凶险性前置胎盘是妊娠晚期可能的最严重并发症之一,其定义为既往有剖宫产史,此次妊娠为前置胎盘,且胎盘附着于子宫瘢痕部位[1]。凶险性前置胎盘常合并胎盘植入,常导致难以控制的大出血,大大增加了围产期风险,有时为了拯救产妇生命不得不进行子宫切除,造成不可逆的生育功能丧失[2]。随着二胎政策施行,剖宫产手术后再次妊娠及高龄孕妇比例增加,凶险性前置胎盘合并胎盘植入发病率明显上升[3]。所以,如何有效地在凶险性前置胎盘合并胎盘植入剖宫产手术中预防大出血,是当前亟待解决的问题。近年来,国内外各产科中心相继开展了透视下的低位腹主动脉球囊阻断(lower abdominal aortic balloon occlusion,LABO),减少出血的效果肯定[4-6]。随着介入手术的开展增多,手术并发症例如动脉损伤、狭窄、血栓形成等也随之不断出现[7-10]。另一种在凶险性前置胎盘剖宫产术中预防大出血的方法为开放腹主动脉暂时阻断(temporary abdominal aortic ligation,TAL),目前报道较少[11-13],尚未有对这两种预防大出血的血管阻断方法的应用进行对比的研究报告。本研究回顾性分析2016年1月—2018年7月住院分娩的凶险性前置胎盘合并胎盘植入患者共84例临床资料,对比这两种腹主动脉阻断手术方法应用的优劣。
1 资料与方法
1.1 资料来源
采用回顾性临床病例对照研究方法。收集2016年1月—2018年7月在湖南省妇幼保健院住院分娩的凶险性前置胎盘合并胎盘植入患者临床资料共84例,其中从2016年1月—2016年12月的所有患者(36例)采用LABO止血,从2017年1月—2018年7月所有患者(48例)采用TAL止血。该研究通过我院伦理委员会审批,患者及家属均签署知情同意书。
1.2 纳入标准与排除标准
纳入标准:⑴年龄20~45岁,既往有剖宫产史。⑵妊娠28~37周,此次妊娠超声诊断为前置胎盘,且胎盘附着于子宫瘢痕部位。⑶两组患者的手术前超声诊断及评估由同一组超声医生执行,同时符合胎盘植入的5条标准之一[14]:胎盘后低回声带消失;胎盘陷窝,内可见高速血流,即“奶酪征、沸水征”;“膀胱线”中断或消失;胎盘基底部异常的血管:弓形动脉走行呈节段性血流信号中断,呈簇状、团状血流;跨界血管(膀胱充盈时可观察到子宫壁上呈“梳状”穿支血流)。⑷患者及其委托代理人签署知情同意书。排除标准:⑴术前超声或核磁共振检查未到达凶险性前置胎盘合并胎盘植入的诊断。⑵急诊手术。⑶剖宫产手术中,胎儿娩出后胎盘娩出前再次评估,排除凶险性前置胎盘合并胎盘植入的诊断。
1.3 手术方法
1.3.1 TAL 由同一组血管外科医生执行。以典型病例为例,取下腹部正中切口绕脐上2 cm,胎儿娩出后,不剥离胎盘,先用压脉带捆扎子宫(图1),再次评估胎盘植入程度,需做TAL者,在主髂动脉分叉处切开后腹膜长约4 cm,并于分叉处上方2 cm处游离长约1.5 cm的一段腹主动脉,用硅胶阻断带绕过腹主动脉,拉紧阻断带阻断腹主动脉血流(图2)。更精确的阻断部位在第4对腰动脉和腹主动脉分叉之间,该段腹主动脉基本没有分支血管,在过阻断带时一般不会出血,也避免了过多腰动脉阻断可能导致的脊髓缺血损伤(图3)。阻断开始同时静脉注射肝素25 mg并记录阻断时间,视胎盘植入及产时出血情况采用各种方法止血,进行产科手术操作。大出血控制后松开阻断带,静脉注射等量鱼精蛋白对抗肝素,阻断时间如果超过30 min,视情况放松阻断带5~10 min,再阻断20~30 min。

图1 压脉带捆扎子宫
Figure 1 Compression of the uterus with a pressure band

图2 拉紧阻断带阻断腹主动脉血流
Figure 2 Blocking the blood fl ow of the abdominal aorta by tightening the occlusion band

