胆道结石病是普通外科常见的疾病,常规超声检查因简便易行、无创伤成为评价胆道梗阻的影像学检查方法。胆道术后的患者更由于胆总管手术局部粘连,胆囊切除等原因导致其在常规超声下显影较差,导致胆总管术后残石在检测中可能存在漏诊。超声造影剂六氟化硫(商品名声诺维,SonoVue)微泡的大小和变形性与红细胞相似,无生物活性,不影响微循环血流,且不会扩散到组织间隙,具有用量小、无需行过敏实验、无肾毒性等优点[1-2]。声诺维在经外周静脉注射的血管显像方面的应用具有优势,然而在非血管腔道显影方面的表现报道较少。本研究通过胆道T管或经皮经肝胆道穿刺引流(PTCD)窦道扩张管将超声造影剂稀释液及生理盐水直接注入胆道,以达到超声显像下的直接胆管显影并发现胆总管术后残石,探讨经胆道超声造影联合生理盐水注入的临床应用价值。
1 资料与方法
1.1 一般资料
选取2016年8月―2017年12月于我科行开腹或腹腔镜下胆总管切开探查取石,胆总管留置T管引流3个月后返回我科行经T管窦道胆道镜探查的患者41例,以及行PTCD术后并进行窦道扩张取石患者10例。其中男24例,女27例;平均年龄(64.4±11.0)岁;单纯胆总管残石17例,单纯肝内胆管结石10例,胆总管残石合并肝内胆管结石6例,肝内外胆管均无结石18例。
1.2 研究方法
1.2.1 胆管腔内超声造影 采用东芝Aplio500型号彩色多普勒成像仪,具有超声造影功能的凸阵探头,频率3~5 MHz。超声造影剂为声诺维(Bracco公司),每瓶加入5 mL生理盐水,充分振荡混匀后备用,使用时抽取按1:100比例以生理盐水稀释后抽取10 mL经T管或PTCD管胆道超声造影显像。先后进行常规超声检查造影模式,经胆道引流管注入声诺维稀释剂10 mL,观察造影剂在胆道内显影情况,明确找到胆总管位置,以造影图像中胆总管为指引并定位,继续注入生理盐水20 mL继续观察胆总管内部情况。图像评价内容:胆总管根据胆总管图像显示的状况,测量并记录造影前后胆总管显示长度及宽度,单位以cm计,观察胆总管内是否存在残留结石,尤其在胆总管下段至乳头处重点观察,记录结石形态、大小及数量。
1.2.2 胆道X线造影检查 由我院胃肠造影室完成,造影剂为碘普罗胺,与生理盐水1:1混合后经T管或PTCD窦道扩张管注入,经多个体位及方向观察胆总管形态,是否存在充盈缺损等情况。患者检查结束后均开放胆道T管或PTCD引流管持续引流,并密切观察24 h是否有发热、腹痛、腹泻等不良反应发生。
1.2.3 胆道镜检查 由我院胆道外科具有多年胆道镜操作及镜下取石经验的副主任级别以上医师于手术室经局麻下进行,经T管或PTCD窦道放入纤维胆道镜,探查胆总管及肝内各级胆管。若发现有残余结石,则使用碎石机及取石网篮取石。取石后再次探查胆总管及肝内各级胆管,若明确无残留结石则撤出胆道镜并封闭窦道口。若胆道残余结石较大或较多难以一次性取尽或患者术中难以耐受继续取石,考虑仍有残余结石者,留置适当粗细T管并固定后结束手术。
1.3 统计学处理
采用SPSS 17.0统计软件,超声造影前后胆总管直径与长度计量资料以均数±标准差( ±s)表示,直径与长度变化采用配对t检验。超声造影、X线胆道造影下是否发现残石结果与胆道镜结果间比较采用配对χ2检验并进行一致性κ检验。
±s)表示,直径与长度变化采用配对t检验。超声造影、X线胆道造影下是否发现残石结果与胆道镜结果间比较采用配对χ2检验并进行一致性κ检验。
2 结 果
2.1 胆道超声造影下胆总管显影情况
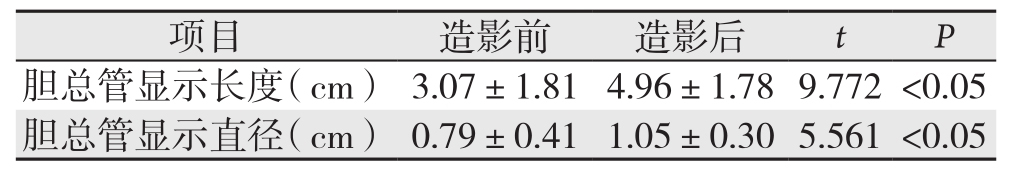
所有患者均在住院期间完成经T管胆道腔内超声造影检查以及经T管窦道胆道镜检查。首先经常规超声检查肝胆脾胰等脏器并记录相关数据(图1A),经T管或PTCD窦道扩张管注入配制好的声诺维约10 mL并观察胆总管显影状态(图1B),注入生理盐水20 mL,着重观察由声诺维注入后显影的胆总管走形区域,生理盐水进入后为阴性对照,可寻找胆总管中强回声影(图1C-D),记录相应数据。所有患者中47例患者(92.2%)在超声造影联合生理盐水胆道注入下可观察到胆总管全长。胆总管显示长度、直径数据如表1所示,超声造影下可明显提高胆总管显影效果。行胆道超声造影联合生理盐水注入检查后观察患者24 h,无发热寒战,腹泻等不良反应发生。
