急性胰腺炎是一种常见的急腹症,具有较高的发病率和病死率。肝门静脉积气(hepatic portal venous gas,HPVG)是急腹症中一种罕见的伴发症[1]。HPVG常见于缺血性肠坏死、机械性肠梗阻、炎症性肠病等疾病,其中缺血性肠坏死发生率最高,而肠缺血常合并严重的脓毒症,短时间内可进展为脓毒性休克导致死亡,但胰腺炎相关性HPVG却罕见相关报道。本文总结了2018年5月—2018年12月收治的2例急性胰腺炎相关性HPVG的患者的临床病例特点,查阅国内外文献,分析讨论该病的临床特征、发病机理及影像学特征、治疗及预后,加强临床医生对该病的认识,现报告如下。
1 临床资料
1.1 病例1
男,65岁,农民,系上腹部疼痛伴纳差10余天于2018年5月26日入院,无胆道结石,高脂血症,结缔组织病等病史,发病前无饮酒及暴饮暴食史。患者2018年5月16日无明显诱因下出现剑突下疼痛,呈持续性隐痛,伴有纳差不适,未予重视治疗,于2018年5月24日症状加重就诊于当地市人民医院,当地CT检查提示急性胰腺炎、胆囊结石伴胆囊炎,给予治疗后患者症状进行性加重并出现呼吸困难,面罩吸氧血氧饱和度维持在85%~95%,复查腹部CT提示腹腔渗液较前增多,2018年5月26日就诊我院,以“急性胆源性胰腺炎”收住普通病房。入院体检:体温37.8℃,心率80次/min,呼吸20次/min,血压138/89 mmHg(1 mmHg= 0.133 kPa),经皮血氧饱和度96%(面罩吸氧)。神清,精神一般,皮肤巩膜无黄染,浅表未及肿大淋巴结,双肺呼吸音粗,可闻及少许哮鸣音,心律齐,未闻及杂音,腹稍胀,上腹部压痛,无反跳痛,肠鸣音不亢,移动性浊音(-),膀胱压14 mmHg。实验室检查:C-反应蛋白331.5 mg/L,白细胞 12.34×109/L,血红蛋白143 g/L,血小板85×109/L,D-二聚体8.43 μg/mL,前降钙素原1.240 ng/mL,pH 7.393,CO2分压37.9 mmHg,氧分压 68.5 mmHg,谷丙转氨酶50 U/L,谷草转氨酶30 U/L,γ-谷氨酰基转移酶92 U/L,总胆红素18.1 μmol/L,葡萄糖7.08 mmol/L,钾离子4.13 mmol/L、钙离子1.97 mmol/L,甘油三酯0.74 mmol/L、淀粉酶229 U/L、白蛋白23.3 g/L。入院后给于吸氧,抗感染,肠内营养支持及通便等治疗后,患者呼吸困难,腹痛症状好转,于2018年6月3日开始半流质饮食。自2018年6月19日患者开始出现腹胀并逐渐加重,予以胃肠减压,较多胃液引出,肠内营养无法进行。2018年6月24日患者精神转差,膀胱压20 mmHg,2018年6月25日复查腹部CT提示HPVG,肝周及盆腔可见游离积液,胰腺内及胰腺周围大量坏死组织包裹(图1),继续予以胃肠减压、抑酸、抑酶、营养支持等综合治疗,2018年6月26夜间突然出现面色苍白、神情呆滞、手脚冰凉,行心电监护血压65/38 mmHg,心率140次/min,血氧饱和度83%;予以高流量吸氧及大量扩容补液后血压逐渐升至90/60 mmHg左右,血氧饱和度恢复至95%左右;去甲肾上腺素静脉泵入维持血压情况下转入重症医学科救治。