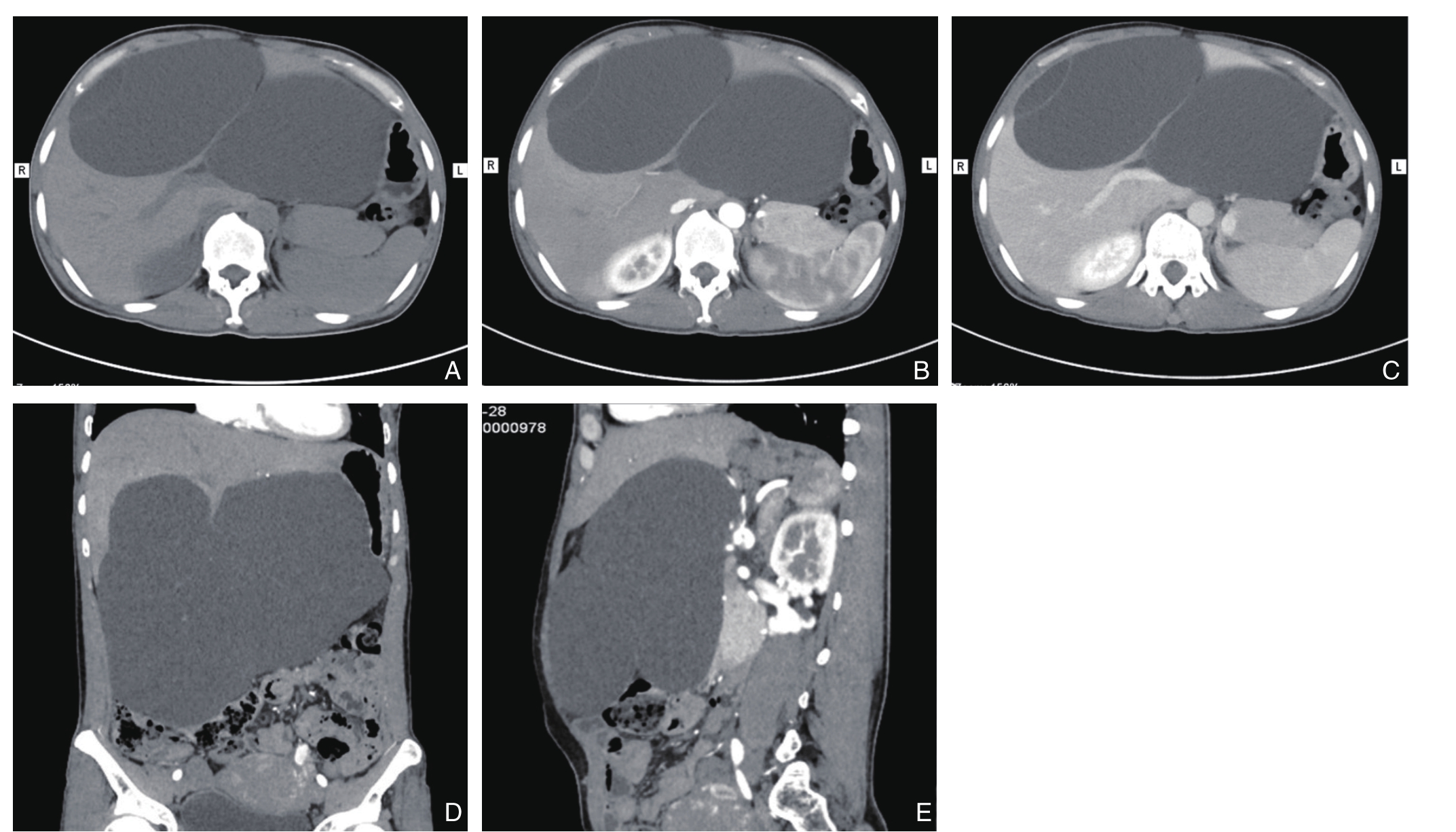
图1 病例1术前CT图像
A:平扫;B:动脉期扫描;C:门脉期扫描;D:冠状位像;E:矢状位像
Figure 1 Preoperative CT images of case 1
A: Plain scan image; B: Arterial phase image; C: Portal phase image; D: Coronal plane image;E: Sagittal plane image
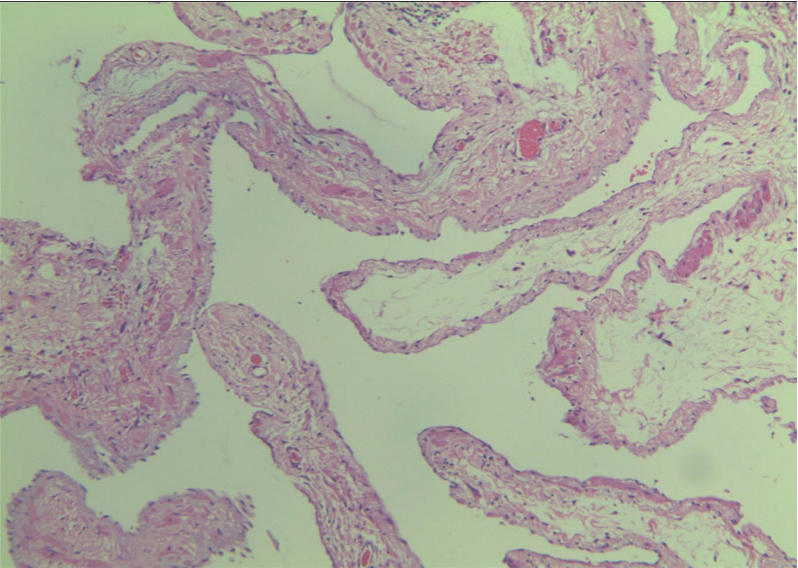
图2 病例1病理结果(HE×100)
Figure 2 Pathological results of case 1(HE×100)
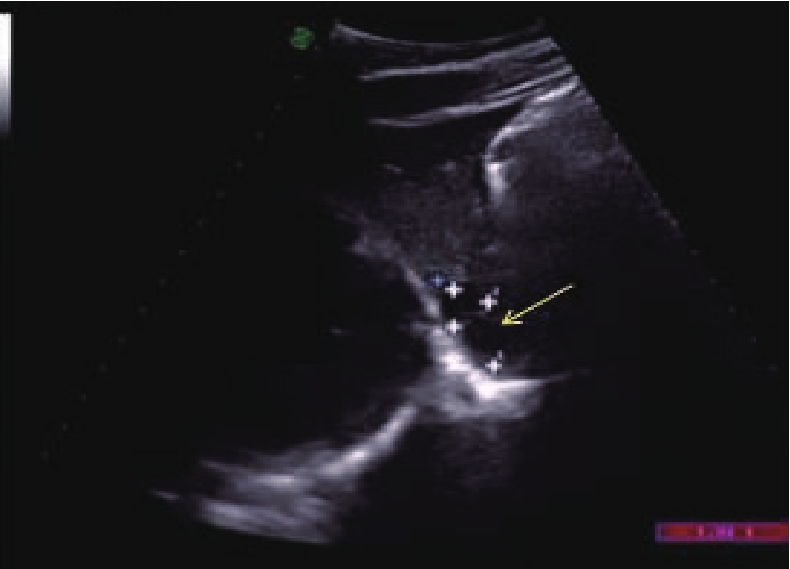
图3 病例2腹部彩色多普勒超声图
Figure 3 Abdominal ultrosonography of case 2
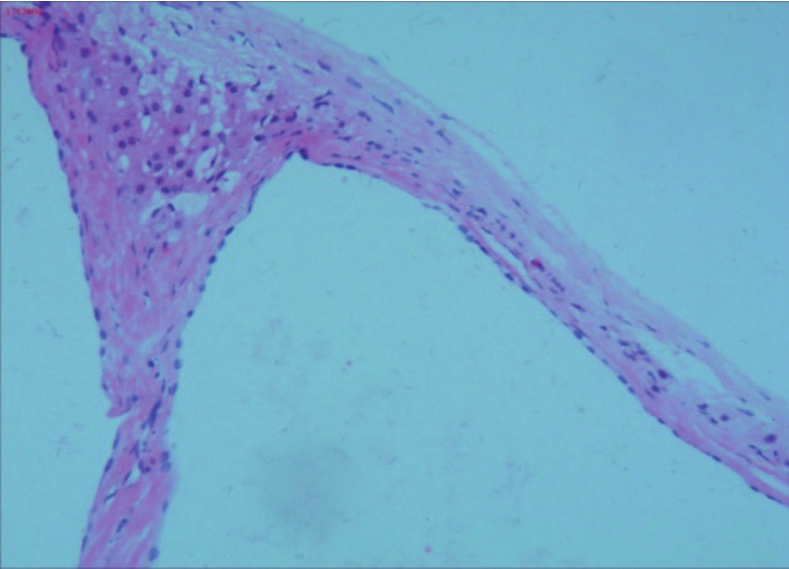
图4 病例2病理结果(HE×100)
Figure 4 Pathological results of case 2 (HE×100)
2 文献复习
同时检索1984年1月—2017年1月31日期间中国期刊数据库(包括CNKI、万方及维普)中关于肝淋巴管的临床研究文献,排除其中重复报道、资料不全的文章 ,通过阅读,最终入选6篇文献[2-7]共6例患者,进行分析总结。