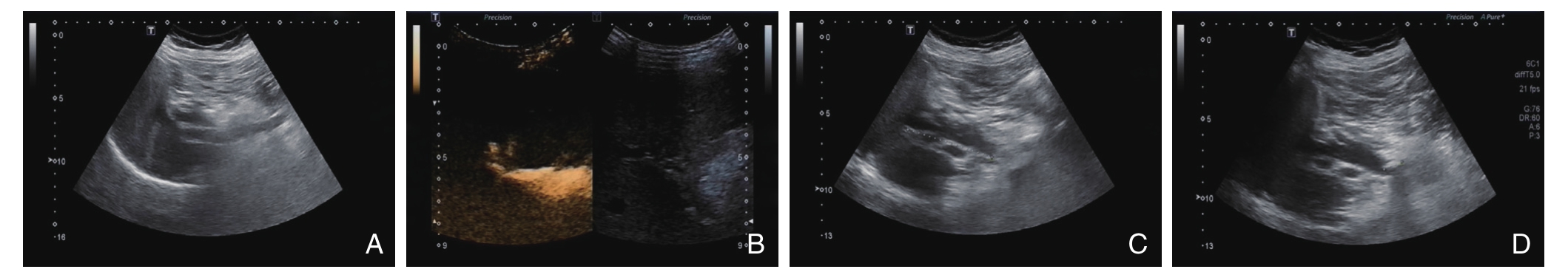
图1 胆道超声造影 A:常规超声检查肝胆脾胰等脏器并记录相关数据;B:经T管或PTCD窦道扩张管注入配制好的声诺维约10 mL并观察胆总管显影状态;C-D:着重观察由声诺维注入后显影的胆总管走形区域,生理盐水进入后为阴性对照,可寻找胆总管中强回声影
Figure 1 Intrabiliary CEUS A: Routine ultrasound examination for the visceral organs such as liver, gallbladder, spleen and pancreas;B: Observation of the common bile duct after 10 mL prepared SonoVue injection through T-tube sinus tract or dilated PTCD sinus tract; C–D: Observing the region of the common bile duct running after SonoVue injection, and then looking for the hyperechoic area after the negative contrast media saline injection
表1 超声造影前后胆总管显示长度、直径( ±s)
±s)
Table 1 The length and diameter of the common bile duct before and after CEUS ( ±s)
±s)
05 05
2.2 超声造影观察胆总管残石
本研究中,胆道超声造影下观察胆总管后注入生理盐水检查胆总管残石的敏感度为78.3%,特异度为96.4%,与金标准配对χ2检验及一致性检验结果显示,差异无统计学意义(P>0.05),与金标准一致性较高(κ=0.76)。诊断符合率为88.2%(45/51),5例胆总管残石患者在超声造影检查中未能发现残石,其中4例患者超声造影联合盐水注入检查下未能全程观察胆总管,且所见区域未发现残石,而胆道镜下观察则发现有残石存在并予以取出,另有1例患者胆道镜下观察为少量泥沙样结石,超声造影后注入生理盐水未能发现;1例患者经超声造影后观察到胆总管全程,注入生理盐水后发现残留强回声团,考虑残石,而胆道镜下观察未发现结石。所有患者在行超声造影检查后返回病房继续观察,24 h内无患者出现发热、腹泻等不良反应。
2.3 胆道X线造影及胆道镜探查结果
X线胆道造影检查在本研究中对胆总管残石诊断敏感度为60.9%,但特异性为100%,一致性检验κ值为0.63,诊断符合率为82.4%(42/51)。超声造影下未发现残石的患者通过X线造影下发现残石存在并通过胆道镜确认。8例患者(15.7%)经胆道X线造影检查后夜间出现轻度发热及腹泻症状,经物理降温及保守治疗后均于12 h内好转。16例肝内胆管结石患者中予以胆道镜下碎石机碎石后网篮取石,9例患者因肝内结石较多,未能一次取尽,遂再次留置窦道支撑管以引流胆汁。所有患者经胆道镜探查术后返回病房密切观察病情变化,无患者出现发热、寒战及腹痛等胆管炎症状。
3 讨 论
