下肢深静脉血栓(deep venous thrombosis,DVT)是下肢深静脉血液凝结引起回流受阻所致的血管性疾病,发生率为20%~40%[1],其引起的肺栓塞严重危及患者生命。置管溶栓(catheterdirected thrombolysis,CDT)是有效清除DVT的首选方法,但对于合并髂静脉压迫综合征(Cokett综合征)的患者,单独的CDT、抗凝治疗疗效欠佳[2]。Cokett综合征是左侧髂总静脉受右侧髂总动脉和腰骶椎的双重压迫引起的临床症状,是引起DVT复发的重要诱因,因此,对合并Cokett综合征的DVT患者,除了清除DVT外,必须同时解除髂静脉受到的压迫及其引起的闭塞和狭窄[3]。支架植入能够有效改善髂静脉的闭塞和狭窄,但其通过异物刺激、局部血流动力学变化和炎症因子引起血管损伤,导致血管内膜过度增生,是支架内再狭窄主要机制之一[4]。本研究观察CDT联合支架植入治疗Cockett综合征伴DVT患者近远期疗效及其对血管损伤程度的影响,分析血管损伤程度与远期疗效的相关性,为CDT联合支架植入的临床使用提供理论依据。
1 资料与方法
1.1 一般资料
选择盐城市第一人民医院血管外科于2013年1月—2015年1月收治的90例Cockett综合征伴DVT患者,年龄22~60岁,病程3~14 d,其中,左下肢DVT 71例,右下肢19例;临床表现为下肢疼痛、肿胀、活动受限,皮肤张力高。依据随机数字表法分为观察组和对照组,各45例。⑴ 观察组:男21例,女24例;年龄(40.5±6.7)岁;病程(8.6±0.8)d;血栓长度(5.5±1.2)mm,中央型24例,混合型21例;发病诱因长期卧床12例,妇科手术或分娩14例,肿瘤7例,下肢外伤7例,不明原因5例;均采用CDT联合支架治疗;⑵ 对照组:男22例,女23例;年龄(40.9±6.9)岁;病程(8.5±0.9)d;血栓长度(5.4±1.1)mm,中央型26例,混合型19例;发病诱因长期卧床 10例,妇科手术或分娩15例,肿瘤8例,下肢外伤 8例,不明原因4例,均采用CDT治疗。两组患者基本资料比较无统计学差异(均P>0.05),具有可比性。
1.2 纳入排除标准
纳入标准:⑴ 经下肢深静脉造影检查或血管彩色多普勒超声确诊;⑵ 血浆D-二聚体不得低于500 ng/mL;⑶ 初次发病;⑷ 无溶栓禁忌证;⑸ 具备经济能力,能够承担治疗费用;⑹ 病程≤14 d;⑺ 自愿参与本研究,并签署知情同意书。排除标准:⑴ 晚期肿瘤,预计生存期<6个月;⑵ 严重肾功能障碍,肌酐清除率<30 mL/min;⑶ 已经手术或药物治疗者;⑷ 无法按时复查,配合随访者;⑸ 孕妇或妊娠期妇女;⑹ 合并感染性疾病。本研究获得我院伦理委员会批准。
1.3 治疗方法
