由肝癌导致的全球病死率每年都在不断增加,尽管经肝动脉化疗栓塞、射频消融、分子靶向治疗、免疫治疗等多元化的治疗手段为肝癌患者带来的更多生存的机会,但手术切除仍是治疗肝癌最有效的方法[1]。术前肝功能以及残余肝体积(FLR)是肝切除术前评估的重要指标,如术前肝功能正常,无肝炎、肝硬化等基础疾病的患者,FLR/全肝体积(TLV)>25%即可耐受较大范围的肝切除术;对于术前存在慢性肝病而未合并肝硬化的患者,FLR/TLV要求达到30%以上;术前已发生肝硬化而尚未出现门脉高压的患者,FLR/TLV要求达到40%以上[2]。门静脉栓塞术(PVE)、门静脉结扎术(PVL)都曾被作为刺激FLR增长的有效方法,但4~8周的二期手术等待时间使一部分患者因为肿瘤的进展而最终失去了根治性手术的机会[3]。因此,如何在短期内快速刺激FLR的增长以提高手术切除率是肝脏外科医生亟待解决的问题。
1 关于肝脏离段联合门静脉结扎二期肝切除术(ALPPS)的诞生及现状
2007年由Schlit首次提出了ALPPS:其原本打算为1例高位肝门部胆管癌的患者施行扩大右半肝切除术,因术中发现患者的FLR过小,故为该患者施行姑息性胆管-空肠吻合术,为了充分暴露手术野并完成高位胆肠吻合,Schlit沿镰状韧带右侧缘将肝实质原位离段,并结扎门静脉右支以减少肿瘤血供。患者于术后第8天复查CT意外发现左肝体积明显增大,于是Schlit再次为患者施行扩大右半肝切除术,术后患者未发生肝功能衰竭并快速康复[4]。
ALPPS自2007年首次实施至2012年正式提出之后[5],国际许多大型肝脏外科中心已先后实施数百例,通过一期手术结扎门静脉右支和施行肝实质离段,ALPPS能在短期内快速刺激FLR增长65%~95%[6],其相比于PVE及PVL造成的1/3的患者因FLR增长不足而失去二期手术机会[7],ALPPS显著提高了肝癌患者的手术切除率,为FLR不足患者带来了新的手术机会和根治可能;但其极高的并发症发生率及病死率至今仍是该术式未能广泛实施的首要瓶颈(表1)。
表1 有关ALPPS的文献回顾
Table1 Review of the literature concerning ALPPS
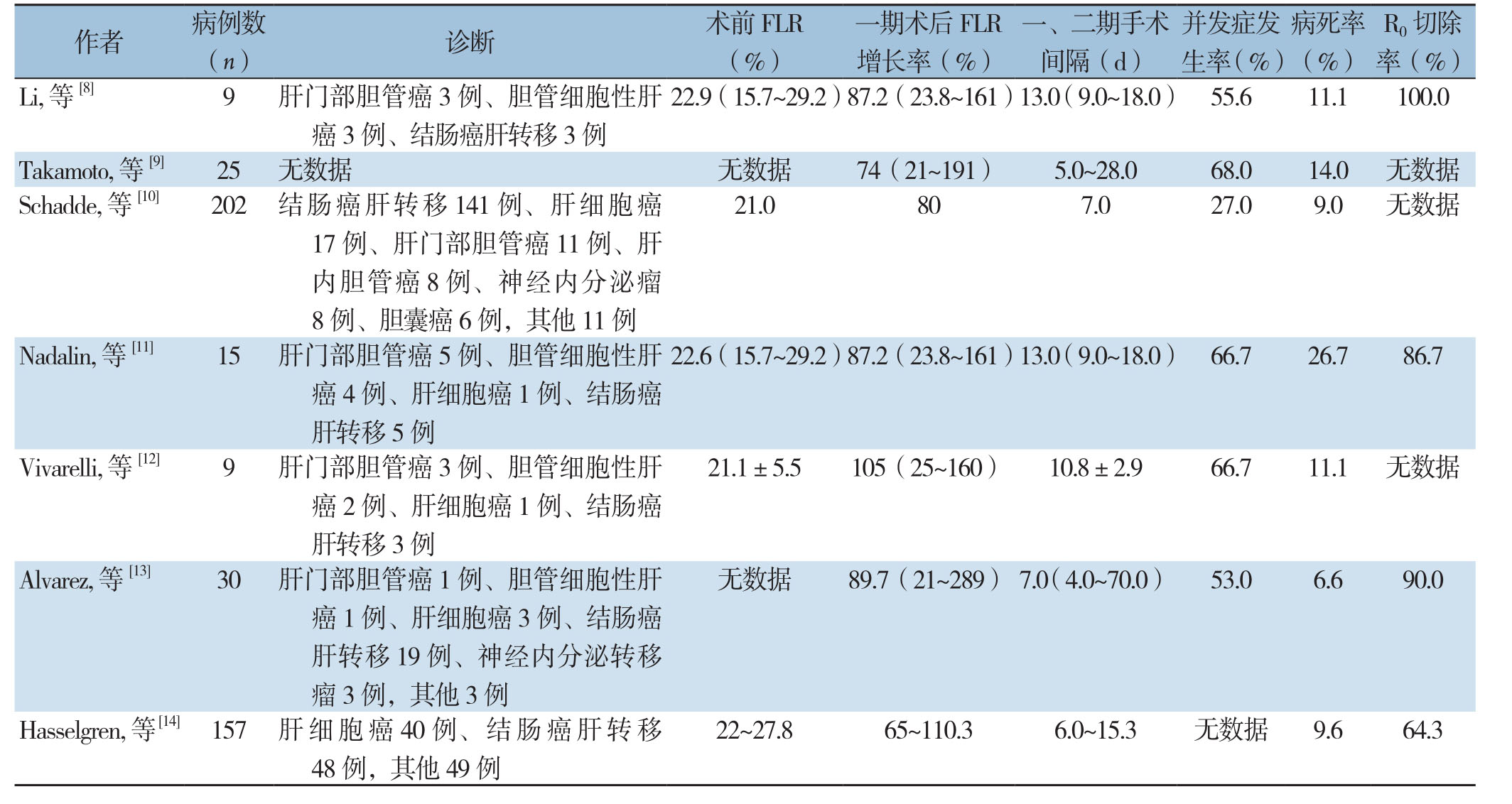
作者 病例数(n) 诊断 术前FLR(%)一期术后FLR增长率(%)一、二期手术间隔(d)并发症发生率(%)病死率(%)22.9(15.7~29.2)87.2(23.8~161)13.0(9.0~18.0) 55.611.1100.0 Takamoto, 等[9] 25 无数据 无数据 74(21~191) 5.0~28.068.014.0 无数据Schadde, 等[10] 202 结肠癌肝转移141例、肝细胞癌R0切除率(%)Li, 等[8] 9 肝门部胆管癌3例、胆管细胞性肝癌3例、结肠癌肝转移3例21.0807.027.09.0 无数据17例、肝门部胆管癌11例、肝内胆管癌8例、神经内分泌瘤8例、胆囊癌6例,其他11例Nadalin, 等[11] 15 肝门部胆管癌5例、胆管细胞性肝癌4例、肝细胞癌1例、结肠癌肝转移5例22.6(15.7~29.2)87.2(23.8~161)13.0(9.0~18.0) 66.726.786.7 Vivarelli, 等[12] 9 肝门部胆管癌3例、胆管细胞性肝癌2例、肝细胞癌1例、结肠癌肝转移3例21.1±5.5105(25~160) 10.8±2.966.711.1 无数据Alvarez, 等[13] 30 肝门部胆管癌1例、胆管细胞性肝癌1例、肝细胞癌3例、结肠癌肝转移19例、神经内分泌转移瘤3例,其他3例无数据 89.7(21~289) 7.0(4.0~70.0) 53.06.690.0 Hasselgren, 等[14] 157 肝细胞癌40例、结肠癌肝转移48例,其他49例22~27.865~110.36.0~15.3 无数据 9.664.3
2 关于ALPPS的基础研究
2.1 ALPPS动物模型的建立