经静脉超声造影目前应用已较广泛,例如肝内占位、胆道梗阻原因鉴别等方面均有较研究[1-2]。X线胆道造影也是胆道术后常用检查手段之一,可观察胆道形态,并通过是否有充盈缺损等来判断是否存在残石。但此检查存在一定的辐射,且造影剂多为含碘造影剂,部分患者使用后存在发热、寒战、过敏等不良反应。在以往研究中也有利用T管注入生理盐水行超声显像,对胆道残石的检出率稍有提高[3],但相关研究较少。曾庆劲等[4]尝试经T管向胆道内注射声诺维及生理盐水来观察残石的存在,与常规超声检查相比显著提高了胆总管及其内结石显影率。本研究采用先经T管向胆道内注入造影剂声诺维,在造影模式中可显示肝内外胆道整体形态,在此基础上注入生理盐水并持续观察胆总管内部状况,通过生理盐水的阴性对比消除声诺维强回声对结石判断的影响,且所有结果均与胆道镜下结果作为金标准相比较来评判其临床意义。在本研究中,注入声诺维前后的胆总管显影效果有明显的统计学差异,所有患者中92.2%可完整地观察到胆总管形态,且可以在此基础上发现胆总管残石并区分出其大小、是否泥沙样结石等。5例患者因胆道积气及胆道术后局部粘连等原因致使胆总管未能完全观察清,但结合X线胆道造影仍可对其胆总管残石是否存在做出更好的判断。虽然目前胆道超声造影下联合生理盐水注入检查结果与胆道镜下观察结果并没有完全一致,但两项检查联合可以较好的提高诊断的准确率,故结合相关术前检查可对胆总管残石的判断更有把握。
相关文献[5-6]报道,一般在开腹胆道手术后2周时间以后,T管周围窦道形成较为牢固,可拔出T管,行经T管窦道胆道镜探查取石术。而在腹腔镜手术后则窦道形成时间一般较长。文献曾报道即使是术后4~6个月时间后拔出T管时仍有患者出现T管窦道胆汁漏的情况。因此,在T管窦道形成较为牢固以前贸然拔出T管是很危险的[6]。因此,目前普遍认为在胆总管切开探查留置T管引流术后4~6周时间后拔出T管行胆道镜探查较为安全[7]。而经T管胆道腔内超声造影检查时间可相对提前,在实践中在PTCD术中或术后任何时间,T管引流术术后2周左右就可以进行,可以在胆道术后较早进行相关检查,明确胆道是否残石存留。在一些未开展胆道镜探查取石术的医院,处理胆道术后患者的时候,通过胆道超声造影下生理盐水注入并结合胆道X线造影提高胆道术后残石,可以在术后较早期对是否存在残石做出较好判断,可以作为在没有胆道镜设备下拔管前的重要检查手段。
超声造影图像对比度和信噪比的同时并不产生超声伪像,具有可以实时动态观察、清晰、可重复性好、辐射剂量少、代谢快、毒副作用少、无辐射等优势[8]。在胆道其他疾病中例如行经皮经肝胆囊穿刺引流术(PTGBD)或PTCD时,当穿刺目标胆管管径过细,穿刺路径图像不甚清晰,或患者不能配合手术、置管后不能确定是否达到目标位置时,借助影像学检查加以明确尤为重要[9-13]。胆道超声造影则可以及时进行,观察造影剂喷射出引流管的位置可以判断引流管末端位置,显示引流管全程,且根据需要实时对引流管位置进行调整,直至到达理想位置,达到引流通畅,且相对无辐射风险[14]。在胆道梗阻性疾病对胆道梗阻部位和病因诊断中,相关研究也证实胆道腔内超声造影的应用价值[14-16],如肝门胆管癌,胆肠吻合口狭窄等。经T管胆道腔内超声造影检查也可用来动态观察肝移植术后胆道吻合口状况及胆道形态[17]。
经T管或PTCD扩张管行胆道腔内超声造影联合生理盐水注入,对胆道术后残石的诊断有一定的临床意义。在实际操作中,向胆道腔内注入造影剂及生理盐水过程需时刻注意患者有无腹痛、腹胀等状况,检查结束后也应继续观察患者是否发热等不良反应[18]。研究中仍有几例患者胆总管显示不清,无法判断是否存在残石,主要考虑与以下几点有关:年龄较大,胃肠道气体干扰严重;胆道手术导致胆道系统处于开放状态且生理结构改变,导致超声检查图像质量显示欠佳。在临床实践中继续探索以找出更好的办法来帮助提高超声下胆总管显影率并提高对胆道残石的诊断水平。另一方面,此检查方法也可被应用于其他类型胆道引流管中,例如经鼻胆管引流管[8](ENBD管)或PTGBD管以及其他方面,提高相应疾病的诊断准确率[19]。
参考文献
[1] Fontán FJ, Reboredo ÁR, Siso AR. Accuracy of Contrast-Enhanced Ultrasound in the Diagnosis of Bile Duct Obstruction[J]. Ultrasound Int Open, 2015, 1(1):E12–18. doi: 10.1055/s–0035–1555880.
