急性下肢动脉血栓形成是血管外科常见的急重症之一。临床主要表现为皮肤苍白或紫绀,脉搏消失、肢体疼痛以及感觉和运动障碍。一旦发病,若无法得到及时有效的诊治,预后通常较差,致残率和病死率高[1-2]。急性下肢动脉血栓形成是急性下肢缺血的重要原因之一[3],降低截肢率和病死率仍是当前临床面临的主要问题[4],随着腔内技术的发展,急性下肢动脉血栓的治疗包括传统开放手术取栓以及腔内介入治疗。置管溶栓(CDT)作为血栓清除的经典介入方法普遍应用于国内各大血管外科中心,但却存在围手术期并发症多、需要多次介入手术从而延长了患者住院时间等缺陷。近年来随着介入器械的发展,采用机械吸栓(PMT)治疗下肢动脉血栓也在部分医院顺利开展。本研究对比两种腔内介入方法治疗下肢动脉血栓的临床疗效,现报告如下。
1 资料与方法
1.1 临床资料
选取2015年7月—2018年3月因急性下肢动脉血栓形成在我院接受介入治疗的67例患者。术前患者下肢缺血严重程度按卢瑟福血管外科学分级均为II级以下。其中39例为I级,25例为IIa级, 3例为IIb级。术前均行下肢血管彩色多普勒及下肢血管CTA明确诊断。其中PMT组共37例,CDT组共30例。PMT组:男22例,女15例;年龄42~76岁,平均年龄(64.8±6.2)岁。合并疾病:动脉粥样硬化30例,糖尿病11例,高血压22例,房颤8例;缺血严重程度方面:IIb级2例,IIa级15例,I级 20例。CDT组:男18例,女12例,年龄46~78岁,平均年龄(65.5±5.5)岁。合并疾病:动脉粥样硬化24例,糖尿病9例,高血压18例,房颤6例;缺血严重程度方面:IIb级1例,IIa级10例,I级 19例。CDT组与PMT组患者术前资料差异均无统计学意义(均P>0.05)(表1)。
表1 两组术前资料比较
Table 1 Comparison of the preoperative data between the two groups
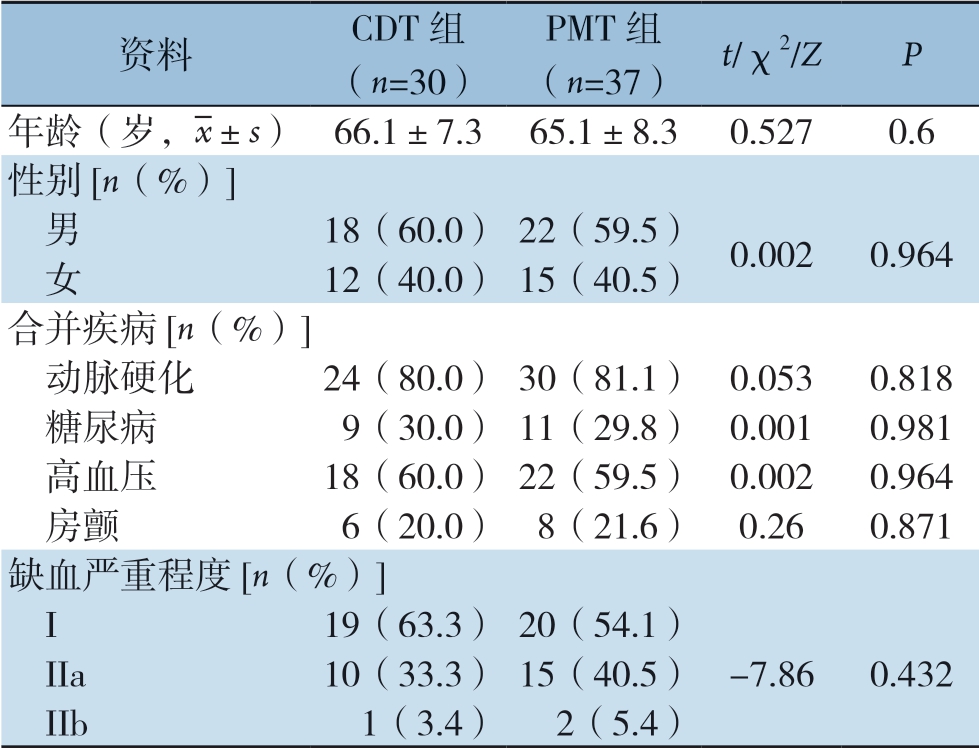
资料CDT组(n=30)PMT组(n=37)t/χ2/ZP年龄(岁,images/BZ_15_1000_2138_1036_2179.png±s)66.1±7.365.1±8.30.5270.6性别[n(%)]男18(60.0)22(59.5)0.0020.964 女12(40.0)15(40.5)合并疾病[n(%)]动脉硬化24(80.0)30(81.1)0.053 0.818 糖尿病9(30.0)11(29.8)0.0010.981 高血压18(60.0)22(59.5)0.002 0.964 房颤6(20.0)8(21.6)0.26 0.871缺血严重程度[n(%)]I19(63.3)20(54.1) IIa10(33.3)15(40.5)-7.86 0.432 IIb1(3.4)2(5.4)
1.2 治疗方法