患者转科后开始出现寒战高热,最高体温39.0℃,复查血降钙素原17.370 ng/mL,给于美罗培南抗感染治疗并行肝周及盆腔穿刺置管引流,引流出淡黄色液体,但患者腹胀未能缓解并出现呼吸衰竭,给于无创通气等治疗未见明显好转,因经济原因于2018年6月29日自动出院,院外随访2018年7月5日死亡。
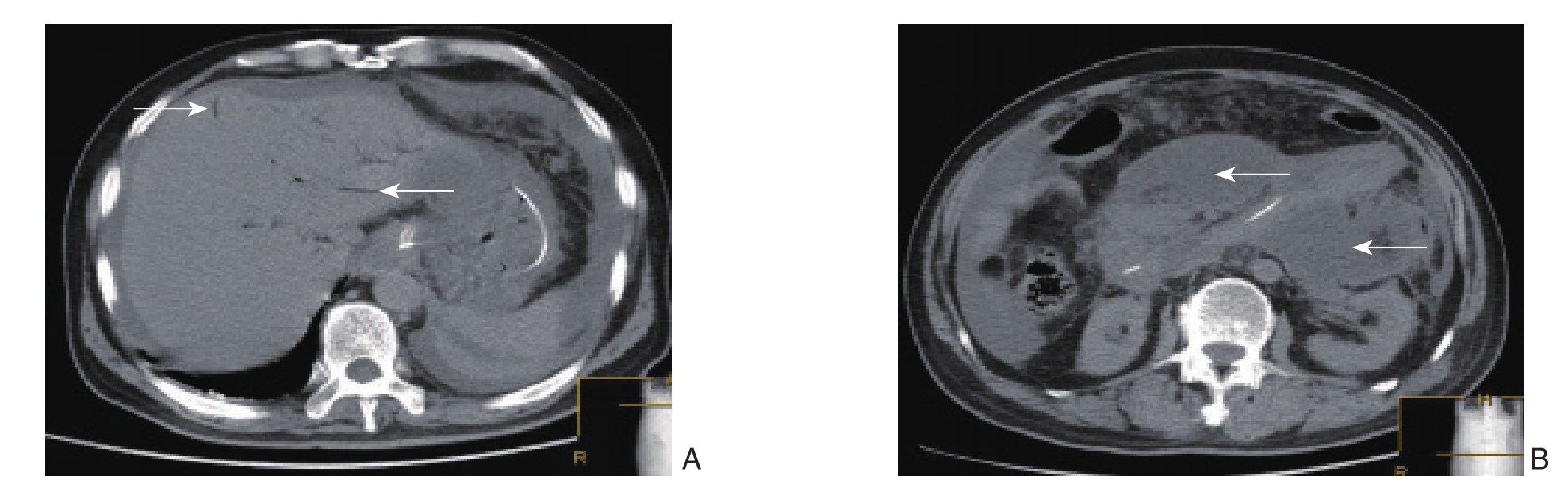
图1 病例1腹部CT资料 A:HPVG(白色箭头);B:胰腺内及胰腺周围大量坏死组织包裹(白色箭头)
Figure1 Abdominal CT findings of case 1 A: HPVG (shown by the white arrows); B: A large amount of walled-off necrotic debris in the pancreas and peripancreatic region (shown by the white arrows)
1.2 病例2
女,70岁,农民,因腹痛1 d于2018年12月25日入院,无胆道结石,高脂血症,结缔组织病病史,发病前无饮酒及暴饮暴食史。患者于2018年12月24日无明显诱因下出现腹痛,为上腹部持续性胀痛,以脐上最为明显,疼痛与体位或活动无关联性,无畏寒发热、胸闷心悸、咳嗽咳痰、腹泻呕吐、呕血黑便等不适,当时自觉疼痛尚能耐受,未行诊治。2018年12月25日自觉症状较前明显加重,至当地医院就诊,上腹部彩超提示胰腺炎可能,遂住院予以相关对症治疗(具体不详),治疗后患者症状改善不明显且出现少尿,遂转入我院进一步诊治。入院急诊CT提示胰腺形态饱满,胰腺周围及腹腔多发渗出及积液,门静脉及胰腺周围多发积气。拟胰腺炎、消化道穿孔可能收住重症医学科(图2)。入院体检:体温36.8℃,心率100次/min,呼吸25次/min,血压90/60 mmHg。神清,精神差,呼吸急促,两肺呼吸音低,心律齐,腹部稍胀,腹肌紧张,全腹可触及压痛及明显反跳痛,未闻及肠鸣音。实验室检查:白细胞计数1.97×109/L,血淀粉酶2840 U/L,脂肪酶6448 U/L,血降钙素原19.650 ng/mL,C-反应蛋白166.2 mg/L。入院诊断急性胰腺炎,急性弥漫性腹膜炎,感染性休克,消化道穿孔?当日急诊在全麻下行腹腔镜探查+中转开腹胰腺被膜切开减压+腹腔引流术,术中腹腔镜探查见腹盆腔黄色脓性液体约300 mL,主要集中在文氏孔,右侧结肠旁沟及盆腔,胆囊未见结石及坏死穿孔,胃,小肠,结肠,回盲部肠管壁暗红色,胰腺被膜水肿,表面覆盖黄色脓苔样皂化斑,中转开腹行胰腺被膜切开减压+腹腔引流术,考虑肠道可能存在缺血情况,但尚未达到坏死,术后补液升压后缺血可能会有所改善,遂未行肠管切除术。术后休克仍难以纠正,出现多脏器功能不全(呼吸循环衰竭、肝衰竭、肾衰竭、消化道衰竭等),给于血液净化等治疗后病情仍进一步加重,2018年12月28患者家属要求自动出院并于当日死亡。