图3 精确阻断部位
Figure 3 The accurate site of occlusion
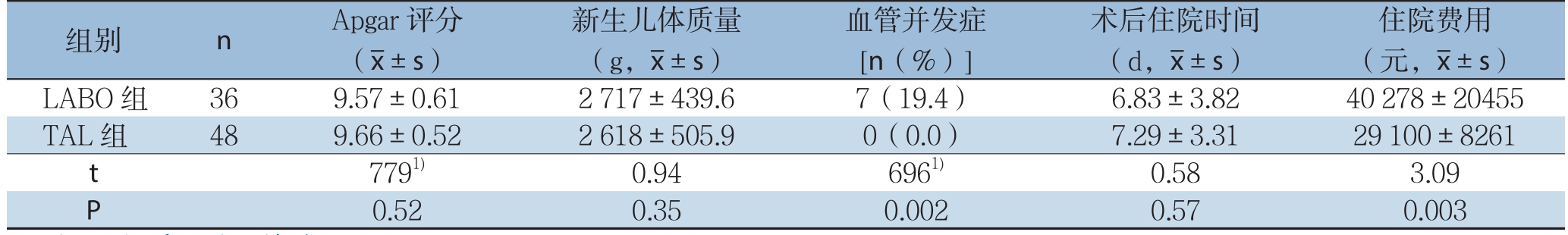
1.3.2 LABO 由同一组介入科医师执行。患者剖宫产术前于介入手术室,常规消毒、局部麻醉后Seldinger法穿刺右侧股动脉,置入12 F血管鞘,经鞘管置入导丝,导入12 F AB46顺应性球囊(Medtronic,Inc.,USA),透视下将球囊送入腹主动脉肾动脉水平以下位置,先不充盈球囊。随后将患者推入常规手术室,产科医师行剖宫产手术,胎儿娩出后,不剥离胎盘,同样先用压脉带捆扎子宫,随即向腹主动脉球囊内注入7~10 mL生理盐水,使球囊充盈以阻断腹主动脉血流,直至双侧股动脉搏动消失(图4)。阻断开始同时静脉注射25 mg肝素,记录阻断开始时间,产科医师视胎盘植入及出血情况采用各种方法止血。大出血控制后,抽出球囊内生理盐水,静脉注射鱼精蛋白25 mg对抗肝素作用,阻断时间不超过30 min。若阻断时间长于30 min,视情况放松球囊压力5~10 min后再阻断20~30min。关腹后,拔除球囊导管,股动脉穿刺部位局部压迫30 min,止血后加压包扎24 h。
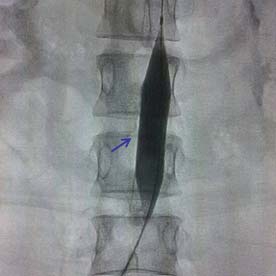
图4 腹主动脉球囊充盈阻断血流
Figure 4 Blood fl ow occlusion by infl ation of the abdominal aortic balloon
1.3.3 剖宫产手术及其后产科止血 均由同一组高年资产科医师主刀,术中采用宫缩药物、缝合、血管结扎及子宫填塞等方法止血。子宫切除标准[15]:⑴保守手术治疗如双侧子宫/髂内动脉结扎/子宫压迫缝合无法控制出血;⑵宫颈胎盘植入失去正常形态时。
1.4 观察指标
术前情况:两组患者年龄、孕产次、分娩间隔时间、分娩孕周、术前胎盘超声评分比较。根据胎盘植入的超声评分[14],胎盘植入根据严重程度分为粘连型、植入型和穿透型3类。胎盘植入超声评分中包括胎盘位置、胎盘厚度、胎盘后低回声带、膀胱线、胎盘陷窝、胎盘基底部血流、宫颈血窦、宫颈形态、剖宫产史等内容,最高分为18分,评分≤5分提示无植入或粘连型胎盘植入;评分6~10分提示植入型胎盘植入;评分≥11分提示穿透型胎盘植入。手术相关指标:两组患者剖宫产手术时间、手术中出血量、输浓缩红细胞量、子宫切除率。术后及新生儿情况:新生儿Apgar评分、新生儿体质量、术后血管相关并发症(例如动脉血栓形成、血管损伤、假性动脉瘤等)情况、术后住院时间、住院费用。出血量统计采用容积法及称重法,血管并发症均通过超声及CTA获得明确诊断。
1.5 统计学处理
采用GraphPad Prism 8.0.2软件对数据进行统计学处理。计量资料以均数±标准差( ±s)表示,两组间比较采用独立样本t检验;计数资料采用率表示,组间比较采用Mann-Whitney秩和检验。P<0.05为差异有统计学意义。
±s)表示,两组间比较采用独立样本t检验;计数资料采用率表示,组间比较采用Mann-Whitney秩和检验。P<0.05为差异有统计学意义。
2 结果
2.1 两组患者术前情况的比较
两组患者在年龄、孕产次、前次妊娠间隔时间、术前胎盘超声评分的差异均无统计学意义(均P>0.05)(表1)。
表1 两组术前情况的比较( ±s)
±s)
Table 1 Comparison of the preoperative variables between the two groups( ±s)
±s)
注:1)采用秩和检验
Note:1)Using rank-sum test