1.2.1 PMT组 采用Angiojet血栓清除装置进行吸栓。穿刺对侧股动脉,翻山至病变侧,交换6 F翻山鞘造影明确血栓栓塞部位。首先20万U尿激酶溶解在250 mL生理盐水中,均匀喷洒至血栓段。30 min后开始吸栓,总的吸栓时间不超过240 s。术毕造影检查血管再通情况。对于局部重度狭窄的部位进一步行球囊扩张(PTA)+支架植入。吸栓过程中密切监测患者生命体征变化情况。
1.2.2 CDT组 DSA室下穿刺对侧股动脉,翻山至病变侧,交换6 F翻山鞘,造影明确病变段。取合适长度溶栓导管置于血栓栓塞段,经溶栓导管持续尿激酶泵入。鞘管内以肝素水持续泵入。3 d后拔除溶栓导管并造影检查血管再通情况。对于局部血管存在重度狭窄的进一步行PTA+支架植入。CDT期间密切监测患者凝血功能变化情况以及有无出血等并发症发生。
1.3 观察指标
观察两组患者术后一期血管开通情况;术中、术后并发症、住院时间、住院费用以及术后 1年后病变血管通畅率情况。
1.4 统计学处理
使用SPSS 19.0统计软件进行统计分析,连续变量以均数±标准差( ±s)表示,采用t检验;分类变量以百分比表示,采用χ2检验,P<0.05为差异有统计学意义。
±s)表示,采用t检验;分类变量以百分比表示,采用χ2检验,P<0.05为差异有统计学意义。
2 结 果
2.1 术中及疗效方面情况比较
两组在单纯行PMT或CDT后需进一步行PTA+支架植入方面、一期血管开通情况以及12个月一期血管通畅率方面均无统计学差异(均P>0.05)(表2)。
表2 两组疗效指标比较[n(%)]
Table 2 Comparison of the efficacy variables between the two groups [n (%)]
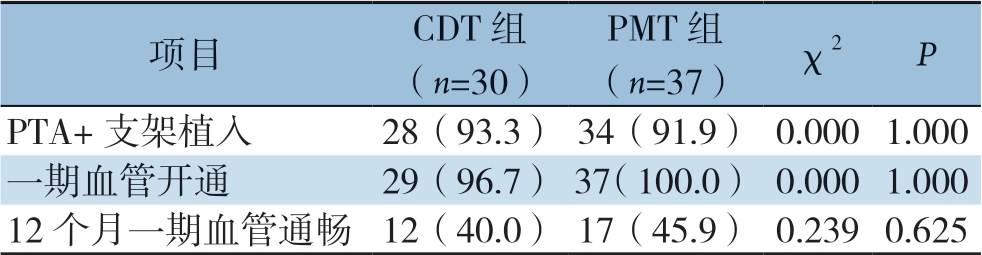
项目CDT组(n=30)PMT组(n=37)χ2P PTA+支架植入28(93.3)34(91.9)0.0001.000一期血管开通29(96.7)37(100.0)0.0001.000 12个月一期血管通畅12(40.0)17(45.9)0.2390.625
2.2 术后情况比较
PMT组的平均住院时间明显少于CDT组,但PMT组的平均住院费用明显高于CDT组(表3)。
表3 两组平均住院时间和费用比较( ±s)
±s)
Table 3 Comparison of the length of hospital stay and costs between the two groups ( ±s)
±s)

项目CDT组(n=30)PMT组(n=37)tP住院时间(d)8.9±0.65.8 ±0.8-16.2360.000住院费用(万元)4.8±0.87.0±1.18.968 0.000
2.3 术中及术后并发症发生情况及相关处理
