直肠癌是世界上最常见的癌症之一[1]。随着腹腔镜技术的不断进步,多项临床研究表明,与开放的全直肠系膜切除(TME)相比,腹腔镜辅助TME(LaTME)无论是短期还是长期的疗效都与开腹手术相当。然而,LaTME在治疗低位直肠癌患者中的作用是有限的,即使是拥有超低位括约肌保肛技术、腹腔镜手术经验丰富的外科医生,也面临着环周切缘(CRM)阳性的风险;此外,狭窄骨盆、男性和高体质量指数(BMI)的患者也不利于LaTME的开展,由于肿瘤远端边缘的视野有限,LaTME转开放手术率一直居高不下。这就需要外科医生找到新的替代方式来治疗直肠癌,特别是那些低位直肠癌的患者。腹腔镜辅助经肛TME(TaTME)采用经肛进入盆腔的入路方式,可更直接地进入低位直肠系膜的周围间隙,相对简便地完成远端直肠系膜的游离切除,可能更有利于确保CRM的安全性,得到更高质量的TME手术切除标本[2]。为低位直肠癌切除术提供了一种创新的微创选择,给外科医生提供新的解决方案。本研究收集了广东省中医院(广州中医药大学第二附属医院)胃肠外科收治的12例行腹腔镜辅助TaTME和同期18例行LaTME低位直肠患者的临床资料,对比分析两者的近期疗效。现报告如下。
1 资料与方法
1.1 一般资料
收集广东省中医院胃肠外科2018年7月—2019年1月30例低位直肠癌患者的临床资料。其中男19例,女11例;年龄34~74岁,平均(63.4±8.63)岁。纳入标准:⑴ 术前均由病理组织检查诊断为直肠腺癌;⑵ 术前诊断分期为I、II、III期结直肠癌[3];⑶ 术前MRI检查、肛门指检提示肿瘤下缘距肛门距离≤5 cm;⑷年龄18~75岁。排除标准:⑴ 合并其他恶性肿瘤;⑵ 肿瘤导致梗阻、穿孔等需急诊手术;⑶ 术前肿瘤学分期为Ⅳ[3];⑷ 合并有严重心肺疾患等。根据手术方式不同分为两组,其中12例腹腔镜辅助TaTME(TaTME组),男6例,女6例;18例行LaTME(LaTME组),男13例,女5例。两组患者年龄、性别、BMI、ASA分级、肿瘤分期、肿瘤距肛门距离、肿瘤直径等一般资料比较差异无统计学意义(均P>0.05)(表1)。所有患者或其家属术前均签署知情同意书。
表1 两组患者的一般资料
Table1 General information of the two groups of patients
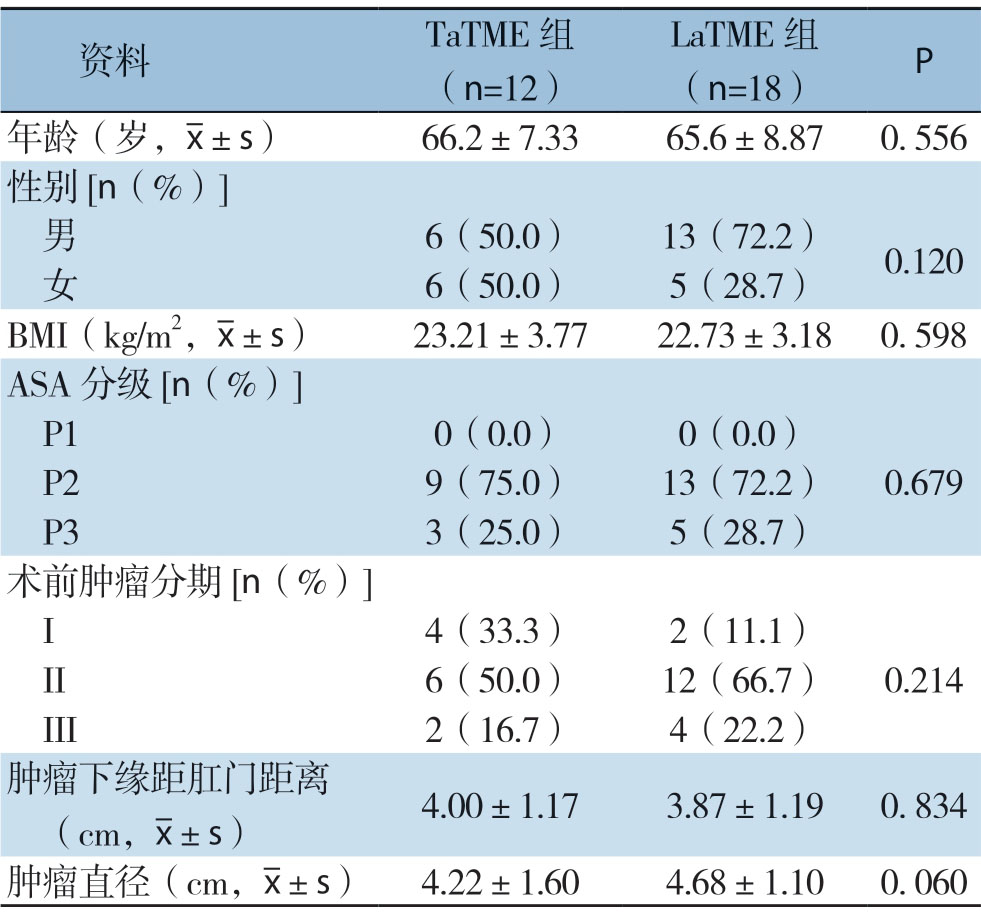
资料 TaTME组(n=12)LaTME组(n=18)P年龄(岁,images/BZ_44_705_2248_734_2291.png±s)66.2±7.33 65.6±8.87 0.556性别[n(%)]男 6(50.0)13(72.2)0.120 女 6(50.0)5(28.7)BMI(kg/m2,images/BZ_44_705_2248_734_2291.png±s)23.21±3.77 22.73±3.18 0.598 ASA分级[n(%)]P1 0(0.0)0(0.0)P2 