动物模型的建立一直是ALPPS基础研究的重点,大鼠在研究门静脉血流动力学变化、肝组织灌注方面较小鼠有明显优势,其次大鼠模型不需要切除左肝外侧叶[15]。通过分离并结扎大鼠右后叶、左外叶、左中叶和尾状叶门静脉分支,并在右中叶及左中叶肝裂间进行肝实质离段,术后3 d,右中叶可见明显增长[16]。
2.2 ALPPS短期内使肝体积快速增长的机制[17]
2.2.1 血流动力学因素 通过结扎门静脉右支,使残余肝血流显著增加是刺激肝体积增生的基础[7, 18],同时施行原位肝实质离段,避免了病肝侧支循环的建立,是ALPPS的FLR增生明显优于PVE及PVL的主要原因[18]。
2.2.2 体液学因素 Schlegel等[19]的实验结果表明无论是ALPPS或PVL,术后均能产生刺激肝细胞增殖的相关血清学因子。Shi等[20]通过对一、二期术后肝组织免疫组化结果进行对比证明ALPPS术后的小鼠其Ki-67及增殖细胞核抗原高于PVL组4倍,高于肝实质离段组10倍;ALPPS组残余肝的TNF-α,IL-6和HGF的表达高于对照组3倍;更有意义的是STAT3、Yap、NF-κB p65在ALPPS组中显著表达。Dhar等[21]的动物实验不仅同样证明了Ki-67和IL-6在ALPPS术后明显升高,同时还检测到粒细胞-巨噬细胞集落刺激因子、血管内皮生长因子、γ-干扰素较PVL组明显升高。黄民等[22]通过建立ALPPS组及PVL组大鼠模型,发现在严重创伤刺激下导致的各种促炎及生长调节因子大量释放,使得ALPPS组肝内干/祖细胞活化程度明显强于PVL组。
3 ALPPS的争议
ALPPS最大的争议在于其较高的并发症发生率及病死率。统计结果显示,ALPPS术后胆汁漏、腹腔感染、脓毒血症、感染性休克等并发症的发生率高达16%~64%,术后随访180 d病死率高达12%~23%[8- 9, 23-25],其中原发性肝癌和胆管癌患者的并发症发生率远高于结肠癌肝转移患者[10, 26],其高病死率在因胆囊癌或胆管癌需要进行胆道重建的患者中尤为明显[8, 11, 26];因此术前积极完善血管CT、胰胆管水成像等相关检查,术中结扎门静脉右支同时保证病肝动脉供血和静脉回流,避免对肝十二指肠韧带的过度解剖[24, 27],能有效降低术后病死率。其次,Joechle等[28]实验得出,ALPPS一期术后FLR快速增长的同时,肿瘤也进一步进展,Fukami等[29]和Kukodo等[3]的实验结果显示肿瘤活检的Ki-67在一期手术后增长近20%,这可能与结扎病肝门静脉后,肿瘤通过其供血肝动脉代偿有关[30-31]。
有关术中处理的争议主要集中于是否在肝实质离段面通过生物活性塑料袋包裹病肝以减轻腹腔粘连和是否在一期手术中结扎右肝管。曾有学者[32]提出在肝实质离段面以生物活性塑料袋包裹病肝不仅可以预防腹腔粘连,还能局限肝断面渗漏的胆汁,减轻腹腔感染。但随着ALPPS实施例数的不断增加,也有学者[8]认为由于一期手术与二期手术间隔时间短,并不易在腹腔形成致密粘连,而且生物活性塑料袋本身属于异物,在部分患者因FLR增长不足无法施行根治性肝切除术的情况下,仍需接受二次手术取出留置于腹腔内的生物活性塑料袋,增加了患者的手术创伤及感染风险[8]。一组来自Alvarez等[24]的数据显示,其在肝断面放置生物活性塑料袋的病例中,术后病死率高达58%。所以目前大多数学者不建议一期手术中在肝断面留置生物活性塑料袋预防腹腔粘连[26, 33-34]。
经典ALPPS术式在结扎门静脉右支的同时结扎右肝管以刺激肝体积增长,但随着越来越多的中心报道传统ALPPS的高病死率,使专家们对术中结扎右肝管持以更加谨慎保守的态度。因术后患者的高病死率与胆汁漏及感染密切相关,不少学者认为结扎右肝管将使其胆道压力升高,增加胆汁漏及其继发的感染等风险,故明确建议避免一期手术中结扎右肝管[35-36]。
其次,有关ALPPS一、二期手术时间间隔目前尚未达成统一共识,基础研究[37]表明,成肝细胞大约需要8~10 d才能变为成熟肝细胞,ALPPS一期术后早期所刺激产生的肝细胞多为不成熟肝细胞,FLR的增长并不能反映其肝功能的恢复,因此一期手术后不仅要评估FLR增长率,还应通过血清肝功能测定、ICG排泄实验等评估肝功能的恢复以确定二期手术时机[38],Truant等[39]也提出,放射性核素肝胆显像(HBS)对于ALPPS一期术后肝功能的评估亦有明显优势。