6例肝囊性淋巴管瘤患者中,男4例(66.7%),女2例(33.3%),男女比例为2.0:1.0。发病年龄4个月~60岁,平均年龄(39.2±25.4)岁。发病时间最短4 h,最长达7年。6例患者临床表现各不相同,有因腹痛或发现腹部膨隆来就诊,也有因其他原因导致急腹症手术探查意外发现,其中,腹痛(2/6)、腹胀(2/6)、发热(1/6)、消化道出血(1/6)、治疗其他疾病偶然发现(1/6)。
6例中,入院诊断肝囊淋巴管瘤2例(2/6,33.3%),其他均误诊(4/6,66.7%),常见误诊为肝囊肿、肝囊腺瘤、肝囊腺癌及Caroli病等肝内囊性占位。
6例患者均行肝切除术并明确病理,有不适症状及体征的患者术后不适症状消失,治疗效果满意。6例患者中仅有3位患者提及术后随访,其中1例因进行性腹胀,进食差,消瘦,术后14个月死于营养障碍[2];其余2例随访10~12个月,淋巴管瘤无复发,治疗满意。回顾文献6例患者的情况见表1。
表1 回顾文献6例患者临床资料
Table 1 Clinical data of the reported 6 patients
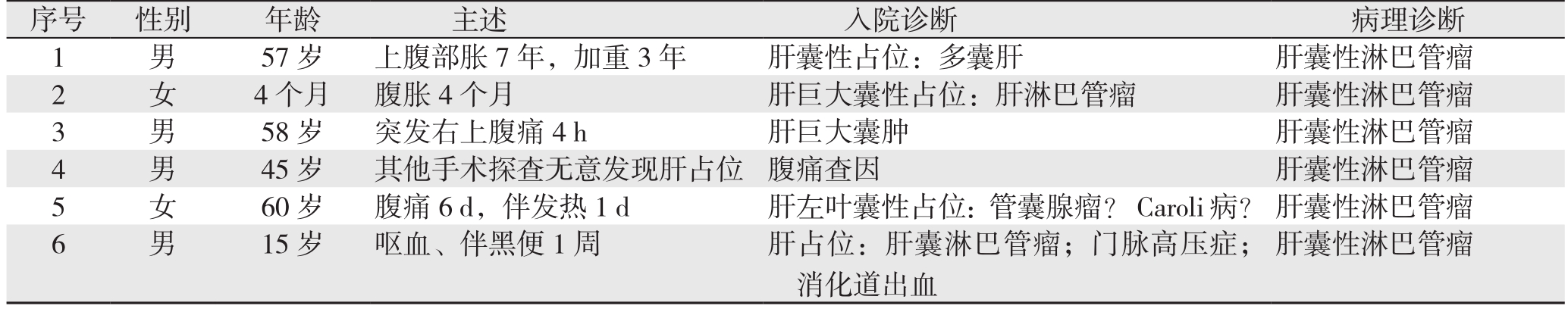
序号 性别 年龄 主述 入院诊断 病理诊断1 男 57岁 上腹部胀7年,加重3年 肝囊性占位:多囊肝 肝囊性淋巴管瘤2 女 4个月 腹胀4个月 肝巨大囊性占位:肝淋巴管瘤 肝囊性淋巴管瘤3 男 58岁 突发右上腹痛4 h 肝巨大囊肿 肝囊性淋巴管瘤4 男 45岁 其他手术探查无意发现肝占位 腹痛查因 肝囊性淋巴管瘤5 女 60岁 腹痛6 d,伴发热1 d 肝左叶囊性占位:管囊腺瘤?Caroli病?肝囊性淋巴管瘤6 男 15岁 呕血、伴黑便1周 肝占位:肝囊淋巴管瘤;门脉高压症;消化道出血肝囊性淋巴管瘤
3 讨 论