两组术后在严重出血、截肢、穿刺处血肿、穿刺处感染以及肾功能不全方面无统计学差异(均P>0.05)。但PMT组术后总并发症发生率明显低于CDT组(表4)。所有并发症均得到对症处理:溶栓组1例出现严重脑出血,自动出院, 1例术后截肢,3例出现股动脉穿刺处局部血肿,予以局部压迫处理均好转,3例出现股动脉穿刺处局部感染,分别予以抗感染、局部换药等对症处理后均好转出院,无死亡病例。PMT组2例出现轻度肾功能不全,予以护肾、水化等对症治疗后均好转,出院时肾功能恢复正常。
表4 两组并发症情况比较[n(%)]
Table 4 Comparison of the complications between the two groups [n (%)]
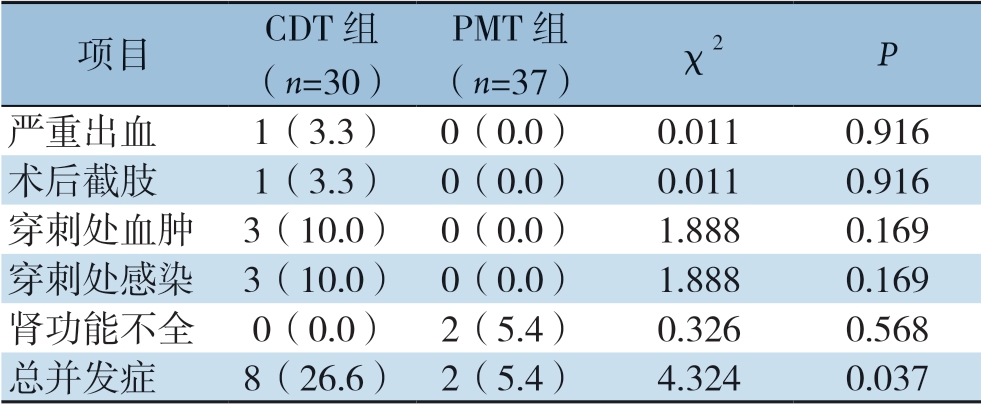
项目CDT组(n=30)PMT组(n=37)χ2P严重出血1(3.3)0(0.0)0.0110.916术后截肢1(3.3)0(0.0)0.0110.916穿刺处血肿3(10.0)0(0.0)1.8880.169穿刺处感染3(10.0)0(0.0)1.8880.169肾功能不全0(0.0)2(5.4)0.3260.568总并发症8(26.6)2(5.4)4.3240.037
3 讨 论
大样本的流行病学研究表明急性下肢缺血是导致截肢和死亡的重要原因之一[5],而下肢动脉血栓形成又是急性下肢缺血的重要原因之一。根据卢瑟福血管外科学对下肢缺血严重程度的分级和治疗选择,治疗上建议I级和IIa级的下肢缺血可优先考虑外科治疗开通血管,对于IIb级和III级的患者建议截肢。本例溶栓组1例术后截肢患者,术前的缺血程度达到IIb级。近年来,随着腔内介入技术的发展,腔内介入治疗在下肢动脉血栓的治疗中逐渐占据主流位置[6],目前主要的腔内介入手术主要包括CDT和PMT。CDT目前在国内大多数医院已成熟开展,但存在其局限性[7],如卧床时间长、尿激酶使用量大、出血风险高[8]。由于PMT在治疗效果上并不差于CDT,且术后总并发症发生率以及平均住院时间均较CDT低,导致PMT已慢慢成为了动脉血栓介入的主流方法。PMT作为下肢动脉血栓的治疗方法之一在国外已有多年临床经验了[9-11]。国外相关文献[12-15]已报道了PMT在下肢动脉血栓治疗中的优势。Silva等[16]一项多中心研究发现,AngioJet应用于下肢动脉硬化伴血栓形成,治疗成功率达91%,6个月保肢率达89%。Zeller等[15]曾报道PMT后通畅率高达92%。截肢率3%。Wissgott等[13]报道:PMT后的血管通畅率达到90%。1例出现严重的脑出血,无死亡病例。Bérczi等[17]报道的PMT术后通畅率为94%,但并发症高达31.5%。 12个月的一期通畅率为39%。无截肢和死亡病例。韩松等[18]报道PMT后通畅率高达90%以上。以上研究者所报道的PMT术后一期血管通畅率较本组PMT的结果相差不大,均低于本研究,主要与现代血管腔内器械的不断发展更新以及术者经验的不断丰富有关。