[2] Spârchez Z, Radu P. Role of contrast enhanced ultrasound in the assessment of biliary duct disease[J]. Med Ultrason, 2014,16(1):41–47.
[3] 张金平, 于晓燕, 郭春兰, 等. 胆道术后T管注水B型超声检查法(附80例分析)[J]. 上海医学影像, 1992, 1(1):19–21.Zhang JP, Yu XY, Guo CL, et al. B-type ultrasound examination via T-tube water injection after biliary surgery: a report of 80 cases[J].Shanghai Medical Imaging, 1992, 1(1):19–21.
[4] 曾庆劲, 许尔蛟, 郑荣琴, 等. 胆总管残留结石经T管胆道腔内超声造影表现及其诊断价值[J]. 中华医学超声杂志:电子版, 2011,8(12):2541–2549. doi:10.3877/cma.j.issn.1672–6448.2011.12.017.Zeng QJ, Xu EJ, Zheng RQ, et al. The feature and diagnostic value of T-tube intracavitary contrast enhanced ultrasound cholangiography in residual common bile duct stones[J]. Chinese Journal of Medical Ultrasound: Electronic Edition, 2011,8(12):2541–2549. doi:10.3877/cma.j.issn.1672–6448.2011.12.017.
[5] Soltani E, Mehrabi Bahar A, Dehghanian P, et al. Prevention of Biliary Leakage after Removal of T-tube in Immunocompromised Patients[J]. Indian J Surg, 2015, 77(Suppl 2):645–649. doi: 10.1007/s12262–013–0958–5.
[6] 丁轶人, 江涌, 赵伟, 等. 胆道T管引流术后T管拔除时间的临床研究[J]. 吉林医学, 2017, 38(1):54–58. doi:10.3969/j.issn.1004–0412.2017.01.020.Ding YR, Jiang Y, Zhao W, et al. The clinical study on the time of removal of T tube after T tube drainage of biliary tract[J]. Jilin Medical Journal, 2017, 38(1):54–58. doi:10.3969/j.issn.1004–0412. 2017.01.020.
[7] 赵亚. 胆总管T管拔除时间探讨[J]. 中国现代普通外科进展,2010, 13(10):834–835. doi:10.3969/j.issn.1009–9905.2010.10.027.Zhao Y. Timing for choledochal T-tube removal[J]. Chinese Journal of Current Advances in General Surgery 2010, 13(10):834–835.doi:10.3969/j.issn.1009–9905.2010.10.027.
[8] 王阳, 唐少珊. 超声造影引导下生理盐水胆道注入在超声检测胆总管残石中的价值[J]. 中华超声影像学杂志, 2017, 26(6):517–521. doi:10.3760/cma.j.issn.1004–4477.2017.06.011.Wang Y, Tang SS. The value of contrast-enhanced ultrasound guiding normal saline injection in the detection of residual common bile duct stones[J]. Chinese Journal of Ultrasonography, 2017,26(6):517–521. doi:10.3760/cma.j.issn.1004–4477.2017.06.011.