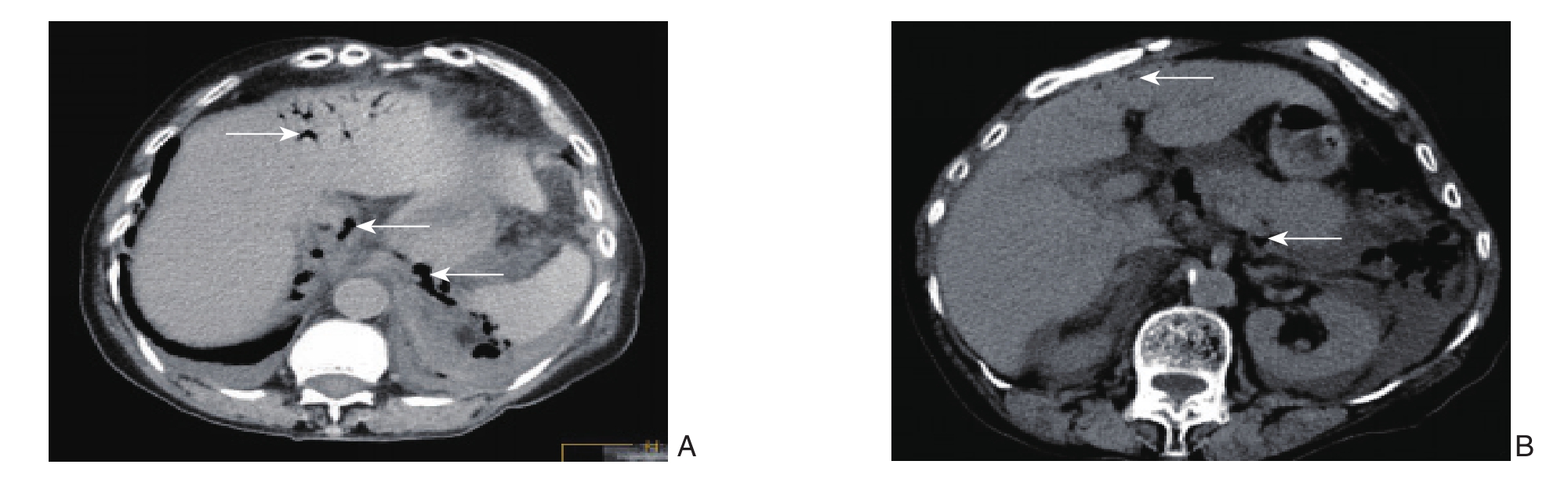
图2 病例2腹部CT资料 A:HPVG(白色箭头);B:腹膜后大量积气(白色箭头)
Figure2 Abdominal CT findings of case 2 A: HPVG (shown by the white arrows); B: Massive gas collections in retroperitoneal space(shown by the white arrows)
2 文献复习与讨论
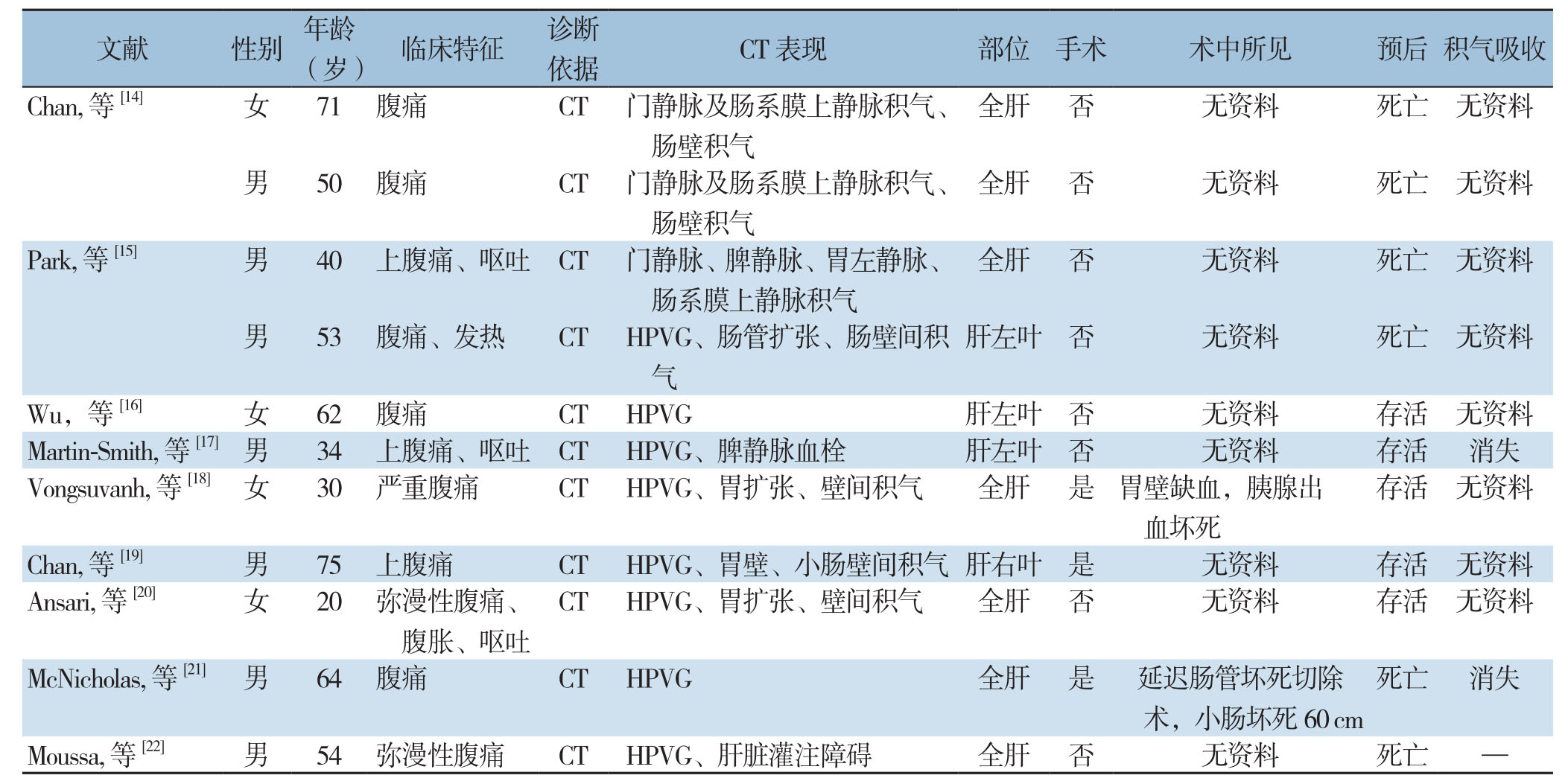
急性胰腺炎是一种常见的急腹症,具有较高的发病率和病死率。胰腺坏死继发感染是胰腺炎的一种局部并发症,病死率可高达30%左右[2-4]。一旦感染且未能有效干预的情况下,病死率甚至可达到100%[5-6]。胰腺炎早期可以出现循环衰竭,肾功能不全等并发症,后期可出现腹膜后感染、出血,消化道穿孔等并发症。HPVG是一种少见的临床征象,具有典型的影像学表现及较高的病死率。1955年Wolfe等[7]首次报道了HPVG在婴儿致命坏死性小肠结肠炎中的作用。随后在1960年Susman等[8]报告了首例成人肠系膜上动脉血栓形成导致HPVG的病例。随后HPVG的临床报道逐渐增多。HPVG不是一种独立的疾病,而是其他疾病在肝脏的一种表现,常见病因为肠缺血坏死、机械性肠梗阻、溃疡性结肠炎和克罗恩病等[9-12]。医源性操作也可以导致HPVG的发生,Suzuki等[13]报道1例结肠镜操作导致的HPVG。在众多病因中,以肠缺血发生率最多见,而肠缺血常合并严重的肠源性脓毒症,短时间内可进展为休克,进而发展为多器官功能不全综合征导致患者死亡。虽然报道各种病因导致HPVG的文献较多,但胰腺炎相关性HPVG在国内罕见报道,国外仅有少量文献[14-22]报道(表1)。关于HPVG在胰腺炎中的发病率目前尚未见相关文献报道。从外文文献中可以看出胰腺炎相关性HPVG的临床主要表现为腹痛,诊断主要依赖B超和CT检查,如果同时具备胰腺炎和HPVG的影像学表现即可以明确诊断。由于超声难以发现HPVG的病因且对超声操作者的技术水平较高,以及CT在诊断HPVG具有高灵敏度的特点,同时CT还可以同时发现肝外门静脉系统及肠壁间积气,而这是B超难以发现的,因此CT在诊断HPVG应用的愈加广泛[23],国外文献对HPVG的诊断也均以CT表现作为标准(表1)。HPVG与肝内胆管积气征象相似,易误诊,两者鉴别要点:⑴ 胆汁的向心方向流动使得胆道积气位于肝脏中心部位,呈分散不连续的气体影;⑵ 肝内门静脉血液离心方的流动使气体多位于肝脏外周、肝被膜2 cm内,呈枯枝状透亮积气影[24-25]。