组别 n 年龄(岁) 孕次(次) 分娩间隔(年) 分娩孕周(周) 术前胎盘超声评分LABO 组 36 32.22±4.25 3.97±1.42 6.94±3.62 35.70±2.12 7.88±2.13 TAL 组 48 32.40±4.23 3.79±1.18 6.77±3.45 36.20±1.73 8.39±2.24 t 0.19 0.63 0.22 1.19 8881)P 0.85 0.53 0.82 0.24 0.23
2.2 两组患者手术相关指标的比较
LABO组和TAL组两组患者的剖宫产手术时间、手术中出血量、输浓缩红细胞量、子宫切除率分别比较,差异均无统计学意义(均P>0.05)(表2)。
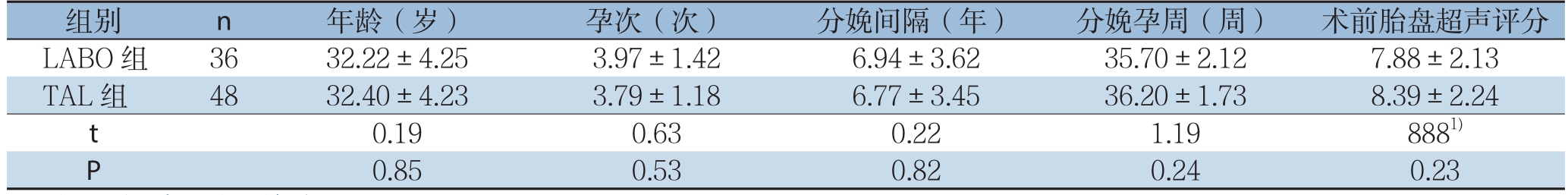
表2 两组手术相关指标的比较( ±s)
±s)
Table 2 Comparison of the surgery-related variables between the two groups( ±s)
±s)
注:1)采用秩和检验
Note:1)Using rank-sum test
输浓缩红细胞量(mL,x±s) 子宫切除[n(%)]LABO 组 36 102.9±22.3 1 785±1241 752.8±1269 10(27.8)TAL 组 48 106.3±21.9 2 149±1644 785.4±825.1 10(20.8)t 0.71 1.11 0.13 8041)P 0.48 0.27 0.89 0.61组别 n 手术时间(min,x±s) 手术中出血量(mL,x±s)
2.3 术后及新生儿情况的比较
LABO组和TAL组两组患者的新生儿评分、新生儿体质量、术后住院时间相比较,差异均无统计学意义(均P>0.05);住院费用的比较差异有统计学意义(P<0.05),TAL组更低。血管并发症率比较,TAL组48例手术后均无血栓或血管损伤等并发症发生;LABO组36例中7例术后出现血管并发症(髂外动脉动脉血栓栓塞4例,股动脉血栓栓塞1例,假性动脉瘤形成2例),血管并发症发生率比较有统计学意义(P<0.05)(表3)。
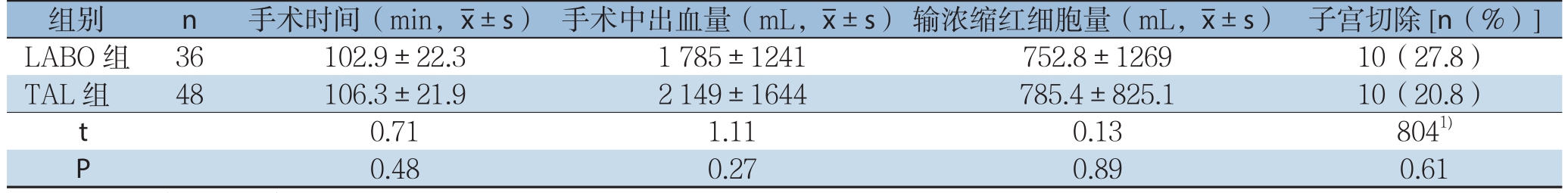
表3 两组术后相关指标及新生儿情况比较( ±s)
±s)
Table 3 Comparison of the postoperative variables and newborns' conditions between the two groups( ±s)
±s)
注:1)采用秩和检验
Note:1)Using rank-sum test
住院费用(元,x±s)LABO组 36 9.57±0.61 2 717±439.6 7(19.4) 6.83±3.82 40 278±20455 TAL组 48 9.66±0.52 2 618±505.9 0(0.0) 7.29±3.31 29 100±8261 t 7791) 0.94 6961) 0.58 3.09 P 0.52 0.35 0.002 0.57 0.003组别 n Apgar评分(x±s)新生儿体质量(g,x±s)血管并发症[n(%)]术后住院时间(d,x±s)
3 讨论
凶险性前置胎盘往往伴有胎盘植入,妊娠晚期增大的血流量加上局部密集而质脆的血管丛,使得难以进行安全和快速的胎盘剥离[16]。胎盘前置并植入的病例出血量可达3 000~5 000 mL,有些病例可多达10 000 mL[17]。凶险性前置胎盘已经是妊娠子宫切除的最重要原因之一[2,18-20]。凶险性前置胎盘合并胎盘植入剖宫产手术如何有效减少出血量、预防子宫切除,是妇产科/血管外科医生一直以来特别关注的问题。