观察组采用CDT联合支架治疗,对照组采用单独的CDT治疗。抗凝治疗:所有患者确诊后,即刻皮下注射100 U/kg低分子量肝素,每12 h注射一次,直至CDT治疗。下腔静脉滤器植入:有患者均常规植入可回收滤器,观察组植入COOK滤器31枚,先健滤器14枚,对照组植入COOK滤器33枚,先健滤器12枚;仰卧位,常规消毒、铺巾,患肢对侧腹股沟局部麻醉,Seldinger穿刺,植入5 F导管鞘,下腔静脉造影,确定肾静脉开口和下腔静脉无血栓、阻塞后,在最低一侧肾静脉开口下0.5~1 cm处植入下腔静脉滤器,造影显示位置良好后,拔出鞘管,压迫止血。CDT:植入下腔静脉滤器后,俯卧位,暴露患肢下肢腘窝。常规消毒、铺巾,彩色多普勒超声定位腘静脉,Seldinger穿刺,植入5 F导管鞘,明确血栓范围。植入4 F Unifuse溶栓导管,固定。患者返回病房,每日经导管持续泵入60~80万U尿激酶,经鞘管泵入肝素,肝素用量依据每日凝血试验调整,保证APTT在1.5~2.5倍。常规检测血色素、纤维蛋白原,对于有出血倾向患者,次日造影检查。所有患者经CDT治疗5~7 d,拔除鞘管及溶栓导管,压迫止血。支架植入:观察组CDT治疗结束后次日,仰卧位,常规消毒、铺巾,患肢腹股沟区局部麻醉。Seldinger穿刺,植入导丝、导管,造影确定压迫或狭窄的位置,采用10~12 mm球囊扩张,植入Z形自膨式支架(直径14 mm,厂家:沈阳永通医疗器械有限公司)。造影确保支架扩张完全,手术完毕,拔除鞘管,压迫止血。术后处理:所有患者术后口服华法林,口服剂量依据凝血检查中国际化标准比值调整,维持改值在2.0~3.0,对照组口服3个月以上,观察组口服6个月以上,在血浆D-二聚体低于500 ng/mL,造影显示血栓无进展时,拆除下降静脉滤器。
1.4 评价指标
术后疗效评价:手术结束后次日,评估患者疗效,分为治愈(髂静脉血流通常,无残余狭窄,临床症状完全消失)、好转(髂静脉血流通常,无残余狭窄,临床症状减轻,血栓大部分吸收,肢体轻微肿胀)和无效(大量血栓存在,管腔狭窄>50%或完全闭塞,临床无变化或加重),计算总有效率=(治愈+好转)/总例数×100%。随访指标:两组患者随访3年,术后1、2、3年定期随访,经彩色多普勒超声检查,计算再阻塞发生情况,计算一次通畅率和二次通畅率以及末次随访的Villalta评分[5]、静脉临床严重程度评分(venous clinical severity score,VCSS)[6]、生活质量调查表(chronic venous insufficiency questionnaire,CIVIQ)[7]评分,其中Villalta、VCSS评分越高,患者症状越重;CIVIQ评分越高,症状越轻,生活质量越好。一次通畅是指随访一段时间内未出现下腔静脉狭窄,二次通畅是指再阻塞发生后经手术干预后一段时间内未出现下腔静脉狭窄,再阻塞是指管腔狭窄>30%或超声显示下腔静脉内无血流或血液倒流。血管损伤程度评分及炎症因子测定:手术前后,彩多普勒超声检查,参照武国良制定的下肢深静脉评分系统[8],分别从二维及加压、CDFI、B-Flow、PWD4项进行测定血管损伤程度评分,每项0~2分,总分0~8分,分值越高,血管损伤程度越高。血管损伤程度评分由2名超声科医生独立评分,取平均值。并于手术前后取空腹肘静脉血,3 000 r/min离心10 min,取上清液,采用ELISA检测血清TNF-α和IL-10水平。记录手术及随访期并发症。