从表1中可以看出胰腺炎相关性HPVG主要位于全肝或左半肝,单独右半肝HPVG少见,具体原因不清。目前,对于HPVG的发病机制仍然不明,目前主要有两种理论:⑴ 机械性:肠腔内压力增高致气体溢入肠系膜静脉并进入门脉系统;⑵ 微生物入侵门静脉后产生气体所致[26]。HPVG在胰腺炎中的潜在发病机制考虑可能与胰酶直接破坏肠壁,或者肠道缺血使气体从肠腔转移到门静脉系统有关[15,27]。本文病例1的HPVG病因可能与胰腺炎后期腹膜后感染导致麻痹性肠梗阻、肠腔内压力增高,从而导致气体进入门脉系统有关;病例2胰腺炎HPVG可能与胰酶直接破坏肠壁有关,但难以完全解释胰腺炎发病1 d即出现腹膜后积气的影像学表现。该者无饮酒、暴饮暴食病史,无高脂血症及高钙血症,IgG4抗体阴性,无系统性红斑狼疮等结缔组织疾病证据,CT及手术未见胆道结石,胰腺炎病因难以明确,发病1 d后即见门静脉及腹膜后积气,不排除存在回盲部炎症导致腹膜后感染,从而导致HPVG和胰腺炎发生的可能。
表1 文献报道的11例急性胰腺炎相关性HPVG患者资料
Table1 Data of 11 patients with HPVG in acute pancreatitis reported by previous literature
 Chan,等[14] 女 71 腹痛 CT 门静脉及肠系膜上静脉积气、肠壁积气全肝 否 无资料 死亡 无资料
Chan,等[14] 女 71 腹痛 CT 门静脉及肠系膜上静脉积气、肠壁积气全肝 否 无资料 死亡 无资料 全肝 否 无资料 死亡 无资料男 50 腹痛 CT 门静脉及肠系膜上静脉积气、肠壁积气Moussa,等[22] 男 54 弥漫性腹痛 CT HPVG、肝脏灌注障碍 全肝 否 无资料 死亡 —
全肝 否 无资料 死亡 无资料男 50 腹痛 CT 门静脉及肠系膜上静脉积气、肠壁积气Moussa,等[22] 男 54 弥漫性腹痛 CT HPVG、肝脏灌注障碍 全肝 否 无资料 死亡 —
急性胰腺炎的治疗趋于保守,已经由过去积极的外科手术转向各种微创引流或清创的方法,大大降低了胰腺炎感染性坏死患者的病死率与并发症发生率[28]。以经皮穿刺置管引流为基础的“升阶梯”治疗策略已成为治疗胰腺坏死继发感染的主流策略[29-30]。国内有多项研究显示,B超或CT引导下的各种穿刺置管引流治疗重症急性胰腺炎继发胰周坏死感染均取得较好的疗效,且并发症发生率低[31]。B超和CT引导下进行经皮穿刺置管引流两种方法各有优缺点。一般只在出现腹腔间室高压综合征、继发消化道穿孔或腹膜后坏死继发感染性休克的情况下才考虑紧急手术[32]。HPVG的治疗应该考虑患者的临床状态及潜在疾病,但它的出现是病情预后较差的一种表现,往往高度提示腹内器官存在缺血坏死,因此多主张急诊手术治疗[33-34]。对于胰腺炎相关性HPVG是否需要或什么时机手术尚无定论。