盆腔血供由丰富的、互相交错的血管网络构成,阻断任意分支均可立即由其他血管代偿,而这些血供主要来自髂内动脉及其分支,少部分来自腹主动脉、髂外动脉和股动脉的侧支循环吻合支,故通过阻断腹主动脉主干来控制出血效果更加直接。1992年Alvarez等[21]首次报道5例具有产科出血高危因素的患者术前预置腹主动脉球囊,起到良好效果。该技术也于近年来在全世界得到广泛应用,在减少剖宫产手术中出血效果肯定[4-6,22-24]。与LABO相比,TAL目前报道较少,有采用Cosgrove Flex Clamp对腹主动脉进行钳夹来阻断血流,或采用硅胶管阻断腹主动脉血流的报道,均取得较好的止血效果[11-12]。本研究回顾性分析比较了我院近年来开展的TAL和LABO两种血管阻断止血方法,发现它们在凶险性前置胎盘合并胎盘植入剖宫产手术中的止血效果差异无统计学意义,并且术后血管并发症发生率明显下降。术后下肢动脉血栓栓塞与假性动脉瘤形成是LABO的主要并发症[9,25-27]。在本研究中,36例行LABO的患者也有7例出现急性下肢动脉血栓栓塞、假性动脉瘤血管并发症,通过动脉切开取栓、人工血管置换等手术成功处理[28-29]。而48例TAL患者无一发生。经过查阅文献学习,笔者认为LABO后血管并发症风险较TAL高的可能机制为:⑴血管内皮受损具有促血栓形成作用:激活血小板、刺激凝血过程、阻止纤维蛋白溶解。血管内皮损伤是启动血栓形成最重要因素[30];LABO选择的血管鞘为12 F(约4 mm),当血管鞘自股动脉通过髂外动脉、髂总动脉放至肾下腹主动脉时,鞘管可对血管内皮造成损伤,而损伤后内皮下组织暴露,血小板黏附、聚集可形成血栓。而TAL是在腹主动脉外壁直接利用输液器硅胶管施加压力,避免了对血管内皮可能的损伤,对于减少血栓的形成起到部分作用。⑵血流动力学改变:正常血流是层流状态,细胞成分位于血管腔的中间,血浆位于周边。LABO术毕拔除鞘管后,机械压迫股动脉穿刺点30 min止血,当压迫力量过大完全阻断股动脉血流时血流动力学发生改变,当血流瘀滞或者发生涡流时可以增加动脉内血栓形成机会。也有研究显示术后血栓形成发病率可能和使用球囊直径有关,直径越大导致血管损伤、血栓发生率越高[30-31]。由于TAL不会对股动脉或者外周动脉造成穿刺损伤,因此也不需要进行相应的血管压迫止血,因此血流动力学方面的影响也可以减到最少。另外,假性动脉瘤的发生可能由于拔鞘管后压迫不充分或凝血功能异常,血液自穿刺点破口流出被邻近组织包裹形成血肿所致。
除了血管并发症风险明显降低以外,笔者认为TAL相比LABO,还具有如下优点:⑴操作简单,无需额外增加手术切口;⑵能在剖宫产手术中完成,无需转移至介入室;⑶几乎没有增加成本,而LABO平均增加约10 000元费用;⑷减少辐射,相比LABO,TAL无辐射暴露,有研究[31]认为,胎儿受辐射剂量超过150 mGy,与未受辐射胎儿相比,畸形发生率多出0.05%;⑸LABO必须从介入手术室置管后转送到普通手术室,在转运过程中可能有污染、导管移位的风险。最早由Chou等[13]报道采用Cosgrove Flex Clamp对腹主动脉进行钳夹来阻断血流,本组选择了Long等[12]报道的采用无菌输液器硅胶管作为阻断带的方法,认为此种方法可能会比金属钳夹损伤更小。并且相比前述报道的TAL个案或小样本研究,笔者中心在开展手术例数、手术流程优化等方面已经处于领先的位置。但需注意的是,TAL在操作时可能导致腰动脉出血等并发症,存在一定风险,最好由有经验的普通外科/血管外科医生完成。总之TAL是一种安全有效的应用于凶险型前置胎盘合并胎盘植入剖宫产术中止血的方法。该项技术与LABO疗效同样肯定,且并发症率更低,也更具医学经济学价值,值得在具有血管外科辅助条件的妇产科中心推广。