肝癌合并肝硬化是否应纳入ALPPS手术适应证存在颇多争议,虽然目前国内外都有肝癌合并肝硬化患者成功实施ALPPS的病例报道[40],但也有报道[41]指出术前合并肝硬化患者的一期术后FLR增长率的往往低于术前肝功能正常的患者,且由于肝功能的恢复往往滞后于肝体积的增长,所以术前合并肝硬化的患者术后发生肝衰竭的概率将明显高于术前肝功能正常的患者;Vivarelli等[12]病例统计中ALPPS术后病死率为11.1.%,其中死亡患者均为术前合并肝纤维化的患者;Uribe等[42]的研究中,肝硬化患者的一、二期手术间隔平均为10 d,相较于无肝脏基础疾病患者7~8 d的二期手术等待期有延长,其次50%的肝硬化患者最终死于术后肝功能衰竭或其他并发症。
4 ALPPS的病例选择
关于ALPPS的手术适应证目前尚未达成统一共识,但大多数学者[34, 43-44]认为:术前未接受化疗、年龄<60岁、结肠癌肝转移患者的手术预后明显优于其他患者。我国作为易感乙型肝炎病毒的典型地区,2015—2016年全国慢性乙肝报告发病率(/10万)为27.01(2005年)~60.08(2016年)[45],彭驰涵等[46]认为,对于合并乙肝背景的原发性巨大肝癌患者,FLR<40%或FLR /体质量(GRWR)<0.8%,可纳入ALPPS手术适应证,其次,肿瘤应局限于左三肝或右三肝内,门静脉主干或主要分支内无癌栓;而肝功能Child-Pugh C 级、肿瘤范围超过左三肝或右三肝范围、门静脉主干及主要门静脉分支、肝静脉内有癌栓应为ALPPS的手术禁忌证。
5 ALPPS术式的改进
为了降低A L P P S的并发症发生率及病死率,外科医生们对ALPPS术式不断进行研究与改进,衍生出多种术式,主要有腹腔镜ALPPS(Lap-ALPPS),部分ALPPS(p-ALPPS),经肝后隧道绕肝带结扎和门静脉结扎二期肝切除术(ALTPS),射频消融ALPPS(RALPPS),杂交ALPPS(H-ALPPS),末梢门静脉栓塞计划性肝切除术(TELPP)等,有关各术式的手术情况及疗效对比见表2。
表2 有关ALPPS衍生术式的病例数据对比
Table2 Comparison of the data of cases undergoing ALPPS derived procedures
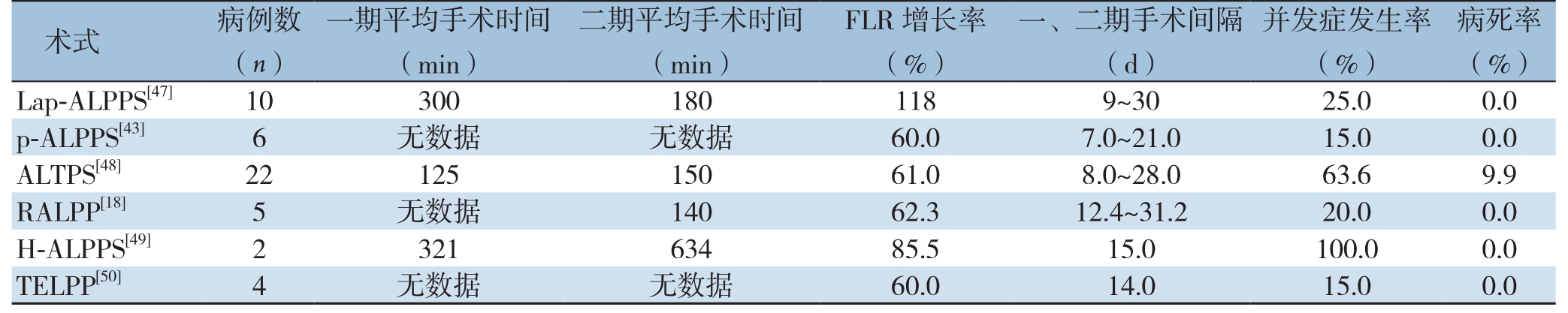
病死率(%)Lap-ALPPS[47] 103001801189~3025.00.0 p-ALPPS[43] 6 无数据 无数据 60.07.0~21.015.00.0 ALTPS[48] 2212515061.08.0~28.063.69.9 RALPP[18] 5 无数据 14062.312.4~31.220.00.0 H-ALPPS[49] 232163485.515.0100.00.0 TELPP[50] 4 无数据 无数据 60.014.015.00.0术式 病例数(n)一期平均手术时间(min)二期平均手术时间(min)FLR增长率(%)一、二期手术间隔(d)并发症发生率(%)
5.1 Lap-ALPPS
自1991年第1例腹腔镜下肝切除术实施至今[51],腹腔镜肝切除术已由最初的技术探索和辅助器械发明发展到如今对其疗效价值的评价[52]。Lap-ALPPS的技术要点与经典ALPPS相同,但Lap-ALPPS可以明显减少腹腔粘连和全身炎症反应[53],大大降低了二期手术难度及并发症风险。 在腹腔镜技术成熟的肝脏外科中心,Lap-ALPPS的术后病死率和缩短住院都明显减少[47],且腹腔镜手术与传统开腹手术在肿瘤切除率方面无明显差异[54],Lap-ALPPS在提高患者围手术期疗效和肿瘤远期疗效上又具有明显优势。
5.2 p-ALPPS
