腹主动脉瘤腔内修复术(endovascular aneurysm repair,EVAR)已逐渐成为治疗腹主动脉瘤(abdominal aortic aneurysm,AAA)的主要治疗方式[1-3]。随着EVAR例数的增长以及随访时间的延长,EVAR术后相关并发症的病例明显增加[4-5],其中髂支闭塞是EVAR术后较为常见的并发症之一[6-7],文献报道其发生率约为5.5%[8]。目前,关于EVAR术后髂支闭塞的原因及治疗方式的选择目前仍存在争议。本文收集中南大学湘雅医院血管外科于2016年1月—2018年7月所收治的行EVAR的AAA患者资料,通过回顾性分析术后发生髂支闭塞的AAA患者临床资料,探讨髂支闭塞的可能病因和治疗方式,并评价治疗效果。
1 资料与方法
1.1 一般资料
回顾性收集130例AAA并接受EVAR患者,时间窗为2016年1月—2018年7月,其中男性101例,女性29例;平均年龄58.6(48~71)岁。所有患者均成功实施EVAR手术。EVAR术中所选腹主动脉覆膜支架包括一体式支架24和106例分体式支架。
1.2 随访
术后通过门诊或者电话随访,行CTA或者彩超复查。如有病情变化,及时通过电话沟通并我院就诊。
2 结 果
2.1 髂支闭塞病例基本资料
130例患者中,EVAR术后6例患者发生髂支闭塞,发生率为4.61%。6例患者均为男性。EVAR术后发生髂支闭塞的平均时间为(55±87)d,均为单侧髂支闭塞。患肢主要临床表现为患肢缺血症状如间歇性跛行(4例)或者静息痛(2例)。6例患肢中,4例髂支远端定位于髂外动脉,2例远端定位于髂总动脉。初步分析髂支狭窄原因有:1例患者瘤颈扭曲、成角大,2例患侧髂动脉严重扭曲,3例患者髂支远端锚定区或流出道血管重度狭窄,详细资料见表1。
表1 6 例髂支闭塞患者临床资料
Table 1 The general data of the 6 patients with iliac limb occlusion
病例年龄(岁) 性别 症状 形成时间(d) 病因 术式 疗效160 男 间歇性跛行 15 髂支远端锚定区狭窄 股动脉切开取栓+股-股动脉人工血管转流术 症状消失270 男 间歇性跛行 30 瘤颈成角大 股动脉切开取栓+股-股动脉人工血管转流术 症状消失346 男 静息痛 1 髂支开口狭窄 覆膜支架植入术 症状消失459 男 间歇性跛行 210 髂支远端锚定区狭窄 股动脉切开取栓+支架植入术 症状消失565 男 间歇性跛行 21 髂支扭曲 股动脉切开取栓+支架植入术 症状消失665 男 静息痛 1 髂支扭曲 股动脉切开取栓+支架植入术 症状消失