术后并发症发生率相差较大,本研究术后并发症发生率PMT组5.4%,溶栓组26.7%。1例截肢患者考虑术前缺血时间较长,缺血程度已达到IIb级。肢体发生了不可逆性坏死。所有患者中出现穿刺处血肿以及感染均发生在CDT组,可能与持续的溶栓导管泵药,夜间患者翻身、屈髋均增加血肿和感染的风险。2例出现肾功能不全病例均发生在PMT组,考虑吸栓过程中同时破坏了大量红细胞,引发部分肾小管阻塞,造成一过性的肾功能损害[19]。通过碱化尿液[20]和水化以及护肾等对症治疗后均恢复正常。
对于急性下肢动脉血栓的介入治疗除了尽量提高一期血管通畅率,对如何提高远期通畅率[21-23]一直也是追求的目标之一。Bérczi等[17]报道12个月的吸栓一期通畅率为39%。本研究的12个月病变血管通畅率为43%。其中PMT组45.9%(17/37),CDT组 40.0%(12/30)。而Gabrielli等[24]研究报道的一期通畅率高达68%。远期通畅率除了和一期血管开通情况有关,同时还与患者的依从性有较大关系。术后规律服药以及定期复查可能会提高远期通畅率。
不同的介入方法在术后并发症方面有明显差异,可以看出本研究中CDT组的术后并发症发生率明显高于PMT组。但CDT也有其独特的优势[25],对于治疗远端小动脉血栓的患者,Angiojet导管往往无法达到病变部位。本研究未能将病变部位进行分类,存在一定缺陷。作为一项回顾性分析,本文样本量较少,对于严重出血、截肢、穿刺处血肿、穿刺处感染、肾功能不全等单一并发症的比较未见明显差异,但总的并发症发生率两组存在统计学差异。因此,仍需要大样本、多中心、随机对照试验来进一步评估。
PMT相比于CDT在治疗急性下肢动脉血栓引发的下肢急性缺血同样是安全、有效的。同时PMT明显降低术后总并发症发生率,缩短住院时间,但增加了平均住院费用。
[1]Davies MG. Criticial limb ischemia: epidemiology[J]. Methodist Debakey Cardiovasc J, 2012, 8(4):10-14.
[2]梁刚柱, 张福先, 罗小云, 等. 杂交手术在急性下肢动脉缺血救治中的应用[J]. 中国普通外科杂志, 2015, 24(12):1678-1682. doi:10.3978/j.issn.1005-6947.2015.12.008.Liang GZ, Zhang FX, Luo XY, et al. Application of hybrid procedures in treatment of acute limb ischemia[J]. Chinese Journal of General Surgery, 2015, 24(12):1678-1682. doi:10.3978/j.issn. 1005-6947.2015.12.008.