[1]Chattopadhyay SK,Kharif H,Sherbeeni MM.Placenta praevia and accreta after previous caesarean section[J].Eur J Obstet Gynecol Reprod Biol,1993,52(3):151-156.doi:10.1016/0028-2243(93)90064-j.
[2]陈静,李秋玲,那全,等.前置胎盘致围产期子宫切除患者的临床分析[J].中国医科大学学报,2015,44(4):315-318.Chen J,Li QL,Na Q,et al.Clinical Analysis on Peripartum Hysterectomy Due to Placenta Previa[J].Journal of China Medical University,2015,44(4):315-318.
[3]陈静,那全,庄艳艳,等.凶险型前置胎盘128例临床分析[J].中国实用妇科与产科杂志,2015,31(6):539-542.Chen J,Na Q,Zhuang YY,et al.Clinical analysis of 128 cases of pernicious placenta previa[J].Chinese Journal of Practical Gynecology and Obstetrics,2015,31(6):539-542.
[4]Zhou X,Sun X,Wang M,et al.The effectiveness of prophylactic internal iliac artery balloon occlusion in the treatment of patients with pernicious placenta previa coexisting with placenta accreta[J].J Matern Fetal Neonatal Med,2019,9:1-6.doi:10.1080/14767058.2019.1599350.
[5]Dai MJ,Jin GX,Lin JH,et al.Pre-cesarean prophylactic balloon placement in the internal iliac artery to prevent postpartum hemorrhage among women with pernicious placenta previa[J].Int J Gynaecol Obstet,2018,142(3):315-320.doi:10.1002/ijgo.12559.
[6]Sun W,Duan S,Xin G,et al.Safety and efficacy of preoperative abdominal Aortic balloon occlusion in placenta increta and/or percreta[J].J Surg Res,2018,222:75-84.doi:10.1016/j.jss.2017.10.002.
[7]苏放明,张海鹰,王英兰,等.腹主动脉预置管球囊阻滞预防凶险型前置胎盘合并胎盘植入大出血1例报道[J].现代妇产科进展,2013,22(3):244-245.Su FM,Zhang HY,Wang YL,et al.Preplacement of balloon of the abdominal aorta for preventing massive hemorrhage in one patient with dangerous placenta previa complicated by placenta accreta[J].Progress in Obstetrics and Gynecology,2013,22(3):244-245.