2.2 治疗方案
6例患者均采取手术治疗,无溶栓治疗。其中2例患者采用股动脉切开取栓+股-股动脉人工血管转流术,3例患者采用股动脉切开取栓+支架植入术,1例患者采用覆膜支架植入术。术后均给予抗凝或抗血小板治疗。
2.3 治疗结果
手术时间最长180 min,最短70 min,平均时间125 min。所有患肢均获得血流再通,手术成功率100%。6例患者术后缺血症状如间歇性跛行或静息痛症状完全消失,围手术期无并发症发生,顺利康复出院。
2.4 随访结果
出院后患者接受抗血小板治疗,6例患者于术后1、3、6、12个月均获得随访。经病史收集、影像学检查等方式获知,所有患肢血管均保持通畅,无缺血症状复发等表现。
3 讨 论
自从进入21世纪,EVAR以其手术效果优良、创伤小等优点,逐渐替代传统的开放式手术治疗腹主动脉瘤[9]。但随访过程中出现的手术并发症随之增多,如内漏、髂支闭塞等。因此,二次手术干预治疗EVAR术后并发症逐渐引起广大临床工作者的重视[10-11]。髂支闭塞是EVAR术后并发症之一,其主要临床表现为下肢急性或慢性缺血症状如间歇性跛行、下肢静息痛等;少部分患者无明显临床症状,通常影像学资料可明确诊断。故而,探讨髂支闭塞发生的原因,以及规范其治疗策略是后EVAR时代的重点和难点。
在本次回顾性临床研究 中,EVAR术后发生髂支闭塞的平均时间为55 d,其中5例均为1个月内出现的急性闭塞,临床症状包括患肢间歇性跛行和静息痛。所有患者EVAR术后均坚持服用抗血小板药物,因此暂不考虑停止药物所致髂支闭塞。6例患者所使用的均为腹主动脉分叉式覆膜支架,目前国内外文献暂未见支架种类与髂支闭塞发生有相关性,故暂不考虑支架类型导致患者髂支闭塞。在分析髂支闭塞的危险因素中,既往研究[12-14]发现,腹主动脉瘤分叉直径小、髂支延伸至髂外动脉、髂总动脉直径偏小是可能导致EVAR术后髂支闭塞的危险因素。在本研究中,我们发现远端锚定区血管狭窄以及远端锚定区的选择、髂支扭曲、瘤颈条件差也是是影响髂支闭塞发生的主要原因。
3.1 髂支远端锚定区狭窄及选择
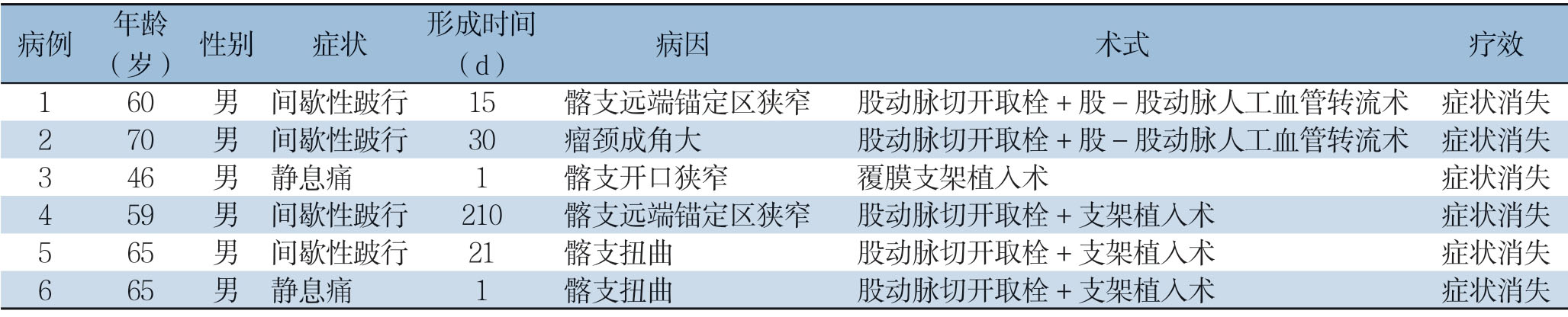