淋巴管瘤通常被认为是淋巴系统的先天性畸形,病因仍不清楚,大多发生在颈部、纵隔及腹膜后,很少发生在肝脏、脾脏、肾及胃肠道等[1,8-12]。肝淋巴管瘤在组织学上可分为毛细管型淋巴管瘤,海绵状淋巴管瘤和囊性淋巴管瘤3种,后者最多[13]。其中肝囊性淋巴瘤多见于婴幼儿,多呈为圆形、卵圆形或分叶状,囊壁薄厚不一,镜下可见淋巴管结构[14]。
肝囊性淋巴管瘤的临床无特异性。临床表现主要与肿瘤大小、增长的速度及不同的病变类型有关[1,8-10]。临床主要表现为无痛性包块、腹部胀闷或胀痛,多因囊肿压缩周围结构引起。若囊肿并发内感染或出血时[15],会出现急性腹痛。当突发腹痛、发热则考虑是囊肿破裂囊液外溢导致急性腹膜炎。如果淋巴管瘤压迫肝门区胆管时会出现黄疸等肝功能损害的症状。本文笔者收治患者因囊肿巨大出现腹部膨隆来就诊。回顾文献6例患者,有2例因腹痛、腹胀就诊,1例急性腹膜炎术中探查意外发现肝占位,切除后病理诊断为肝囊性淋巴管瘤。还有1例肝尾叶淋巴管瘤因压迫下腔静脉、门静脉继发引起门静脉海绵样变性出现呕血来就诊[6]。
病理检查被认为是诊断肝囊性淋巴管的唯一方法,结合淋巴管内皮细胞特异性抗体D2-40及CD31检测有助于进一步明确诊断[11,13,16]。病理学穿刺是否作为明确病理首先,存在争议。秦颖等[17]认为超声引导下经皮细针肝穿刺术是一种简便、快捷、安全的检查方法。然而,Liu等[10]认为病理学穿刺阳性率低,且存在出血和种植转移的可能。影像学诊断方面,大对数学者均认为彩色多普勒超声、CT对诊断肝淋巴管无明显特异性。肝囊性淋巴管患者临床影像学多提示肝单发或多发有分房的囊性占位[18],易误诊为肝囊肿、肝囊腺瘤、肝囊腺癌及Caroli病等肝内囊性病变[19-21]。