p-ALPPS即从最初的原位肝实质全部离段更改为部分肝实质离段。Petrowsky等[43]、Tanaka等[55]的病例对照及研究中得出结论:一期手术中离段50%~80%肝实质能有效减少一期手术后胆汁漏及脓毒血症发生率,且其中位二期手术等待时间及FLR增长率与施行完全肝实质离段无统计学差异。来自Alvarez等[24]的统计结果显示,在其针对ALPPS高病死率相关的危险因素分析中,在年龄、性别、体质量指数(BMI)、术前化疗、FLR/TLV、是否需肝外胆道处理及是否完全离段肝实质等因素中,只有“是否完全离段肝实质”作为独立危险因素具有统计学意义。目前,该术式已被许多中心采纳认可。
5.3 ALTPS
经肝后隧道绕肝带结扎肝实质,避免了肝实质离段,不仅能显著缩短一期手术时间、减少术中出血,减轻一期手术引起的腹腔粘连,还能避免因胆汁漏引起的腹腔感染、脓毒血症等并发症[48, 56]。Li等[32]的统计结果显示:ALTPS一期术后7 d FLR增长率为33%~189%,FLR中位增长率为61%。由于该术式操作相对简单,在腹腔镜下即可完成;如FIR增长不足,还可通过PVE等方法补救,目前在国内外均有成功实施的病例报[31, 57-58]。
5.4 RALPPS
Gall等[18]在2015年提出了以射频消融替代原位肝实质离段的射频消融ALPSS,即在术中B超定位下标记肝切除线后,用射频消融装置沿预设肝切除线由前向后烧灼出1条“无血带”,同时施行门静脉右支结扎;二期手术沿“无血带”行肝切除术。此术式的优点在于不仅有效减轻一期手术引起的腹腔粘连,缩短一、二期手术时间和术中出血,还能大大降低了因施行原位肝实质离段导致的胆汁漏等并发症发生。
5.5 H-ALPPS
Aloia等[59]提出经典ALPPS严重违背“no-touch”肿瘤学原则,将大大降低手术远期疗效。2016年Li等[49]提出H-ALPPS,即前入路的原位肝实质离段联合门静脉栓塞二期肝切除术。该术式尤其适合于肿瘤侵犯门静脉右支的病例,通过栓塞门静脉右支从而避免了对肿瘤的牵拉、挤压,将达到更好的肿瘤根治效果[60-61]。
5.6 TELPP
通过完善血管三维成像,在栓塞门静脉右支的同时,栓塞Ⅴ、Ⅷ段门静脉末梢,以达到完全阻断病肝门静脉血流,其FLR增长率与经典ALPPS无统计学差异[50]。从现有资料来看,TELPP最大的优点在于患者只需接受1次全麻手术,并且避免了施行一期肝实质离段,不仅有效降低了患者的手术创伤,而且大大降低了腹腔粘连、胆汁漏及感染的发生率[62];但由于实施例数有限,其安全性及疗效并不明确[63]。
6 总 结
ALPPS术式的提出可谓是肝脏外科发展史上一个重要的里程碑,极大程度上提高了肝恶性肿瘤患者的手术切除率;但由于ALPPS目前仍是一项新兴的技术,各方面技术不够成熟且存在颇多争议,而由ALPPS衍生的各种术式又缺乏多中心大样本的数据统计支持,未来仍需更多的努力致力于手术方式的改进,在保证足够FLR增生的同时降低手术并发症发生率及病死率。其次,有关ALPPS的基础研究仍处于动物实验阶段,如何让基础研究结果服务于临床是最终目标,比如能否通过人为激活某些信号通路或在肝切除术后加用某些相关刺激肝细胞再生因子以刺激肝细胞再生和促进成肝细胞成熟,最终达到降低术后肝功能衰竭发生率目的等。ALPPS仍处于一个不断探索和创新的阶段,相信外科医生在此领域的临床与基础的研究和探索将大有可为。
[1] Tong YF, Meng N, Chen MQ, et al. Maturity of associating liver partition and portal vein ligation for staged hepatectomy-derived liver regeneration in a rat model[J]. World J Gastroenterol, 2018,24(10):1107-1119. doi:10.3748/wjg.v24.i10.1107.