髂支远端锚定区如髂外动脉或者髂总动脉狭窄是导致髂支闭塞的重要因素。如图1所示,患者右侧髂支远端开口明显狭窄,髂动脉狭窄最小处直径仅2 mm,狭窄程度>75%。狭窄的髂外动脉引起髂支内血流动力学变化,易引起髂支内血栓形成,血栓向两端延伸引起严重的髂支闭塞和下肢急性缺血症状。类似地,由于解剖原因,动脉直径随着髂总动脉延伸至髂外动脉而减小,故而髂支从近端开口至远端开口形成喇叭状,更易引起髂支闭塞[15]。经过急诊行髂动脉球囊扩张+支架植入术,解除右下肢急性缺血症状,造影显示髂支及远端动脉通畅。因此,AAA不累及髂总动脉时,我们建议髂支锚定于髂总动脉,既可保留髂内动脉,又可减少髂支闭塞的风险;同时,如果术前或术中发现髂支远端锚定区或流出道血管狭窄,需利用球囊扩张技术解决狭窄问题或髂腿支架延伸至狭窄远心端,以减少髂支闭塞发生的可能性。
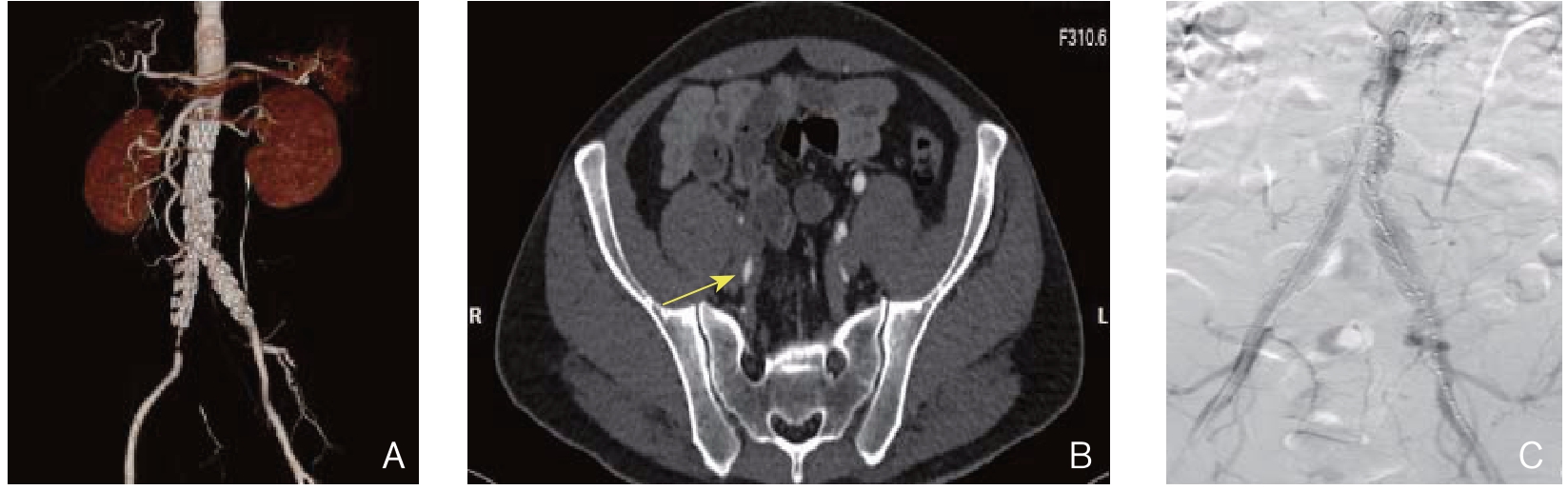
图1 髂支远端锚定区狭窄
Figure 1 Stenosis of the distal landing zone of the iliac limb
A:CT 三维重建图像显示EVAR 术后右侧髂支血栓形成,支架远端开口处狭窄明显;B:CT横断面显示右侧髂动脉支架远端开口处髂外动脉狭窄明显;C:行髂外动脉球囊扩张+支架植入术解决狭窄,造影显示血流恢复通畅
A:3D CT image reconstruction showing thrombus formation in the right iliac limb after EVAR,and evident stricture of the distal opening of the stent;B:CT cross-section image showing evident stricture of the external iliac artery in the distal opening of the right iliac stent;C:Resolution of stenosis after balloon dilatation and stent placement,and radiography showing the restored blood fl ow
3.2 髂支扭曲
髂支严重扭曲是导致EVAR术后髂支闭塞的另一个重要原因。如图2所示,由于患者髂动脉明显扭曲,置入的髂腿支架严重弯曲、打折,导致髂腿支架重度狭窄。马晓辉等[16]表明,EVAR术后髂支与髂动脉之间的相互作用力进一步加重后期髂支的变形、扭曲,导致髂支血栓形成。同时,Taudorf等[17]通过回顾性研究发现,髂支扭曲对EVAR术后髂支闭塞形成有重要促进作用。因此手术者在术前及术中需评估患者髂动脉的生理解剖特点,如有严重扭曲,需选择柔顺性较好的髂支移植物;术后造影如发现因扭曲而形成的髂支打折现象,需加用支撑性好的支架配合压力球囊,力争一次性处理髂支打折。如此,可有效降低EVAR术后髂支闭塞的发生率。