笔者收治的2例患者均是术后病理才明确诊断。回顾文献中6例患者病例资料,术前仅有2例诊断正确(2/6),其余均被误诊。肝囊肿在彩色多普勒超声及CT上多提示肝脏实质内可见低密度圆形或类圆形病灶,边界清晰,内部密度较均匀,强化后壁不增强。肝脏囊腺瘤及肝脏囊腺癌常有分隔,而且囊内可见实质性呈不规则或“菜花样”的肿块 [21]。Caroli病表现为沿肝内胆管走行分布的大小不等的圆形或梭形的液性腔,其囊壁较厚回声增强。Choi等[20]MRI诊断1例肝囊性淋巴管患者时发现,淋巴管瘤在T1加权像呈低信号,增强后淋巴管瘤的微囊成分会增强,故T2加权分叶状囊性占位呈高信号,研究得出MRI有助于诊断肝囊性淋巴管瘤,诊断效果优于CT和彩色多普勒超声。
在治疗方面,因肝囊性淋巴管瘤与其他肝占位性病变较难鉴别。故主张对于不典型、不能排除恶性的,同时有明确体征或症状的患者应尽早手术,切除提倡完整切除病灶,有助于防止术后囊肿复发[10]。术中完善冷冻病理学检查,在明确病灶性质同时也可确定手术方式及切除范围。术后定期随访复查有助于复发早期诊断[22]。对于术前评估巨大的肝淋巴管瘤不能切除、严重的肝功能异常或不能耐受手术的患者可选择肝脏移植、无水酒精或注射硬化剂等治疗措施[23]。孙启鑫等[24]主张对于病理已明确,患者无不适、肝功能正常的患者, 且肝内病灶多发,可随访动态观察。
参考文献
[1] Stavropoulos M, Vagianos C, Scopa CD, et al. Solitary hepatic lymphangioma. A rare benign tumour: a case report[J]. HPB Surg,1994, 8(1):33–36.