尽管有国外文献[20, 22]报道了胰腺炎相关性HPVG经过保守治疗病情好转的病例,但Chan等[14-15]分别报道了2例胰腺炎相关性HPVG由于未及时手术导致了患者发病后短期内死亡。因此对于胰腺炎相关性HPVG的患者而言,在决定是否手术之前同样需要评估患者的临床状态,胰腺炎的危重程度等情况。本文病例1病程中出现明显的腹胀、腹腔内压力增高、HPVG及感染性休克的临床表现,此时可能已经出现了缺血性肠坏死,如果能够及时行坏死肠管切除手术治疗,有可能会改善预后。病例2术中发现胃、小肠、结肠、回盲部肠管壁暗红色,即均有缺血表现,但考虑到如果全部切除,势必造成术后营养困难,且存在给予液体复苏治疗后肠管未必会发展至肠坏死地步的侥幸心理,故未行肠道坏死切除术,造成术后肠坏死导致病情急剧恶化,循环功能等多器官功能不全难以纠正,最终导致死亡,与此前Piton等[35]报道相符,因此在术中对那些缺血的肠管应该积极切除,避免肠道坏死而加重病情。
回顾分析2例患者的治疗经过,教训及经验总结如下:⑴ 临床医师对HPVG缺乏认识和重视,当CT表现为HPVG时并未引起临床医师的警惕,病例1如果在行CT检查发现HPVG后果断剖腹探查,或可以避免患者死亡。⑵ 临床医师对肠道缺血坏死警惕性不够,存在侥幸心理,如当时难以判断肠管是否坏死,可以给予热敷肠管等方式后观察肠管活力,如不能改善或缺血进一步加重,及时切除缺血坏死肠管,可能患者不至于死亡;⑶ 关于胰腺炎相关性HPVG进腹手术方式的选择,目前鲜有文献提及。对于胰腺炎患者,往往选择上腹部穹窿样切口进腹,而腹腔镜手术并不是一个合适的选择,特别是对于存在HPVG的患者,气腹会造成腹腔内压力的骤然升高,加重腹腔内脏器的缺血并造成腹腔内感染的播散,从而造成病情的进一步恶化。因此如果需要手术,应该采取传统的剖腹方式。
急性胰腺炎中HPVG的出现是一个不良的预后信号,病情复杂,预后较差,病死率高,需要早期发现并积极治疗,必要时急诊手术治疗,尤其是伴有肠系膜缺血患者。
[1]Villa M,Ranade AN,Jaimes-Vanegas N,et al."STOP,LOOK,and LISTEN." Hepatic Portal VenousGas: Time for Clinical Assessment![J].Int J Angiol,2013,22(2):123-126.doi: 10.1055/s-0032 -1333066.
[2]申鼎成,刘志勇,黄耿文,等.电极片定位超声引导下经皮穿刺置管引流治疗感染性胰腺坏死:附61例报告[J].中国普通外科杂志,2017,26(9):1168-1173.doi:10.3978/j.issn.1005-6947.2017.09.014.Shen DC,Liu ZY,Huang GW,et al.Percutaneous catheter drainage under positioning of electrode plates and ultrasound guidance: a report of 61 cases[J].Chinese Journal of General Surgery,2017,26(9):1168-1173.doi:10.3978/j.issn.1005-6947.2017.09.014.