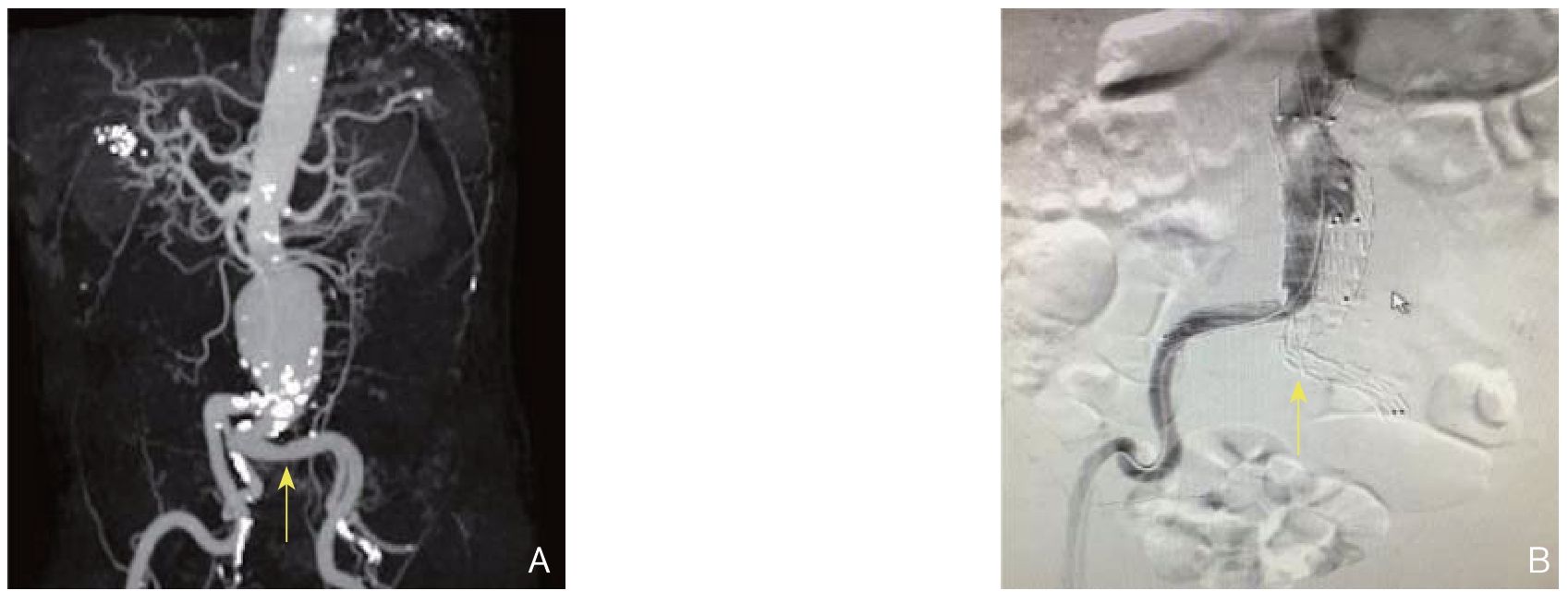
图2 髂支扭曲
Figure 2 Iliac stent-graft distortion
A:3D CT image reconstruction showing the severe distortion of the left iliac artery before EVAR;B:Radiography after EVAR showing thrombus formation in the left iliac limb and severe distortion of the left iliac stent-graft
A:CT 三维重建图像显示EVAR 术前左侧髂动脉扭曲严重;B:EVAR 术后造影显示左侧髂支血栓形成,左侧髂动脉支架扭曲严重
3.3 瘤颈条件差
瘤颈条件差,如成角大、瘤颈狭窄等亦是引起髂支闭塞的重要原因。如图3所示,瘤颈成角接近90°,且位于髂支开口处,故而一侧髂支开口被对侧髂支挤压而形成明显狭窄,导致髂支血栓形成。戈小虎等人称之为“盖帽效应”[18]。同时,瘤颈狭窄易导致髂支开口受阻而易形成狭窄。但EVAR由于其本身的限制,难以修正瘤颈成角大及狭窄等缺点;故而对于瘤颈条件差的患者,术者应警惕髂支闭塞这类并发症的发生,尽量避免将髂支开口于瘤颈狭窄或弯曲处重合。此外,考虑到瘤颈差所致内漏等情况,传统的开放式腹主动脉瘤切除+人工血管置换术也是一种选择。

图3 瘤颈条件差
Figure 3 Unfavorable features of the aneurysmal neck
A:CT 三维重建图像显示EVAR 术前AAA 瘤颈成角明显(>90 °);B:EVAR 术后CT 横断面显示右侧髂支开口明显受压、狭窄,右侧髂支内血栓形成
A:3D CT image reconstruction before EVAR showing angulation of the neck of the AAA (>90 °);B:CT cross-section image after EVAR showing the evident oppression and stricture of the opening of the right iliac limb and in-stent thrombosis of the iliac limb