[8]Dilauro MD,Dason S,Athreya S.Prophylactic balloon occlusion ofinternal iliac arteries in women with placenta accreta:literature review and analysis[J].Clin Radiol,2012,67(6):515-520.doi:10.1016/j.crad.2011.10.031.
[9]Bishop S,Butler K,Monaghan S,et al.Multiple complications following the use of prophylactic internal iliac artery balloon catheterisation in a patient with placenta percreta[J].Int J Obstet Anesth,2011,20(1):70-73.doi:10.1016/j.ijoa.2010.09.012.
[10]曾鸿,王妍,王阳,等.穿透型胎盘植入行腹主动脉球囊置入的围术期管理1例[J].北京大学学报:医学版,2015,47(6):1031-1033.doi:10.3969/j.issn.1671-167X.2015.06.026.Zeng H,Wang Y,Wang Y,et al.Perioperative management of abdominal aortic balloon occlusion in patients complicated with placenta percteta:a case report[J].Journal of Peking University:Health Sciences,2015,47(6):1031-1033.doi:10.3969/j.issn.1671-167X.2015.06.026.
[11]黄双英,夏爱斌,Grace Jamail,等.腹主动脉暂时阻断术在凶险型前置胎盘剖宫产术中的临床效果[J].中南大学学报:医学版,2017,42(3):313-319.doi:10.11817/j.issn.1672-7347.2017.03.013.Huang SY,Xia AB,Jamail G,et al.Efficacy of temporary ligation ofinfrarenal abdominal aorta during cesarean section in pernicious placenta previa[J].Journal of Central South University:Medical Science,2017,42(3):313-319.doi:10.11817/j.issn.1672-7347.2017.03.013.
[12]Long ML,Cheng CX,Xia AB,et al.Temporary loop ligation of the abdominal aorta during cesarean hysterectomy for reducing blood loss in placenta accrete[J].Taiwan J Obstet Gynecol,2015,54(3):323-325.doi:10.1016/j.tjog.2014.08.006.
[13]Chou MM,Ke YM,Wu HC,et al.Temporary cross-clamping of the infrarenal abdominal aorta during cesarean hysterectomy to control operative blood loss in placenta previa increta/percreta[J].Taiwan J Obstet Gynecol,2010,49(1):72-76.doi:10.1016/S1028-4559(10)60013-7.
[14]李琴,邓学东,王中阳,等.凶险型前置胎盘合并胎盘植入的产前超声诊断分析[J].中华医学超声杂志:电子版,2016,13(3):218-223.doi:10.3877/cma.j.issn.1672-6448.2016.03.011.Li Q,Deng XD,Wang ZY,et al.The prenatal ultrasonic diagnosis of pernicious placenta previa disease complex with placenta implantation[J].Chinese Journal of Medical Ultrasound:Electronic Edition,2016,13(3):218-223.doi:10.3877/cma.j.issn.1672-6448.2016.03.011.
[15]Sentilhes L,Vayssière C,Deneux-Tharaux C,et al.Postpartum hemorrhage:guidelines for clinical practice from the French College of Gynaecologists and Obstetricians(CNGOF):in collaboration with the French Society of Anesthesiology and Intensive Care(SFAR)[J].Eur J Obstet Gynecol Reprod Biol,2016,198:12-21.doi:10.1016/j.ejogrb.2015.12.012.
[16]Palacios Jaraquemada JM,García Mónaco R,Barbosa NE,et al.Lower uterine blood supply:extrauterine anastomotic system and its application in surgical devascularization techniques[J].Acta Obstet Gynecol Scand,2007,86(2):228-234.doi:10.1080/00016340601089875.
[17]Hudon L,Belfort MA,Broome DR.Diagnosis and management of placenta percreta:a review[J].Obstet Gynecol Surv,1998,53(8):509-517.doi:10.1097/00006254-199808000-00024.
[18]Jin R,Guo Y,Chen Y.Risk factors associated with emergency peripartum hysterectomy[J].Chin Med J(Engl),2014,127(5):900-904.