[3]van Santvoort HC,Bakker OJ,Bollen TL,et al.A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome[J].Gastroenterology,2011,141(4):1254-1263.doi:10.1053/j.gastro.2011.06.073.
[4]Raraty MG,Halloran CM,Dodd S,et al.Minimal access retroperitoneal pancreatic necrosectomy: improvement in morbidity and mortality with a less invasive approach[J].Ann Surg,2010,251(5):787-793.doi: 10.1097/SLA.0b013e3181d96c53.
[5]Werner J,Hartwig W,Hackert T,et al.Surgery in the treatment of acute pancreatitis--open pancreatic necrosectomy[J].Scand J Surg,2005,94(2):130-134.doi: 10.1177/145749690509400209.
[6]Petrov MS,Shanbhag S,Chakraborty M,et al.Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis[J].Gastroenterology,2010,139(3):813-820.doi: 10.1053/j.gastro.2010.06.010.
[7]Wolfe JN,Evans WA.Gas in the portal veins of the liver in infants;a roentgenographic demonstration with postmortem anatomical correlation[J].Am J Roentgenol Radium Ther Nucl Med,1955,74(3): 486-488.
[8]Susman N,Senturia HR.Gas embolization of the portal venous system[J].Am J Roentgenol Radium Ther Nucl Med,1960,83:847-850.