3.4 治疗方式的选择
处理EVAR术后髂支闭塞这类并发症时,合理的治疗策略亦是保证治疗效果的根本。目前,有关EVAR术后髂支闭塞的治疗方式选择的相关报道较少,暂未见前瞻性临床研究,均为单中心经验分享,主要治疗方式包括[16,18-22]:股动脉切开取栓术,股动脉人工血管转流术,股动脉置管溶栓术,股动脉球囊扩张+支架植入术,以及髂动脉预防性植入裸支架等等。
对于治疗方式的选择,笔者的经验是“对因施治”,即根据患者发生髂支闭塞的原因选择合适的手术方式。⑴ 髂动脉扭曲,应在复合手术室实行手术:第一步将股动脉切开并采用双腔取栓导管将移植物内血栓清除完全;第二步在DSA辅助下明确髂支打折处,并导入支撑性好的支架配合压力球囊将狭窄处撑开。⑵ 髂支远端锚定区狭窄:单纯的血管腔内治疗即可解决。应导入长度合适的覆膜支架,近心端定位于髂支开口,远端覆盖髂动脉狭窄处。此种治疗方式需注意血栓脱落所致下肢远端栓塞,术中需造影明确下肢动脉通畅性。⑶ 瘤颈条件差:针对此类因素所致髂支闭塞,单纯血管腔内治疗效果不确切,且有使对侧髂腿支架狭窄或闭塞的风险。股-股动脉转流术,能行之有效的解决髂腿支架闭塞,并且术式简单,近期及远期疗效明确,值得推广。
髂支闭塞是EVAR术后并不罕见的并发症。本研究分析认为,髂支闭塞的原因包括瘤颈条件差、髂动脉入路扭曲、髂支远端锚定区解剖异常等。仔细分析髂支闭塞原因,有针对性地选择股动脉切开取栓和(或)血管腔内治疗,是行之有效的治疗方法。
当然,本研究仍然存在一定 局限性。本次研究是基于单中心的临床回顾性研究,病例数较小,需要更多的来自多个中心的病例验证本文所提出的观点。其次,本研究未通过统计学方法分析获得相关结论,更多的是描述性结论,属于经验分享和个案报道,影响本文结论的严谨性。
[1]Lederle FA,Freischlag JA,Kyriakides TC,et al.Long-term comparison of endovascular and open repair of abdominal aortic aneurysm[J].N Engl J Med,2012,367(21):1988-1997.doi:10.1056/NEJMoa1207481.