[19]Zeng C,Yang M,Ding Y,et al.Placenta accreta spectrum disorder trends in the context of the universal two-child policy in China and the risk of hysterectomy[J].Int J Gynaecol Obstet,2018,140(3):312-318.doi:10.1002/ijgo.12418.
[20]Chou MM,Kung HF,Hwang JI,et al.Temporary prophylactic intravascular balloon occlusion of the common iliac arteries before cesarean hysterectomy for controlling operative blood loss in abnormal placentation[J].Taiwan J Obstet Gynecol,2015,54(5):493-498.doi:10.1016/j.tjog.2014.03.013.
[21]Alvarez M,Lockwood C J,Ghidini A,et al.Prophylactic and emergent arterial catheterization for selective embolization in obstetric hemorrhage[J].Am J Perinatol,1992,9(5/6):441-444.doi:10.1055/s-2007-999284.
[22]张伟.前置胎盘剖宫产术中髂内动脉栓塞与低位腹主动脉球囊阻断比较研究[J].介入放射学杂志,2018,27(4):322-326.doi:10.3969/j.issn.1008-794X.2018.04.008.Zhang W.Internal iliac artery embolization vs lower abdominal aortic balloon occlusion in cesarean section for delivery women with placenta previa:a comparative study[J].Journal of Interventional Radiology,2018,27(4):322-326.doi:10.3969/j.issn.1008-794X.2018.04.008.
[23]Qiu Z,Hu J,Wu J,et al.Prophylactic temporary abdominal aorta balloon occlusion in women with placenta previa accretism during late gestation[J].Medicine(Baltimore),2017,96(46):e8681.doi:10.1097/MD.0000000000008681.
[24]Fan Y,Gong X,Wang N,et al.A prospective observational study evaluating the efficacy of prophylactic internal iliac artery balloon catheterization in the management of placenta previa-accreta:A STROBE compliant article[J].Medicine(Baltimore),2017,96(45):e8276.doi:10.1097/MD.0000000000008276.
[25]Luo F,Wu Z,Mei J,et al.Thrombosis after aortic balloon occlusion during cesarean delivery for abnormally invasive placenta[J].Int J Obstet Anesth,2018,33:32-39.doi:10.1016/j.ijoa.2017.09.003.
[26]Zhang N,Lou WH,Zhang XB,et al.Vascular complications following prophylactic balloon occlusion of the internal iliac arteries resolved by successful interventional thrombolysis in a patient with morbidly adherent placenta[J].J Zhejiang Univ Sci B,2017,18(3):272-276.doi:10.1631/jzus.B1600315.
[27]Peng Q,Zhang W.Rupture of multiple pseudoaneurysms as a rare complication of common iliac artery balloon occlusion in a patient with placenta accreta:A case report and review of literature[J].Medicine(Baltimore),2018,97(12):e9896.doi:10.1097/MD.0000000000009896.
[28]吴世勇,郭学利,张海容,等.经股动脉下段切开取栓术59例临床分析[J].中国普通外科杂志,2014,23(6):845-848.doi:10.7659/j.issn.1005-6947.2014.06.028.Wu SY,Guo XL,Zhang HR,et al.Embolectomy via incision in lower segment of the femoral artery:clinical analysis of 59 cases[J].Chinese Journal of General Surgery,2014,23(6):845-848.doi:10.7659/j.issn.1005-6947.2014.06.028.
[29]李振振,曾昭凡,肖占祥,等.外周性假性动脉瘤的治疗:附29例报告[J].中国普通外科杂志,2016,25(6):864-868.doi:10.3978/j.issn.1005-6947.2016.06.015.Li ZZ,Zeng ZF,Xiao ZX,et al.Treatment of peripheral arterial pseudoaneurysms:a report of 29 cases[J].Chinese Journal of General Surgery,2016,25(6):864-868.doi:10.3978/j.issn.1005-6947.2016.06.015.
[30]Nieswandt B,Pleines I,Bender M.Platelet adhesion and activation mechanisms in arterial thrombosis and ischaemic stroke[J].J Thromb Haemost,2011,9(Suppl 1):92-104.doi:10.1111/j.1538-7836.2011.04361.x.
[31]McCollough CH,Schueler BA,Atwell TD,et al.Radiation exposure and pregnancy:when should we be concerned?[J].Radiographics,2007,27(4):909-917.doi:10.1148/rg.274065149.