[9]Liang HH,Wang W,Hung CS,et al.Branch-type gas in the liver[J].J Emerg Med,2013,44(5):e363-364.doi: 10.1016/j.jemermed.2012.11.029.
[10]Chung H,Lilien LD.Portal venous gas: a clinical finding in obstructed infracardiac total anomalous pulmonary venous connection[J].Pediatr Cardiol,2012,33(4):669-671.doi: 10.1007/s00246-012-0195-x.
[11]Siswojo A,Ihle BU.Hepatic portal venous gas in a patient with intestinal necrosis[J].Emerg Med Austmlas,20l0,22(2):187-188.doi: 10.1111/j.1742-6723.2010.01274.x.
[12]Alqahtani S,Coffin CS,Burak K,et al.Hepatic portal venous gas: a report of two cases and a review of the epidemiology,pathogenesis,diagnosis and approach to management[J].Can J Gastroenterol,2007,21(5):309-313.
[13]Suzuki S,Takeuchi Y,Ishihara R,et al.Hepatic Portal Venous Gas Following Colonic Endoscopic Submucosal Dissection[J].Intern Med,2019,58(5):755-756.doi: 10.2169/internalmedicine.1771-18.
[14]Chan SC,Wan YL,Cheung YC,et al.Computed tomography findings in fatal cases of enormous hepatic portal venous gas[J].World J Gastroenterol,2005,11(19):2953-2935.
[15]Park HC,Lee WS,Joo SY,et al.Hepatic portal venous gas associated with acute pancreatitis: reports of two cases and review of literature[J].Korean J Gastroenterol,2007,50(2):131-135.
[16]Wu JM,Wang MY.Hepatic portal venous gas in necrotizing pancreatitis[J].Dig Surg,2009,26(2):119-120.doi:10.1159/000206147.
[17]Martin-Smith JD,Larkin JO,Hogan JG,et al.Necrotizing pancreatitis presenting with pneumatosis coli and hepatic portal venous gas[J].ANZ J Surg,2011,81(6):467-468.
[18]Vongsuvanh R,Pleass H,van der Poorten D.Acute necrotizing pancreatitis,gastric ischemia,and portal venous gas complicating intragastric balloon placement[J].Endoscopy,2012,44(Suppl 2 UCTN):E383-384.doi: 10.1055/s-0032-1310146.
[19]Chan AC,Poon RT.Portal venous gas and pneumatosis intestinalis in necrotizing pancreatitis[J].Clin Gastroenterol Hepatol,2014,12(7):e57-58.doi: 10.1016/j.cgh.2013.10.010.
[20]Ansari MM,Mushtaq N,Pateria V,et al.Gas in Hepatic Portal Veins with Gastric Massive Dilatation and Pneumatosis in Acute Pancreatitis[J].J Clin Diagn Res,2015,9(10):PD05-7.doi:10.7860/JCDR/2015/11941.6634.
[21]McNicholas DP,Kelly ME,Das JP,et al.Disappearing portal venous gas in acute pancreatitis and small bowel ischemia[J].Radiol Case Rep,2017,12(2):269-272.doi: 10.1016/j.radcr.2017.01.006.
[22]Moussa M,Marzouk I,Abdelmoula K,et al.Role of Computed tomography in predicting prognosis of Hepatic portal venous gas[J].Int J Surg Case Rep,2017,30:177-182.doi: 10.1016/j.ijscr.2016.11.055.
[23]史逸华,戴灵波,肖德双,等.腹腔间隔室综合征伴肝门静脉积气[J].中华普通外科杂志,2018,33(11):960-961.doi:10.3760/cma.j.issn.1007-631X.2018.11.019.Shi YH,Dai LB,Xiao DQ,et al.Abdominal compartment syndrome accompanied with Hepatic portal venous gas[J].Zhong Hua Pu Tong Wai Ke Za Zhi,2018,33(11):960-961.doi:10.3760/cma.j.issn.1007-631X.2018.11.019.
[24]姚敏学,冯秋鹏,鲍磊,等.门静脉积气一例[J].中华急诊医学杂志,2016,25(3):355.doi:10.3760/cma.j.issn.1671-0282.2016.03.020.Yao MX,Feng QP,Bao L,et al.One case report of portal venous gas[J].Chinese Journal of Emergency Medicine,2016,25(3):355.doi:10.3760/cma.j.issn.1671-0282.2016.03.020.