[2] 彭远飞, 王征, 周俭. 联合肝脏离断和门静脉结扎的二步肝切除术的争议与发展[J]. 外科理论与实践, 2018, 23(3):185-190.doi:10.16139/j.1007-9610.2018.03.001.Peng YF, Wang Z, Zhou J. Controversy and development of associating liver partition and portal vein ligation for staged hepatectomy[J]. Journal of Surgery Concepts & Practice, 2018,23(3):185-190. doi:10.16139/j.1007-9610.2018.03.001.
[3] Kokudo N, Tada K, Seki M, et al. Proliferative activity of intrahepatic colorectal metastases after preoperative hemihepatic portal vein embolization[J]. Hepatology, 2001, 34(2):267-272. doi:10.1053/jhep.2001.26513.
[4] Clavien PA, Petrowsky H, DeOliveira ML, et al. Strategies for safer liver surgery and partial liver transplantation[J]. N Engl J Med,2007, 356(15):1545-1559. doi:10.1056/NEJMra065156.
[5] Schnitzbauer AA, Lang SA, Goessmann H, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings[J]. Ann Surg, 2012, 255(3):405-414. doi:10.1097/SLA.0b013e31824856f5.
[6] Stockmann M, Bednarsch J, Malinowski M, et al. Functional considerations in ALPPS - consequences for clinical management[J]. HPB (Oxford), 2017, 19(11):1016-1025. doi:10.1016/j.hpb.2017.07.010.
[7] Bertens KA, Hawel J, Lung K, et al. ALPPS:challenging the concept of unresectability--a systematic review[J]. Int J Surg, 2015,13:280-287. doi:10.1016/j.ijsu.2014.12.008.
[8] Li J, Girotti P, Königsrainer I, et al. ALPPS in right trisectionectomy:a safe procedure to avoid postoperative liver failure[J]. J Gastrointest Surg, 2013, 17(5):956-961. doi:10.1007/s11605-012-2132-y.
[9] Takamoto T, Sugawara Y, Hashimoto T, et al. Associating liver partition and portal vein ligation (ALPPS):Taking a view of trails[J]. Biosci Trends, 2015, 9(5):280-283. doi:10.5582/bst.2015.01131.
[10] Schadde E, Ardiles V, Robles-Campos R, et al. Early survival and safety of ALPPS:first report of the International ALPPS Registry[J]. Ann Surg, 2014, 260(5):829-836. doi:10.1097/SLA.0000000000000947.