[3]Grip O, Kuoppala M, Acosta S, et al. Outcome and complications after intra-arterial thrombolysis for lower limb ischaemia with or without continuous heparin infusion[J]. Br J Surg, 2014, 101(9):1105-1112. doi: 10.1002/bjs.9579.
[4]赵国瑞, 任建庄, 陈鹏飞, 等. 急性下肢动脉栓塞导管取栓与支架植入临床疗效对比分析[J]. 介入放射学杂志, 2016, 25(10):853-857. doi:10.3969/j.issn.1008-794X.2016.10.004.Zhao GR, Ren JZ, Chen PF, et al. Transcatheter embolectomy and stent implantation for the treatment of acute lower limb arterial embolism: a comparative analysis of clinical efficacy[J]. Journal of Interventional Radiology, 2016, 25(10):853-857. doi:10.3969/j.issn.1008-794X.2016.10.004.
[5]Baril DT, Patel VI, Judelson DR, et al. Outcomes of lower extremity bypass performed for acute limb ischemia[J]. J Vasc Surg, 2013, 58(4):949-956. doi: 10.1016/j.jvs.2013.04.036.
[6]中华医学会外科学分会血管外科学组. 下肢动脉硬化闭塞症诊治指南[J]. 中华医学杂志, 2015, 95(24):1883-1896. doi:10.3760/cma.j.issn.0376-2491.2015.24.004.Vascular Surgery Group of Society of Surgery of Chinese Medical Association. Guidelines fordiagnosis and treatment of arteriosclerosis obliterans of the lower extremities[J]. National Medical Journal of China, 2015, 95(24):1883-1896. doi:10.3760/cma.j.issn.0376-2491.2015.24.004.
[7]薛冠华, 梁卫, 黄晓钟, 等. 导管溶栓治疗急性下肢动脉缺血的疗效评价[J]. 介入放射学杂志, 2010, 19(9):715-717. doi:10.3969/j.issn.1008-794X.2010.09.013. Xue GH, Liang W, Huang XZ, et al. Therapeutic evaluation of catheter-directed thrombolysis for the treatment of acute arterial ischemia of lower extremities[J]. Journal of Interventional Radiology, 2010, 19(9):715-717. doi:10.3969/j.issn.1008-794X.2010.09.013.
[8]Berridge DC, Kessel DO, Robertson I. Surgery versus thrombolysis for initial management of acute limb ischaemia[J]. Cochrane Database Syst Rev, 2013, (6):CD002784. doi: 10.1002/14651858.CD002784.
[9]Zeller T, Frank U, Burgelin K, et al. Long-term results after recanalization of acute and subacute thrombotic occlusions of the infra-aortic arteries and bypass-grafts using a rotational thrombectomy device[J]. Rofo, 2002, 174(12):1559-1565. doi: 10.1055/s-2002-35942.
[10]Kashyap VS, Gilani R, Bena JF, et al. Endovascular therapy for acute limb ischemia[J]. J Vasc Surg, 2011, 53(2):340-346. doi: 10.1016/j.jvs.2010.08.064.
[11]Byrne RM, Taha AG, Avgerinos E, et al. Contemporary outcomes of endovascular interventions for acute limb ischemia[J]. J Vasc Surg, 2014, 59(4):988-995. doi: 10.1016/j.jvs.2013.10.054.
[12]Zeller T, Muller C, Frank U, et al. The Straub-Rotarex thrombectomy system: initial experiences[J]. Rofo, 2001, 173(7):626-631. doi: 10.1055/s-2001-15843.
[13]Wissgott C, Kamusella P, Andresen R. Treatment of femoropopliteal stenoses and occlusions with mechanical rotational catheters: comparison of results with the Rotarex and Pathway devices[J]. J Cardiovasc Surg (Torino), 2012, 53(2):177-186.
[14]Wissgott C, Andresen R. Comments: interventional revascularisation of acute and subacute occlusions with the Rotarex device[J]. Zentralbl Chir, 2013, 138(5):575-581. doi: 10.1055/s-0033-1350653.