1.5 统计学处理
本研究的数据分析采用SPSS 19.0进行,计数资料以率表示,采用χ2检验比较,计量资料以均数±标准差( ±s)表示,采用t检验比较,等级资料采用秩和检验,统计结果以P<0.05为差异有统计学意义。
±s)表示,采用t检验比较,等级资料采用秩和检验,统计结果以P<0.05为差异有统计学意义。
2 结 果
2.1 两组患者术后疗效比较
两组患者治疗过程顺利,无术中死亡病例,观察组支架植入定位准确,能够完全覆盖狭窄段和残余血栓。两组患者治疗总有效率均为100%,术后疗效经秩和检验比较,差异无统计学意义(H=0.518,P=0.604)(表1)。
表1 两组患者术后疗效比较[n=45,n(%)]
Table 1 Comparison of postoperative clinical efficacy between the two groups [n=45, n (%)]
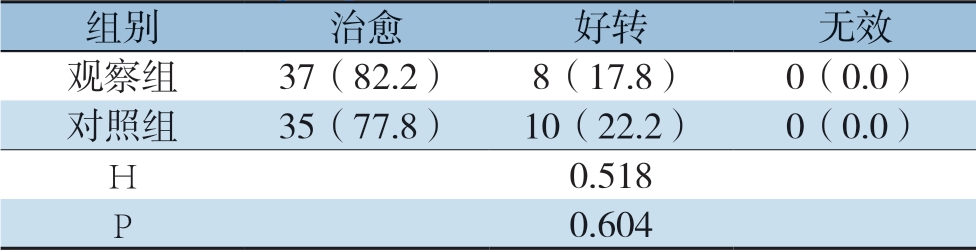
组别治愈好转无效观察组37(82.2)8(17.8)0(0.0)对照组35(77.8)10(22.2)0(0.0)H 0.518 P 0.604
2.2 随访结果
两组患者均随访36~40个月,观察组(37.8±0.4)个月,对照组(38.1±0.5)个月,无失访病例。随访期间,无支架断裂、移位、塌陷、解体或穿破血管现象。随访期间,两组患者均有再阻塞情况发生,经二次治疗后保持通畅。观察组患者随访期再阻塞率明显低于对照组,而术后1、2年及整个随访期的一次通畅率明显高于对照组(均P<0.05),两组组间二次通畅率差异无统计学意义(均P>0.05)(表2)。
2.3 两组患者末次随访各项评分比较
观察组患者末次随访Villalta评分、VCSS评分明显低于对照组,而CIVIQ评分明显高于对照组(均P<0.05)(表3)。
表2 两组患者下腔静脉通畅情况比较[n=45,n(%)]
Table 2 Comparison of inferior vena cava patency between the two groups [n=45, n (%)]
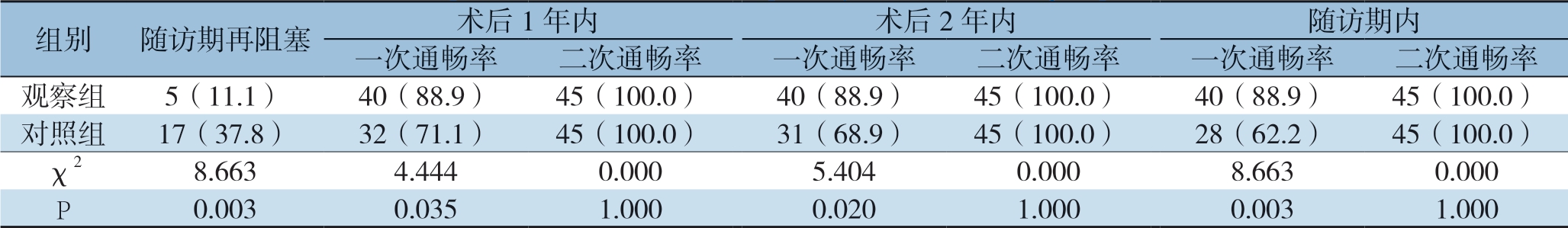
组别随访期再阻塞术后1年内术后2年内随访期内一次通畅率二次通畅率一次通畅率二次通畅率一次通畅率二次通畅率观察组5(11.1)40(88.9)45(100.0)40(88.9)45(100.0)40(88.9)45(100.0)对照组17(37.8)32(71.1)45(100.0)31(68.9)45(100.0)28(62.2)45(100.0)χ28.6634.4440.0005.4040.0008.6630.000 P0.0030.0351.0000.0201.0000.0031.000
表3 两组患者末次随访各项评分比较(n=45, ±s)
±s)
Table 3 Comparison of the studied scores at the last follow-up between two groups (n=45,  ±s)