[2]兰勇,王征,李大军,等.主动脉EVAR治疗腹主动脉瘤的临床效果分析[J].中国普通外科杂志,2017,26(12):1628-1632.doi:10.3978/j.issn.1005-6947.2017.12.019.
Lan Y,Wang Z,Li DJ,et al.Analysis of clinical efficacy of aotic EVAR treatment of abdominal aortic aneurysm[J].Chinese Journal of General Surgery,2017,26(12):1628-1632.doi:10.3978/j.issn.1005-6947.2017.12.019.
[3]孙凯,胡何节.腔内修复术在复杂型肾下腹主动脉瘤中的应用[J].中国普通外科杂志,2015,24(12):1658-1663.doi:10.3978/j.issn.1005-6947.2015.12.004.
Sun K,Hu HJ.Endovascular repair for complex infrarenal abdominal aortic aneurysm[J].Chinese Journal of General Surgery,2015,24(12):1658-1663.doi:10.3978/j.issn.1005-6947.2015.12.004.
[4]Mehta M,Sternbach Y,Taggert JB,et al.Long-term outcomes of secondary procedures after endovascular aneurysm repair[J].J Vasc Surg,2010,52(6):1442-1449.doi:10.1016/j.jvs.2010.06.110.
[5]Wyss TR,Dick F,Brown LC,et al.The influence of thrombus,calcification,angulation,and tortuosity of attachment sites on the time to the first graft-related complication after endovascular aneurysm repair[J].J Vasc Surg,2011,54(4):965-971.doi:10.1016/j.jvs.2011.04.007.
[6]Maldonado TS,Rockman CB,Riles E,et al.Ischemic complications after endovascular abdominal aortic aneurysm repair[J].J Vasc Surg,2004,40(4):703-709.doi:10.1016/j.jvs.2004.07.032.
[7]Carroccio A,Faries PL,Morrissey NJ,et al.Predicting iliac limb occlusions after bifurcated aortic stent grafting:anatomic and device-related causes[J].J Vasc Surg,2002,36(4):679-684.
[8]Wang G,Zhai S,Li T,et al.Limb graft occlusion following endovascular aortic repair:Incidence,causes,treatment and prevention in a study cohort[J].Exp Ther Med,2017,14(2):1763-1768.doi:10.3892/etm.2017.4658.
[9]Adkar SS,Turner MC,Leraas HJ,et al.Low mortality rates after endovascular aortic repair expand use to high-risk patients[J].J Vasc Surg,2018,67(2):424-432.doi:10.1016/j.jvs.2017.06.107.
[10]Becquemin JP,Kelley L,Zubilewicz T,et al.Outcomes of secondary interventions after abdominal aortic aneurysm endovascular repair[J].J Vasc Surg,2004,39(2):298-305.doi:10.1016/j.jvs.2003.09.043.
[11]陈洪胜,郭媛媛,彭飞,等.腹主动脉瘤腔内修复术后髂支支架内闭塞的危险因素分析[J].中国普通外科杂志,2016,25(6):828-832.doi:10.3978/j.issn.1005-6947.2016.06.008.
Chen HS,Guo YY,Peng F,et al.Analysis of risk factors for iliac limb occlusion after endovascular repair of abdominal aortic aneurysm[J].Chinese Journal of General Surgery,2016,25(6):828-832.doi:10.3978/j.issn.1005-6947.2016.06.008.
[12]O'Neill S,Collins A,Harkin D.Limb occlusion after endovascular repair of an abdominal aortic aneurysm:beware the narrow distal aorta[J].Ir J Med Sci,2012,181(3):373-376.doi:10.1007/s11845-010-0464-8.