[11] Nadalin S, Capobianco I, Li J, et al. Indications and limits for associating liver partition and portal vein ligation for staged hepatectomy (ALPPS). Lessons Learned from 15 cases at a single centre[J]. Z Gastroenterol, 2014, 52(1):35-42. doi:10.1055/s-0033-1356364.
[12] Vivarelli M, Vincenzi P, Montalti R, et al. ALPPS Procedure for Extended Liver Resections:A Single Centre Experience and a Systematic Review[J]. PLoS One, 2015, 10(12):e0144019. doi:10.1371/journal.pone.0144019.
[13] Alvarez FA, Ardiles V, de Santibañes M, et al. Associating liver partition and portal vein ligation for staged hepatectomy offers high oncological feasibility with adequate patient safety:a prospective study at a single center[J]. Ann Surg, 2015, 261(4):723-732. doi:10.1097/SLA.0000000000001046.
[14] Hasselgren K, Sandström P, Björnsson B. Role of associating liver partition and portal vein ligation for staged hepatectomy in colorectal liver metastases:a review[J]. World J Gastroenterol,2015, 21(15):4491-4498. doi:10.3748/wjg.v21.i15.4491.
[15] Yao L, Li C, Ge X, et al. Establishment of a rat model of portal vein ligation combined with in situ splitting[J]. PLoS One, 2014,9(8):e105511. doi:10.1371/journal.pone.0105511.
[16] Schadde E, Hertl M, Breitenstein S, et al. Rat Model of the Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS) Procedure[J]. J Vis Exp, 2017, (126). doi:10.3791/55895.
[17] 林为东, 莫经刚. ALPPS促进剩余肝脏快速增生机制及相关因素研究进展[J]. 中国普通外科杂志, 2017, 26(8):1065-1070.doi:10.3978/j.issn.1005-6947.2017.08.016.Lin WD, Mo JG. Mechanisms of ALPPS promoting rapid hypertrophy of future liver remnant and relevant factors:recent advances[J]. Chinese Journal of General Surgery, 2017, 26(8):1065-1070. doi:10.3978/j.issn.1005-6947.2017.08.016.
[18] Gall TM, Sodergren MH, Frampton AE, et al. Radio-frequencyassisted Liver Partition with Portal vein ligation (RALPP) for liver regeneration[J]. Ann Surg, 2015, 261(2):e45-46. doi:10.1097/SLA.0000000000000607.
[19] Schlegel A, Lesurtel M, Melloul E, et al. ALPPS:from human to mice highlighting accelerated and novel mechanisms of liver regeneration[J]. Ann Surg, 2014, 260(5):839-846. doi:10.1097/SLA.0000000000000949.
[20] Shi H, Yang G, Zheng T, et al. A preliminary study of ALPPS procedure in a rat model[J]. Sci Rep, 2015, 5:17567. doi:10.1038/srep17567.
[21] Dhar DK, Mohammad GH, Vyas S, et al. A novel rat model of liver regeneration:possible role of cytokine induced neutrophil chemoattractant-1 in augmented liver regeneration[J]. Ann Surg Innov Res, 2015, 9:11. doi:10.1186/s13022-015-0020-3.
[22] 黄民, 黄粲宸, 肖乐, 等. ALPPS一期术后肝内干/祖细胞的变化及其与肝再生的关系[J]. 中国普通外科杂志, 2018, 27(2):210-218.doi:10.3978/j.issn.1005-6947.2018.02.013.Huang M, Huang CC, Xiao L, et al. Alteration in intrahepatic stem/progenitor cells after first stage of ALPPS and its relationship to liver regeneration[J]. Chinese Journal of General Surgery, 2018,27(2):210-218. doi:10.3978/j.issn.1005-6947.2018.02.013.
[23] Sala S, Ardiles V, Ulla M, et al. Our initial experience with ALPPS technique:encouraging results[J]. Updates Surg, 2012, 64(3):167-172. doi:10.1007/s13304-012-0175-y.
[24] Alvarez FA, Ardiles V, Sanchez CR, et al. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS):tips and tricks[J]. J Gastrointest Surg, 2013, 17(4):814-821. doi:10.1007/s11605-012-2092-2.
[25] Torres OJ, Fernandes Ede S, Oliveira CV, et al. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS):the Brazilian experience [J]. Arq Bras Cir Dig, 2013, 26(1):40-43.
[26] Buac S, Schadde E, Schnitzbauer AA, et al. The many faces of ALPPS:surgical indications and techniques among surgeons collaborating in the international registry[J]. HPB (Oxford), 2016,18(5):442-448. doi:10.1016/j.hpb.2016.01.547.
[27] Oldhafer KJ, Stavrou GA, van Gulik TM, et al. ALPPS--Where Do We Stand, Where Do We Go?:Eight Recommendations From the First International Expert Meeting[J]. Ann Surg, 2016, 263(5):839-841. doi:10.1097/SLA.0000000000001633.
[28] Joechle K, Moser C, Ruemmele P, et al. ALPPS (associating liver partition and portal vein ligation for staged hepatectomy) does not affect proliferation, apoptosis, or angiogenesis as compared to standard liver resection for colorectal liver metastases[J]. World J Surg Oncol, 2017, 15(1):57. doi:10.1186/s12957-017-1121-8.