±s)
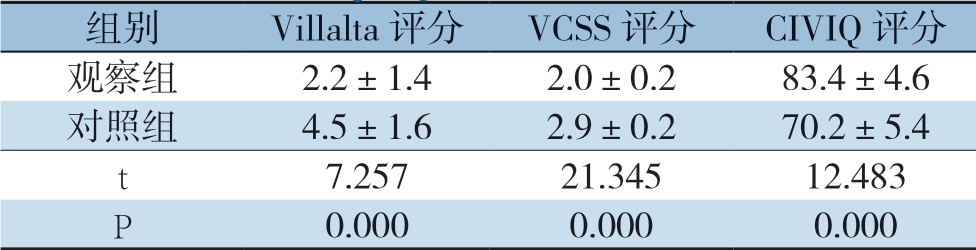
组别Villalta评分VCSS评分CIVIQ评分观察组2.2±1.42.0±0.283.4±4.6对照组4.5±1.62.9±0.270.2±5.4 t 7.25721.34512.483 P 0.0000.0000.000
2.4 两组患者血管损伤程度评分及血清炎症因子水平比较
两组患者术后血管损伤程度评分、血清TNF-α、IL-10水平较术前明显升高(均P<0.05),观察组术后血管损伤程度评分、血清TNF-α、IL-10水平明显高于对照组(均P<0.05)(表4)。
表4 两组患者血管损伤程度评分及血清炎症因子水平比较(n=45, ±s)
±s)
Table 4 Comparison of vascular injury score and serum inflammatory factor levels between two groups (n=45,  ±s)
±s)
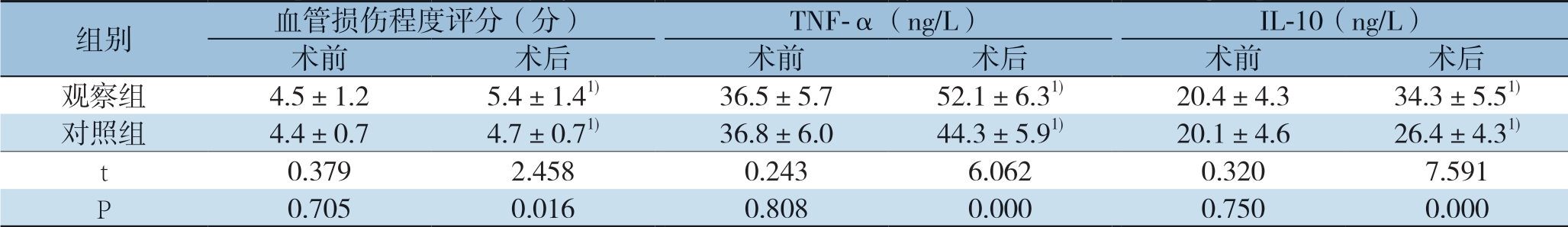
注:1)与术前比较,P<0.05
Note: 1) P<0.05 vs. preoperative value
组别血管损伤程度评分(分)TNF-α(ng/L)IL-10(ng/L)术前术后术前术后术前术后观察组4.5±1.25.4±1.41)36.5±5.752.1±6.31)20.4±4.334.3±5.51)对照组4.4±0.74.7±0.71)36.8±6.044.3±5.91)20.1±4.626.4±4.31)t 0.3792.4580.2436.0620.3207.591 P 0.7050.0160.8080.0000.7500.000
2.5 再阻塞与无再阻塞患者术后血管损伤程度评分及血清炎症因子水平比较
观察组再阻塞患者血管损伤程度评分、血清TNF-α、IL-10水平明显高于无再阻塞患者(P<0.05),对照组再阻塞与无再阻塞患者血管损伤程度评分、血清TNF-α、IL-10水平差异无统计学意义(均P>0.05)(表5)。
表5 再阻塞与无再阻塞患者术后血管损伤程度评分及血清炎症因子水平比较(n=45, ±s)
±s)
Table 5 Comparison of postoperative vascular injury score and serum inflammatory factor levels between patients with and without re-occlusion (n=45,  ±s)
±s)
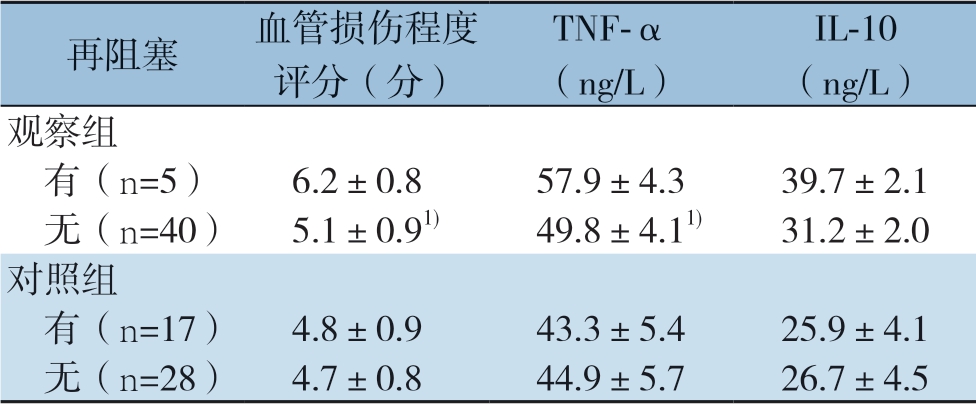
注:1)与同组再阻塞患者比较,P<0.05
Note: 1) P<0.05 vs. patients with re-occlusion in the same group