[25]汪登亮,康权,彭飞,等.食管破裂致不典型肝门静脉积气一例[J].中华普通外科杂志,2018,33(4):344-345.doi:10.3760/cma.j.issn.1007-631X.2018.04.022.Wang DL,Kang Q,Peng F,et al.Hepatic portal venous gas caused by esophageal rupture: a report of one case[J].Zhong Hua Pu Tong Wai Ke Za Zhi,2018,33(4):344-345.doi:10.3760/cma.j.issn.1007-631X.2018.04.022.
[26]Abboud B,El Hachem J,Yazbeck T,et al.Hepatic ponal Venous gas:physiopathology,etiology,prognosis and treatment[J].World J Gastroenterol,2009,15(29):3585-3590.
[27]Liebman PR,Patten MT,Mann J,et al.Hepatic--portal venous gas in adults: etiology,pathophysiology and clinical significance[J].Ann Surg,1978,187(3):281-287.
[28]宁彩虹,黄耿文,申鼎成,等.真菌感染性胰腺坏死的临床分析:附46例报告[J].中国普通外科杂志,2018,27(9):1155-1159.doi:10.7659/j.issn.1005-6947.2018.09.011.Ning CH,Huang GW,Shen DC,et al.Clinical analysis of fungal infected pancreatic necrosis:a report of 46 cases[J].Chinese Journal of General Surgery,2018,27(9):1155-1159.doi:10.7659/j.issn.1005-6947.2018.09.011.
[29]申鼎成,周书毅,黄耿文,等.多重耐药菌感染的包裹性胰腺坏死的外科治疗策略[J].中国普通外科杂志,2016,25(9):1319-133.doi:10.3978/j.issn.1005-6947.2016.09.016.Shen DC,Zhou SY,Huang GW,et al.Surgical treatment strategies for wall-off pancreatic necrosis with multi-drug resistant organism infections[J].Chinese Journal of General Surgery,2016,25(9):1319-133.doi:10.3978/j.issn.1005-6947.2016.09.016.
[30]刘国华,戴东,谭小宇,等.循PCD引流管路径微小切口联合经皮肾镜治疗重症急性胰腺炎感染性坏死[J].中国普通外科杂志,2018,27(3):335-342.doi:10.3978/j.issn.1005-6947.2018.03.011.Liu GH,Dai D,Tan XY,et al.Small incision along the PCD tube tract combined with percutaneous nephroscope in treatment of severe acute pancreatitis complicated with infected necrosis[J].Chinese Journal of General Surgery,2018,27(3):335-342.doi:10.3978/j.issn.1005-6947.2018.03.011.
[31]阿不都热依木·阿不都拉,买买提吐尔逊·吐尔迪,伊斯马依力·艾麦提,等.超声引导下经皮穿刺置管引流术治疗重症胰腺炎合并胰周脓肿[J].中国普通外科杂志,2017,26(3):390-395.doi:10.3978/j.issn.1005-6947.2017.03.019.Abudoureyimu·ABDL,Maimaitituerxun·TRD,Yisimayili·AMT,Ultrasound-guided percutaneus catheter drainage in treatment of severe acute pancreatitis complicated with peripancreatic abscess[J].Chinese Journal of General Surgery,2017,26(3):390-395.doi:10.3978/j.issn.1005-6947.2017.03.019.
[32]Rau B,Pralle U,Uhl W,et al.Management of sterile necrosis in instances of severe acute pancreatitis[J].J Am Coll Surg,1995,181(4):279-288.
[33]毛敏杰,许振琦,汪彩红,等.急性缺血性结肠炎致门静脉积气一例报道[J].中华危重症医学杂志:电子版,2014,7(3):218-219.doi:10.3877/cma.j.issn.1674-6880.2014.03.016.Mao MJ,Xu ZQ,Wang CH,et al.Portal venous gas caused by acute ischemic colitis: a report of one case[J].Chinese Journal of Critical Care Medicine: Electronic Edition,2014,7(3):218-219.doi:10.3877/cma.j.issn.1674-6880.2014.03.016.
[34]Nelson AL,Millington TM,Sahani D,et al.Hepatic portal Venous gas: the ABCs of management[J].Arch Surg,2009,144(6):575-581.doi: 10.1001/archsurg.2009.88.
[35]Piton G,Capellier G,Delabrousse E.Echography of the portal vein in a patient with shock[J].Crit Care Med,2016,44(6):e443-445.doi: 10.1097/CCM.0000000000001476.