[29] Fukami Y, Kurumiya Y, Kobayashi S. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS):an analysis of tumor activity[J]. Updates Surg, 2014, 66(3):223-225.doi:10.1007/s13304-014-0256-1.
[30] Oldhafer KJ, Donati M, Jenner RM, et al. ALPPS for patients with colorectal liver metastases:effective liver hypertrophy, but early tumor recurrence[J]. World J Surg, 2014, 38(6):1504-1509. doi:10.1007/s00268-013-2401-2.
[31] Xu J, Lu X, Zhang Y, Yet al. Laparoscopic associating liver tourniquet and portal ligation combined rescue transhepatic arterial embolization for staged hepatectomy:A case report[J].Medicine (Baltimore), 2017, 96(43):e8378. doi:10.1097/MD.0000000000008378.
[32] Li J, Ewald F, Gulati A, et al. Associating liver partition and portal vein ligation for staged hepatectomy:From technical evolution to oncological benefit[J]. World J Gastrointest Surg, 2016, 8(2):124-133. doi:10.4240/wjgs.v8.i2.124.
[33] Donati M, Stavrou GA, Oldhafer KJ. Current position of ALPPS in the surgical landscape of CRLM treatment proposals[J]. World J Gastroenterol, 2013, 19(39):6548-6554. doi:10.3748/wjg.v19.i39.6548.
[34] Ardiles V, Schadde E, Santibanes E, et al. Commentary on"Happy marriage or "dangerous liaison":ALPPS and the anterior approach"[J]. Ann Surg, 2014, 260(2):e4. doi:10.1097/SLA.0000000000000735.
[35] Dokmak S, Belghiti J. Which limits to the "ALPPS" approach[J].Ann Surg, 2012, 256(3):e6. doi:10.1097/SLA.0b013e318265fd64.
[36] Torres OJ, Fernandes ES, Herman P. ALPPS:past, present and future[J]. Arq Bras Cir Dig, 2015, 28(3):155-156. doi:10.1590/S0102-67202015000300001.
[37] Chaudhari P, Tian L, Deshmukh A, et al. Expression kinetics of hepatic progenitor markers in cellular models of human liver development recapitulating hepatocyte and biliary cell fate commitment[J]. Exp Biol Med (Maywood), 2016, 241(15):1653-1662. doi:10.1177/1535370216657901.
[38] Serenari M, Collaud C, Alvarez FA, et al. Interstage Assessment of Remnant Liver Function in ALPPS Using Hepatobiliary Scintigraphy:Prediction of Posthepatectomy Liver Failure and Introduction of the HIBA Index[J]. Ann Surg, 2018, 267(6):1141-1147. doi:10.1097/SLA.0000000000002150.
[39] Truant S, Baillet C, Deshorgue AC, et al. Contribution of hepatobiliary scintigraphy in assessing ALPPS most suited timing[J]. Updates Surg, 2017, 69(3):411-419. doi:10.1007/s13304-017-0481-5.
[40] Sparrelid E, Jonas E, Tzortzakakis A, et al. Dynamic Evaluation of Liver Volume and Function in Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy[J]. J Gastrointest Surg, 2017,21(6):967-974. doi:10.1007/s11605-017-3389-y.
[41] Lau WY, Lai EC, Lau SH. Associating liver partition and portal vein ligation for staged hepatectomy:the current role and development[J]. Hepatobiliary Pancreat Dis Int, 2017, 16(1):17-26.
[42] Uribe M, Uribe-Echevarría S, Mandiola C, et al. Insight on ALPPS- Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy - mechanisms:activation of mTOR pathway[J].HPB (Oxford), 2018, pii:S1365-182X(18)30725-1. doi:10.1016/j.hpb.2018.02.636. [Epub ahead of print]
[43] Petrowsky H, Györi G, de Oliveira M, et al. Is partial-ALPPS safer than ALPPS? A single-center experience[J]. Ann Surg, 2015,261(4):e90-92. doi:10.1097/SLA.0000000000001087.
[44] Hernandez-Alejandro R, Bertens KA, Pineda-Solis K, et al. Can we improve the morbidity and mortality associated with the associating liver partition with portal vein ligation for staged hepatectomy (ALPPS) procedure in the management of colorectal liver metastases?[J]. Surgery, 2015, 157(2):194-201. doi:10.1016/j.surg.2014.08.041.
[45] 张国民, 缪宁, 郑徽, 等. 中国2005-2016年乙型病毒性肝炎报告发病的年龄和地区特征[J]. 中国疫苗和免疫, 2018, 24(2):121-126.Zhang GM, Miao N, Zheng H, et al. Incidence by age and region of hepatitis B reported in China from 2005 to 2016[J]. Chinese Journal of Vaccines and Immunization, 2018, 24(2):121-126.