[2] 岳继式. 肝囊状淋巴管瘤一例[J]. 癌症, 1986, 5(1):56.Yue JW. Cystic hepatic lymphangioma in one case[J]. Chinese Journal of Cancer, 1986, 5(1):56.
[3] 张海兰, 王练英. 小婴儿肝巨大多囊性淋巴管瘤一例[J]. 中华小儿外科杂志, 2002, 23(6):542. doi:10.3760/cma.j.issn.0253–3006.2002.06.043.Zhang HL, Wang LY. Giant polycystic hepatic lymphangioma in an infant [J]. Chinese Journal of Pediatric Surgery, 2002, 23(6):542.doi:10.3760/cma.j.issn.0253–3006.2002.06.043.
[4] 侯敏, 孙经建. 肝脏淋巴管瘤1例[J]. 中国医学影像技术, 2003,19(2):194.Hou M, Sun JJ. Cystic lymphangioma of the liver: a report of one case[J]. Chinese Journal of Medical Imaging Technology, 2003,19(2):194.
[5] 白志刚, 德力格尔图, 赖玉书, 等. 肝脏囊状淋巴管瘤一例[J].中华普通外科杂志, 2003, 18(2):86. doi:10.3760/j.issn:1007–631X.2003.02.026.Bai ZG, Deli GET, Lai YS, et al. Cystic liver lymphangioma: a report of one case[J]. Zhong Hua Pu Tong Wai Ke Za Zhi, 2003,18(2):86. doi:10.3760/j.issn:1007–631X.2003.02.026.
[6] 邹荣莉, 陈娟. 肝尾叶淋巴管瘤致下腔静脉肝后段狭窄及门静脉海绵样变性一例[C]//中国超声医学工程学会成立30周年暨第十二届全国超声医学学术大会论文汇编. 西安: 中国超声医学工程学会成立30周年暨第十二届全国超声医学学术大会委员会,2014:C227.Zou RL, Chen J. Stenosis of the retrohepatic segment of inferior vena cava and portal vein cavernous transformation caused by lymphangioma of the hepatic caudate lobe: a report of one case[C]//Proceedings of the 30th anniversary of Chinese Association of Ultrasound in Medicine and Engineering and the 12th Chinese meeting of ultrasonic medicine. Xian: Committee of the 30th anniversary of Chinese Association of Ultrasound in Medicine and Engineering and the 12th Chinese meeting of ultrasonic medicine,2014:C227.
[7] 林巧妹, 谭炜, 朱锦德. 肝淋巴管瘤1例[J]. 浙江实用医学, 2014,19(2):150–151.Lin QM, Tan W, Zhu JD. Cystic lymphangioma of the liver in one case[J]. Zhejiang Practical Medicine, 2014, 19(2):150–151.
[8] Huang L, Li J, Zhou F, et al. Giant cystic lymphangioma of the liver[J]. Hepatol Int, 2010, 4(4):784–787. doi: 10.1007/s12072–010–9220–4.
[9] Zhang YZ, Ye YS, Tian L, et al. Rare case of a solitary huge hepatic cystic lymphangioma[J]. World J Clin Cases, 2013, 1(4):152–154.doi: 10.12998/wjcc.v1.i4.152.