再阻塞血管损伤程度评分(分)TNF-α(ng/L)IL-10(ng/L)观察组 有(n=5)6.2±0.857.9±4.339.7±2.1 无(n=40)5.1±0.91)49.8±4.11)31.2±2.0对照组 有(n=17)4.8±0.943.3±5.425.9±4.1 无(n=28)4.7±0.844.9±5.726.7±4.5
2.6 安全性比较
治疗及随访期内,观察组出现1例血尿,1例穿刺点渗血,2例皮下瘀斑,1例牙龈出血,不良反应率11.1%;对照组出现1例血尿,1例阴道出血,1例皮下瘀斑,不良反应率6.7%,两组间不良反应率差异无统计学意义(χ2=0.549,P=0.459)。
3 讨 论
目前,CDT治疗DVT疗效已获得血管外科界的公认[9],能够改善深静脉通畅程度、减少血栓综合征的发生以及DVT复发,但对伴Cockett综合征的DVT患者疗效欠佳。对于该类患者,单独的CDT治疗2年内血栓复发率为47%~73%,但采用介入手术干预,血栓复发率可降低至17%~39%[10-11]。支架植入是CDT术后干预的重要手段,对降低血栓复发有利,但植入支架极易诱发新的血栓生成[12]。因此,对于伴Cockett综合征的DVT患者是否进一步进行支架植入治疗,目前尚存争议。本研究观察CDT联合支架植入对伴Cockett综合征的DVT患者血管损伤的影响及近远期疗效,为CDT联合支架植入治疗伴Cockett综合征的DVT提供理论依据。
71.7 %~100%的DVT患者伴有髂静脉压迫,是DVT发生的第四因素[13]。处理髂静脉压迫是伴Cockett综合征的DVT治疗的关键,而单独的CDT并不能纠正髂静脉压迫,且髂静脉病变远心端侧支循环丰富,病变部位有慢性血栓,腔外有解剖压迫,故单独的CDT治疗疗效有限[14-15]。支架植入通过支架对阻塞段血管的有效支撑,与髂静脉压迫平衡,维持该段血管通畅,从而治疗伴Cockett综合征的DVT[16]。据报道[17],溶栓术后支架植入的伴Cockett综合征的DVT患者,术后1年的深静脉通畅率较单独的溶栓术由29.6%提高至87.5%,支架植入已成为血栓通溶解后的重要辅助手段,能够显著提高急性DVT的痊愈率。本研究中,两组患者术后疗效差异无统计学意义,但观察组随访3年的在阻塞率低于对照组,一次通畅率高于对照组,且末次随访的Villalta评分、VCSS评分、CIVIQ评分优于对照组,表明CDT联合支架植入的近期疗效与单独的CDT一致,但远期疗效更为理想,在提高通畅率,减少复发,改善临床症状及生活质量方面优势明显。这是因为CDT能够溶解血栓[2],支架植入能够及时缓解静脉高压,恢复血流[19],两者联用协同互补,从而提高了临床效果。
尽管支架植入能够矫正髂静脉压迫,改善压迫带来的下肢静脉功能不全症状,但其引起的异物刺激、血流动力学变化及血管内膜增生等严重限制了在伴Cockett综合征的DVT患者中的应用[19-20]。多数学者[21-22]认为,支架植入极容易引起新的血栓形成,这时需要再原有支架上套新的支架,导致病变节段长度增加,手术难度增大,远期疗效渐差。数据[17]显示,支架植入引起新的血栓形成与血管损伤和炎症反应相关。