[46] 彭驰涵, 李川, 文天夫, 等. 原发性肝癌行ALPPS的适应证与禁忌证初探(附15例报道) [J]. 中国普外基础与临床杂志, 2015,22(10):1183-1186.Peng CH, Li C, Wen TF, et al. Discussion about The Indications and Contradictions of ALPPS for Primary Hepatoce-Uular Carcinoma Patients (Reports of 15 Cases)[J]. Chinese Journal of Bases and Clinics In General Surgery, 2015, 22(10):1183-1186.
[47] Machado MA, Makdissi FF, Surjan RC, et al. Transition from open to laparoscopic ALPPS for patients with very small FLR:the initial experience[J]. HPB (Oxford), 2017, 19(1):59-66. doi:10.1016/j.hpb.2016.10.004.
[48] Robles R, Parrilla P, López-Conesa A, et al. Tourniquet modification of the associating liver partition and portal ligation for staged hepatectomy procedure[J]. Br J Surg, 2014, 101(9):1129-1134. doi:10.1002/bjs.9547.
[49] Li J, Kantas A, Ittrich H, et al. Avoid "All-Touch" by Hybrid ALPPS to Achieve Oncological Efficacy[J]. Ann Surg, 2016, 263(1):e6-7.doi:10.1097/SLA.0000000000000845.
[50] 彭淑牖, 黄从云, 李江涛, 等. 末梢门静脉栓塞术在计划性肝切除术中的应用初探[J]. 中华外科杂志, 2016, 54(9):664-668.doi:10.3760/cma.j.issn.0529-5815.2016.09.004.Peng SY, Huang CY, Li JT, et al. Terminal branches portal vein embolization for planed hepatectomy[J]. Chinese Journal of Surgery, 2016, 54(9):664-668. doi:10.3760/cma.j.issn.0529-5815.2016.09.004.
[51] Reich H, McGlynn F, DeCaprio J, e al. Laparoscopic excision of benign liver lesions[J]. Obstet Gynecol, 1991, 78(5 Pt 2):956-958.
[52] Cai X. Laparoscopic liver resection:the current status and the future[J]. Hepatobiliary Surg Nutr, 2018, 7(2):98-104. doi:10.21037/hbsn.2018.02.07.
[53] Schelotto PB, Gondolesi G. Laparoscopy in ALPPS Procedure:When We Can Do It[J]. Ann Surg, 2017, 265(4):e30-31. doi:10.1097/SLA.0000000000000834.
[54] Akyuz M, Yazici P, Yigitbas H, et al. Oncologic results of laparoscopic liver resection for malignant liver tumors[J]. J Surg Oncol, 2016, 113(2):127-129. doi:10.1002/jso.24119.
[55] Tanaka K, Kikuchi Y, Kawaguchi D, et al. Modified ALPPS Procedures Avoiding Division of Portal Pedicles[J]. Ann Surg,2017, 265(2):e14-20. doi:10.1097/SLA.0000000000001967.
[56] Robles Campos R, Parrilla Paricio P, López Conesa A, et al. A new surgical technique for extended right hepatectomy:tourniquet in the umbilical fissure and right portal vein occlusion (ALTPS).Clinical case[J]. Cir Esp, 2013, 91(10):633-637. doi:10.1016/j.ciresp.2013.09.004.
[57] Robles Campos R, Brusadin R, López Conesa A, et al. Staged liver resection for perihilar liver tumors using a tourniquet in the umbilical fissure and sequential portal vein embolization on the fourth postoperative day (a modified ALTPS) [J]. Cir Esp, 2014,92(10):682-686. doi:10.1016/j.ciresp.2014.07.006.
[58] López-López V, Robles-Campos R, Brusadin R, et al. Tourniquet-ALPPS is a promising treatment for very large hepatocellular carcinoma and intrahepatic cholangiocarcinoma[J]. Oncotarget,2018, 9(46):28267-28280. doi:10.18632/oncotarget.25538.
[59] Aloia TA, Vauthey JN. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS):what is gained and what is lost?[J]. Ann Surg, 2012, 256(3):e9. doi:10.1097/SLA.0b013e318265fd3e.
[60] Cai YL, Song PP, Tang W, et al. An updated systematic review of the evolution of ALPPS and evaluation of its advantages and disadvantages in accordance with current evidence[J].Medicine (Baltimore), 2016, 95(24):e3941. doi:10.1097/MD.0000000000003941.
[61] Lai Q, Melandro F, Rossi M. Hybrid Partial ALPPS:a Feasible Approach in Case of Right Trisegmentectomy and Macrovascular Invasion[J]. Ann Surg, 2018, 267(4):e80-82. doi:10.1097/SLA.0000000000002219.
[62] Peng SY, Wang XA, Huang CY, et al. Evolution of associating liver partition and portal vein ligation for staged hepatectomy:Simpler,safer and equally effective methods[J]. World J Gastroenterol, 2017,23(23):4140-4145. doi:10.3748/wjg.v23.i23.4140.
[63] Xiao N, Yu K, Yu S, et al. The paradigm of tumor shrinkage and rapid liver remnant hypertrophy for conversion of initially unresectable colorectal liver metastasis:a case report and literature review[J]. World J Surg Oncol, 2017, 15(1):148. doi:10.1186/s12957-017-1212-6.