[10] Liu Q, Sui CJ, Li BS, et al. Solitary hepatic lymphangioma: a onecase report[J]. Springerplus, 2014, 3:314. doi: 10.1186/2193–1801–3–314.
[11] Chung JH, Suh YL, Park IA, et al. A pathologic study of abdominal lymphangiomas[J]. J Korean Med Sci, 1999, 14(3):257–262.
[12] Koh CC, Sheu JC. Hepatic lymphangioma--a case report[J]. Pediatr Surg Int, 2000, 16(7):515–516.
[13] 陈玉芳, 刘红, 程红岩, 等. 单发肝脏海绵状淋巴管瘤1例[J]. 中国介入影像与治疗学, 2017, 14(11):714. doi:10.13929/j.1672–8475.201707038.Chen YF, Liu H, Cheng HY, et al. Solitary hepatic lymphangioma:Case report[J]. Chinese Journal of Interventional Imaging and Therapy, 2017, 14(11):714. doi:10.13929/j.1672–8475.201707038.
[14] Van Steenbergen W, Joosten E, Marchal G, et al. Hepatic lymphangiomatosis. Report of a case and review of the literature[J].Gastroenterology, 1985, 88(6):1968–1972.
[15] Nakano T, Hara Y, Shirokawa M, et al. Hemorrhagic giant cystic lymphangioma of the liver in an adult female[J]. J Surg Case Rep,2015, 2015(4). pii: rjv033. doi: 10.1093/jscr/rjv033.
[16] Galambos C, Nodit L. Identi fi cation of lymphatic endothelium in pediatric vascular tumors and malformations[J]. Pediatr DevPathol,2005, 8(2):181–189.
[17] 秦颖, 倪勇, 王成友, 等. 肝脏罕少见实性占位病变的诊断和治疗(附38例病例报告)[J]. 安徽医学, 2009, 30(2):157–159.doi:10.3969/j.issn.1000–0399.2009.02.021.Qin Y, Ni Y, Wang CY, et al. Diagnosis and treatment of the rare tumor-like lesions of liver[J]. Anhui Medical Journal 2009,30(2):157–159. doi:10.3969/j.issn.1000–0399.2009.02.021.
[18] Chan SC, Huang SF, Lee WC, et al. Solitary hepatic lymphangioma-a case report[J]. Int J Clin Pract Suppl, 2005,(147):100–102.
[19] Vargas-Serrano B, Alegre-Bernal N, Cortina-Moreno B , et al.Abdominal cystic lymphangiomas: US and CT findings[J]. Eur J Radiol., 1995, 19(3):183–187.
[20] Choi WJ, Jeong WK, Kim Y, et al. MR imaging of hepatic lymphangioma[J]. Korean J Hepatol, 2012, 18(1):101–104. doi:10.3350/kjhep.2012.18.1.101.
[21] Soares KC, Arnaoutakis DJ, Kamel I, et al. Cystic neoplasms of the liver: biliary cystadenoma and cystadenocarcinoma[J].J Am Coll Surg, 2014, 218(1):119–128. doi: 10.1016/j.jamcollsurg.2013.08.014.
[22] Lee HH, Lee SY. Case report of solitary giant hepatic lymphangioma[J]. Korean J Hepatobiliary Pancreat Surg, 2016,20(2):71–74. doi: 10.14701/kjhbps.2016.20.2.71.
[23] Tepetes K, Selby R, Webb M, et al. Orthotopic liver transplantation for benign hepatic neoplasms[J]. Arch Surg, 1995, 130(2):153–156.
[24] 孙启鑫, 张颖, 曾军, 等. 肝淋巴管瘤病合并血性乳糜胸1例[J]. 广东医学, 2009, 30(3):496. doi:10.3969/j.issn.1001–9448.2009.03.081.Sun QX, Zhang Y, Zeng J, et al. Cystic hepatic lymphangiomat with a bloody chylothorax in one case[J]. Guangdong Medical Journal,2009, 30(3):496. doi:10.3969/j.issn.1001–9448.2009.03.081.