TNF-α、IL-10是与深静脉血栓血管损伤程度有关的炎症因子,本文发现两组患者术后血管损伤程度评分、血清TNF-α、IL-10水平较术前显著升高,组间比较差异具有统计学意义,表明支架植入会刺激血管内膜释放炎症因子,加重血管内皮损伤,并通过炎症信号通路促进血栓生成[23]。进一步比较再阻塞和无再阻塞患者血管损伤程度评分、血清TNF-α、IL-10水平,发现观察组再阻塞患者高于无再阻塞患者,对照组再阻塞与无再阻塞患者之间差异无统计学意义,表明CDT联合支架植入后发生再阻塞与支架植入引起的血管损伤有关,但单独的CDT治疗后再阻塞与血管损伤关系不大,髂静脉压迫可能是再阻塞的重要原因[24]。因此,对于伴Cockett综合征的DVT患者,支架植入是必要的,但应监测患者术后血管损伤程度,对于血管损伤程度严重者,应给予药物治疗预防DVT的复发。
总之,CDT联合髂静脉支架植入治疗Cockett综合征伴DVT近期疗效与单独的CDT一致,但远期疗效优于单独的CDT,随访期再阻塞率低,一次通畅率高。CDT联合支架植入治疗后发生再阻塞,可能与支架植入刺激炎症因子释放和导致血管损伤有关。
[1]Shi WY, Gu JP, Liu CJ, et al. Endovascular treatment for iliac vein compression syndrome with or without lower extremity deep vein thrombosis: A retrospective study on mid-term in-stent patency from a single center[J]. Eur J Radiol, 2016, 85(1):7-14. doi: 10.1016/j.ejrad.2015.10.021.
[2]Haig Y, Enden T, Grøtta O, et al. Post-thrombotic syndrome after catheter-directed thrombolysis for deep vein thrombosis (CaVenT): 5-year follow-up results of an open-label, randomised controlled trial[J]. Lancet Haematol, 2016, 3(2):e64-71. doi: 10.1016/S2352-3026(15)00248-3.
[3]Xue GH, Huang XZ, Ye M, et al. Catheter-directed thrombolysis and stenting in the treatment of iliac vein compression syndrome with acute iliofemoral deep vein thrombosis: outcome and follow-up[J]. Ann Vasc Surg, 2014, 28(4):957-963. doi: 10.1016/j.avsg.2013.11.012.