[15]Zeller T, Frank U, Burgelin K, et al. Early experience with a rotational thrombectomy device for treatment of acute and subacute infra-aortic arterial occlusions[J]. J Endovasc Ther, 2003, 10(2):322-331. doi: 10.1177/152660280301000224.
[16]Silva JA, Ramee SR, Collins TJ, et al. Rheolytic thrombectomy in the treatment of acute limb-threatening ischemia: immediate results and six-month follow-up of the multicenter AngioJet registry. Possis Peripheral AngioJet Study AngioJet Investigators[J]. Cathet Cardiovasc Diagn, 1998, 45(4):386-393.
[17]Bérczi V, Deutschmann HA, Schedlbauer P, et al. Early experience and midterm follow-up results with a new, rotational thrombectomy catheter[J]. Cardiovasc Intervent Radiol, 2002, 25(4):275-281.
[18]韩松, 周修适, 刘斐, 等. AngioJet在下肢动脉血栓栓塞性疾病治疗中应用[J]. 中国普通外科杂志, 2017, 26(12):1575-1582. doi:10.3978/j.issn.1005-6947.2017.12.011.Han S, Zhou XS, Liu F, et al. Application of AngioJet in treatment of lower extremity arterial thromboembolic disease[J]. Chinese Journal of General Surgery, 2017, 26(12):1575-1582. doi:10.3978/j.issn.1005-6947.2017.12.011.
[19]张雷, 陆清声, 裴轶飞, 等. AngioJet机械血栓抽吸技术在动脉栓塞及血栓形成中的应用体会[J]. 中国血管外科杂志:电子版, 2016, 8(3):203-207. doi:10.3969/j.issn.1674-7429.2016.03.010. Zhang L, Lu QS, Pei YF, et al. Experience of AngioJet mechanical thrombectomy treatment on acute arterial embolism[J].ChineseJournal of Vascular Surgery:ElectronicVersion, 2016, 8(3):203-207. doi:10.3969/j.issn.1674-7429.2016.03.010.
[20]Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review: Rhabdomyolysis--an overview for clinicians[J]. Crit Care, 2005 9(2):158-169. doi: 10.1186/cc2978.
[21]蒋俊豪. 腘动脉硬化性病变腔内治疗的技术要点[J]. 中国普通外科杂志, 2014, 23(6):724-726. doi:10.7659/j.issn.1005-6947.2014.06.003.Jiang JH. Technical tips for endovascular treatment of popliteal arteriosclerotic lesions[J]. Chinese Journal of General Surgery, 2014, 23(6):724-726. doi:10.7659/j.issn.1005-6947.2014.06.003.
[22]马震寰, 杨镛, 杨国凯, 等. 下肢动脉硬化闭塞症继发血栓形成治疗分析[J]. 中国普外基础与临床杂志, 2010, 17(3):275-277.Ma ZH, Yang Y, Yang GK, et al. Analysis on Treatment Of Arteriosclerosis Obliterans in Lower Limbs Accompanied with Thrombosis[J]. Chinese Journal of Bases and Clinics in General Surgery, 2010, 17(3):275-277.
[23]李杰, 常光其, 李松奇, 等. 下肢慢性缺血合并急性血栓形成的外科治疗[J]. 中国血管外科杂志:电子版, 2011, 3(4):226-228. doi:10.3969/j.issn.1674-7429.2011.04.010.Li J, Chang GQ, Li SQ, et al. Surgical treatment for chronic lower limb ischemia complicated with acute arterial thrombosis[J]. Chinese Journal of Vascular Surgery: Electronic Version, 2011, 3(4):226-228. doi:10.3969/j.issn.1674-7429.2011.04.010.
[24]Gabrielli R, Rosati MS, Carra A, et al. Outcome after preoperative or intraoperative use of intra-arterial urokinase thrombolysis for acute popliteal artery thrombosis and leg ischemia[J]. Thorac Cardiovasc Surg, 2015, 63(2):164-167. doi: 10.1055/s-0034-1378189.
[25]Dotter CT, Rösch J, Seaman AJ. Selective clot lysis with lowdose streptokinase[J]. Radiology, 1974, 111(1):31-37. doi: 10.1148/111.1.31.