[13]Conway AM,Modarai B,Taylor PR,et al.Stent-graft limb deployment in the external iliac artery increases the risk of limb occlusion following endovascular AAA repair[J].J Endovasc Ther,2012,19(1):79-85.doi:10.1583/11-3550.1.
[14]Faure EM,Becquemin JP,Cochennec F,et al.Predictive factors for limb occlusions after endovascular aneurysm repair[J].J Vasc Surg,2015,61(5):1138-1145.doi:10.1016/j.jvs.2014.11.084.
[15]Coulston J,Baigent A,Selvachandran H,et al.Lack of Iliac Engagement Correlates With Iliac Limb Complications Following Standard EVAR[J].Vasc Endovascular Surg,2015,49(7):201-205.doi:10.1177/1538574415614403.
[16]马晓辉,郭伟,刘小平,等.腹主动脉瘤腔内修复术后髂支闭塞的治疗[J].中华普通外科杂志,2013,28(9):693-695.doi:10.3760/cma.j.issn.1007-631X.2013.09.013.
Ma XH,Guo W,Liu XP,et al.The management of graft limb occlusion following abdominal aortic aneurysm endovascular repair[J].Zhong Hua Pu Tong Wai Ke Za Zhi,2013,28(9):693-695.doi:10.3760/cma.j.issn.1007-631X.2013.09.013.
[17]Taudorf M,Jensen LP,Vogt KC,et al.Endograft limb occlusion in EVAR:iliac tortuosity quantified by three different indices on the basis of preoperative CTA[J].Eur J Vasc Endovasc Surg,2014,48(5):527-533.doi:10.1016/j.ejvs.2014.04.018.
[18]戈小虎,方青波,管圣,等.EVAR术后瘤颈解剖源性的髂支闭塞危险因素分析[J].血管与腔内血管外科杂志,2015,1(2/3):92-94.
Ge XH,Fang QB,Guan S,et al.Analysis of risk factors for iliac limb occlusion after EVAR due to anatomical reasons of aneurysmal neck[J].Journal of Vascular and Endovascular Surgery,2015,1(2/3):92-94.
[19]唐骁,符伟国,郭大乔,等.支架植入预防腹主动脉瘤腔内修复术后髂支血栓形成的疗效研究[J].中国血管外科杂志:电子版,2012,4(4):218-220.doi:10.3969/j.issn.1674-7429.2012.04.009.
Tang X,Fu WG,Guo DQ,et al.The stent implantation reducing the risk of iliac limb occlusions following endovascular abdominal aortic aneurysm repair[J].Chinese Journal of Vascular Surgery:Electronic Version,2012,4(4):218-220.doi:10.3969/j.issn.1674-7429.2012.04.009.
[20]van Zeggeren L,Bastos Gonçalves F,van Herwaarden JA,et al.Incidence and treatment results of Endurant endograft occlusion[J].J Vasc Surg,2013,57(5):1246-1254.doi:10.1016/j.jvs.2012.11.069.
[21]Leurs LJ,Harris PL,Buth J,et al.Secondary interventions after elective endovascular repair of degenerative thoracic aortic aneurysms:results of the European collaborators registry (EUROSTAR)[J].J Vasc Interv Radiol,2007,18(4):491-495.doi:10.1016/j.jvir.2007.01.018.
[22]葛红卫,朱云峰,朱永斌,等.腹主动脉瘤腔内修复术中髂动脉瘤的处理策略[J].中国普通外科杂志,2015,24(6):787-791.doi:10.3978/j.issn.1005-6947.2015.06.004.
Ge HW,Zhu YF,Zhu YB,et al.Treatment strategy of iliac artery aneurysm in endovascular repair for abdominal aortic aneurysm[J].Chinese Journal of General Surgery,2015,24(6):787-791.doi:10.3978/j.issn.1005-6947.2015.06.004.