[4]Cui YF, Fu YF, Liu HT, et al. Combined catheter-directed thrombolysis and iliac vein recanalization for iliac vein compression syndrome with secondary acute deep vein thrombosis: effectiveness and long-term outcome[J]. Int Angiol, 2016, 35(1):40-46.
[5]Vedantham S, Goldhaber SZ, Julian JA, et al. Pharmacomechanical Catheter-Directed Thrombolysis for Deep-Vein Thrombosis[J]. N Engl J Med, 2017, 377(23):2240-2252. doi: 10.1056/NEJMoa1615066.
[6]Gagne P, Khoury T, Zadeh BJ, et al. A Multicenter, Retrospective Study of the Effectiveness of the Trellis-8 System in the Treatment of Proximal Lower-Extremity Deep Vein Thrombosis[J]. Ann Vasc Surg, 2015, 29(8):1633-1641. doi: 10.1016/j.avsg.2015.05.029.
[7]Ghanima W, Wik HS, Tavoly M, et al. Late consequences of venous thromboembolism: Measuring quality of life after deep vein thrombosis and pulmonary embolism[J]. Thromb Res, 2018, 164:170-176. doi: 10.1016/j.thromres.2017.07.025.
[8]黄荣, 李梦帆, 黄毅. 深静脉血栓患者血清炎症因子水平与血管损伤程度的关系[J]. 山东医药, 2016, 56(44):58-60. doi:10.3969/j.issn.1002-266X.2016.44.020.Huang R, Li MF, Huang Y. Relationship between serum levels of inflammatory factors and severity of vascular injury in patients with deep vein thrombosis[J]. Shandong Medical Journal, 2016, 56(44):58-60. doi:10.3969/j.issn.1002-266X.2016.44.020.
[9]刘飒华, 肖占祥, 戚悠飞, 等. DSA引导下胫后/胫前静脉穿刺置管碎栓/溶栓治疗急性下肢深静脉血栓形成[J]. 中国普通外科杂志, 2017, 26(6):758-763. doi:10.3978/j.issn.1005-6947.2017.06.014.Liu SH, Xiao ZX, Qi YF, et al. DSA-guided posterior/anterior tibial vein puncture and catheter-directed clot fragmentation/thrombolysis for acute lower extremity deep venous thrombosis[J]. Chinese Journal of General Surgery, 2017, 26(6):758-763. doi:10.3978/j.issn.1005-6947.2017.06.014.
[10]朱杰昌, 张益伟, 冯舟, 等. 减容治疗在左侧下肢深静脉血栓形成合并Cockett综合征治疗中的应用价值[J]. 血管与腔内血管外科杂志, 2016, 2(5):365-369. doi:10.19418/j.cnki.issn2096-0646.2016.05.03.Zhu JC, Zhang YW, Feng Z, et al. Value of Debulking treatment for iliac vein compression syndrome with secondary acute deep venous thrombosis[J]. Journal of Vascular and Endovascular Surgery, 2016, 2(5):365-369. doi:10.19418/j.cnki.issn2096-0646.2016.05.03.
[11]Park JY, Ahn JH, Jeon YS, et al. Iliac vein stenting as a durable option for residual stenosis after catheter-directed thrombolysis and angioplasty of iliofemoral deep vein thrombosis secondary to May-Thurner syndrome[J]. Phlebology, 2014, 29(7):461-470. doi: 10.1177/0268355513491724.
[12]Kakefuda Y, Sato A, Watabe H, et al. Efficacy of Endeavor zotarolimus-eluting stent implantation for the treatment of very late stent thrombosis with late-acquired incomplete stent apposition after sirolimus-eluting stent implantation[J]. Heart Vessels, 2016, 31(7):1196-1199. doi: 10.1007/s00380-015-0720-y.