[9] 许尔蛟, 郑荣琴, 李凯, 等. 胆管内超声造影在经皮经肝胆道引流术中的应用价值[J]. 中华医学超声杂志:电子版, 2011, 8(9):1937–1945. doi:10.3877/cma.j.issn.1672–6448.2011.09.010.Xu EJ, Zheng RQ, Li K, et al. Application value of intrabiliary contrast-enhanced ultrasonography in percutaneous transhepatic cholangial drainage[J]. Chinese Journal of Medical Ultrasound:Electronic Edition, 2011, 8(9):1937–1945. doi:10.3877/cma.j.issn.1672–6448.2011.09.010.
[10] 崔玉军. 胆道超声造影的临床实践进展[J]. 继续医学教育, 2010,24(5):53–55. doi:10.3969/j.issn.1004–6763.2010.05.018.Cui YJ. The Progress on Clinical Practice of Ultrasound Cholangiography[J]. Continuing Medical Education, 2010,24(5):53–55. doi:10.3969/j.issn.1004–6763.2010.05.018.
[11] 孔艳鹏, 冯蕾, 夏要友, 等. 对比增强超声在非血管性腔道的应用[J]. 中国医学影像学杂志, 2014, 22(9):704–707. doi:10.3969/j.issn.1005–5185.2014.09.21.Kong YP, Feng L, Xia YY, et al. Application of Contrast-enhanced Ultrasound in Detection Non-vascular Channel[J]. Chinese Journal of Medical Imaging, 2014, 22(9):704–707. doi:10.3969/j.issn.1005–5185.2014.09.21.
[12] Xu EJ, Zheng RQ, Su ZZ, et al. Intra-biliary contrast-enhanced ultrasound for evaluating biliary obstruction during percutaneous transhepatic biliary drainage: a preliminary study[J]. Eur J Radiol,2012, 81(12):3846–3850. doi: 10.1016/j.ejrad.2012.06.025.
[13] 吕新华. 胆道超声造影在经皮经肝胆道穿刺引流术后引流不畅患者中的应用价值[J]. 中国超声医学杂志, 2015, 31(9):801–803.Lu XH. Application Value of Contrast-enhanced Ultrasonic Cholangiography in Percutaneous Transhepatic Cholangial Drainage[J].Chinese Journal of Ultrasound in Medicine, 2015, 31(9):801–803.
[14] Luyao Z, Xiaoyan X, Huixiong X, et al. Percutaneous ultrasoundguided cholangiography using microbubbles to evaluate the dilated biliary tract: initial experience [J]. Eur Radiol, 2012, 22(2):371–378.doi: 10.1007/s00330–011–2265–5.
[15] 许尔蛟, 李凯, 郑荣琴, 等. 三维经胆道超声造影对肝门部胆管癌的诊断价值的初步研究[J]. 中山大学学报:医学科学版, 2015,36(1):150–153.Xu EJ, Li K, Zheng RQ, et al. Preliminary Study of Value of Three-dimensional Intra-biliary Contrast Enhanced Ultrasound in Diagnosis of Hilar Cholangiocarcinoma[J]. Journal of Sun Yat-sen University: Medical Sciences, 2015, 36(1):150–153.
[16] 李颖如, 樊静, 蒋晓春, 等. 超声胆道造影技术的初步应用[J]. 新医学, 2013, 44(6):382–384. doi:10.3969/g.issn.0253–9802.2013. 06.007.Li YR, Fan J, Jiang XC, et al. Application of contrast-enhanced ultrasonography in biliary tract[J]. New Medicine, 2013, 44(6):382–384. doi:10.3969/g.issn.0253–9802.2013.06.007.
[17] Chopra SS, Eisele R, Stelter L, et al. Contrast enhanced ultrasound cholangiography via T-tube following liver transplantation [J]. Ann Transplant, 2012, 17(4):108–112.
[18] Geleijnse ML, Nemes A, Vletter WB, et al. Adverse reactions after the use of sulphur hexafluoride (SonoVue) echo contrastagent[J]. J Cardiovasc Med (Hagerstown), 2009, 10(1): 75–77. doi: 10.2459/JCM.0b013e328319bfba.
[19] 郑荣琴, 许尔蛟. 超声造影在胆道系统的应用新进展[J]. 中华医学超声杂志:电子版, 2012, 9(3):191–194. doi:10.3877/cma.j.issn.1672–6448.2012.03.001.Zheng RQ, Xu EJ. New progress of contrast-enhanced ultrasonography for biliary system[J]. Chinese Journal of Medical Ultrasound: Electronic Edition, 2012, 9(3):191–194. doi:10.3877/cma.j.issn.1672–6448.2012.03.001.