[13]Choi JW, Jae HJ, Kim HC, et al. CT venography for deep venous thrombosis: Can it predict catheter-directed thrombolysis prognosis in patients with iliac vein compression syndrome?[J]. Int J Cardiovasc Imaging, 2015, 31(2):417-426. doi: 10.1007/s10554-014-0546-1.
[14]Hage AN, Srinivasa RN, Abramowitz SD, et al. Management and treatment of iliocaval thrombosis using endovascular recanalization, stenting, and reconstruction: What all practitioners should know[J]. J Radiol Nur, 2017, 36(4):218-223. doi: doi.org/10.1016/j.jradnu.2017.09.001.
[15]Engelberger RP, Stuck A, Spirk D, et al. Ultrasound-assisted versus conventional catheter-directed thrombolysis for acute iliofemoral deep vein thrombosis: 1-year follow-up data of a randomizedcontrolled trial[J]. J Thromb Haemost, 2017, 15(7):1351-1360. doi: 10.1111/jth.13709.
[16]Jayaraj A, Crim W, Knight A, et al. Characteristics and outcomes of stent occlusion after iliocaval stenting[J]. J Vasc Surg Venous Lymphat Disord, 2019, 7(1):56-64. doi: 10.1016/j.jvsv.2018.07.013.
[17]Ming ZB, Li WD, Yuan RF, et al. Effectiveness of catheter directed thrombolysis and stent implantation on iliofemoral vein thrombosis caused by iliac vein compression[J]. J Thromb Thrombolysis, 2017, 44(2):254-260. doi: 10.1007/s11239-017-1515-z.
[18]Konishi A, Iwasaki M, Shinke T, et al. Lower on-treatment platelet reactivity during everolimus-eluting stent implantation contributes to the resolution of post-procedural intra-stent thrombus: serial OCT observation in the PRASFIT-Elective study[J]. Heart Vessels, 2018, 33(12):1423-1433. doi: 10.1007/s00380-018-1195-4.
[19]Saydam O, Atay M, Seren M, et al. Endovascular treatment of acute deep venous thrombosis secondary to may-thurner syndrome[J]. J Turgut Ozal Med Cent, 2016, 23(3):320-323. doi: 10.5455/jtomc.2016.01.010.
[20]Zhu QH, Zhou CY, Chen Y, et al. Percutaneous manual aspiration thrombectomy followed by stenting for iliac vein compression syndrome with secondary acute isolated iliofemoral deep vein thrombosis: a prospective study of single-session endovascular protocol[J]. Eur J Vasc Endovasc Surg, 2014, 47(1):68-74. doi: 10.1016/j.ejvs.2013.09.030.
[21]Yamamoto Y, Ino Y, Kubo T, et al. TCTAP C-234 Very Late Stent Thrombosis Caused by Obvious Very Late Acquired Stent Malapposition Assessed by Optical Coherence Tomography After Everolimus-eluting Stent Implantation into Sirolimus-eluting Stent[J]. J Am Coll Cardiol, 2016, 67(16S):387-388. doi: 10.1016/j.jacc.2016.03.450.
[22]Matsuda A, Yamada N, Ogihara Y, et al. Early and long-term outcomes of venous stent implantation for iliac venous stenosis after catheter-directed thrombolysis for acute deep vein thrombosis[J]. Circ J, 2014, 78(5):1234-1239.
[23]Nabeta T, Hashikata T, Tojo T, et al. Localized Inflammation and Aneurysm Formation 10 Years After Sirolimus-Eluting Stent Implantation[J]. Circ J, 2017, 81(7):1054-1055. doi: 10.1253/circj.CJ-16-1064.
[24]Nakata T, Fujii K, Fukunaga M, et al. Morphological, Functional, and Biological Vascular Healing Response 6 Months After Drug-Eluting Stent Implantation: A Randomized Comparison of Three Drug-Eluting Stents [J]. Catheter Cardiovasc Interv, 2016, 88(3):350-357. doi: 10.1002/ccd.26273.