9(75.0)13(72.2)0.679 P3 3(25.0)5(28.7)术前肿瘤分期[n(%)]I 4(33.3)2(11.1)II 6(50.0)12(66.7)0.214 III 2(16.7)4(22.2)肿瘤下缘距肛门距离(cm,images/BZ_44_705_2248_734_2291.png±s)4.00±1.17 3.87±1.19 0.834肿瘤直径(cm,images/BZ_44_705_2248_734_2291.png±s)4.22±1.60 4.68±1.10 0.060
1.2 手术方法
1.2.1 腹腔镜辅助TaTME 分两组人员同时进行。腹部腹腔镜操作:采用常规五孔法。术者立于患者右侧,一助手站于患者左侧,扶镜手站于术者右侧。切开乙状结肠系膜根部右侧后腹膜,清扫肠系膜下动脉根部淋巴结,并结扎、离断肠系膜下动脉,同法离断肠系膜下静脉;沿腹膜后间隙继续向左侧游离乙状结肠及降结肠系膜至左结肠旁沟,剪开乙状结肠系膜根部左侧后腹膜,游离乙状结肠及降结肠;向下游离直肠,在游离过程中注意保护两侧输尿管及神经,分离至腹膜反折。经肛门操作:充分扩肛,冲洗消毒肿瘤远端直肠、肛管,小拉钩牵开肛门(图1A),直视下距肿瘤下缘2 cm 处行直肠黏膜下荷包缝合以封闭直肠腔,隔离肿瘤及细菌(图1B)。置入STARPORT(图1C);向盆腔内灌注CO2,建立气腹,置入腹腔镜及操作器械,腔镜视野下于缝合线远端环形切开直肠壁各层组织(图1D);进入直肠系膜与盆底筋膜之间的肛提肌上间隙,转而后方循盆筋膜脏层及壁层之间向上游离直肠系膜,注意避免损伤骶前静脉(图1E);侧方向上游离解剖直肠侧韧带,注意避免损伤盆腔神经丛、NVB(图1F);前方沿Denovillivers 筋膜向上游离,注意避免损伤囊腺(或阴道)、尿道或前列腺(图1G);逐步向上游离与腹腔镜操作组汇合(图1H)。经肛门脱出直肠,于距离肿瘤上端10 cm 处离断肠管,移除标本,手工行结肠直肠端端吻合,留置肛管及盆腔引流管,逐层缝合手术切口完成手术。
1.2.2 LaTME 行标准的腹腔镜下直肠癌根治术[4-5]。前面步骤同TaTME 腹腔镜操作;自上而下,按后方、前方、两侧的顺序进行游离直肠,在游离过程中注意保护两侧输尿管及神经;游离直肠系膜后于肿瘤远端1~2 cm 处离断直肠;于耻骨联合上约5 cm 切口,取出肿瘤标本;腹腔镜下行结肠与直肠肛管吻合。
1.3 观察指标
手术情况:手术时间、出血量、预防性造口、保肛情况;肿瘤学指标:淋巴结清扫总数、环周切缘阳性率;术后并发症情况:吻合口出血、吻合口瘘、肠梗阻、切口感染;术后恢复情况:术后排气时间、全流饮食时间、术后住院时间、住院费用。
1.4 统计学处理
采用SPSS 20.0统计软件行数据分析。计数资料用例数(百分比)[n(%)]表示,行χ2检验;计量资料以均数±标准差( ±s)表示,行t检验。P<0.05为差异有统计学意义。
±s)表示,行t检验。P<0.05为差异有统计学意义。
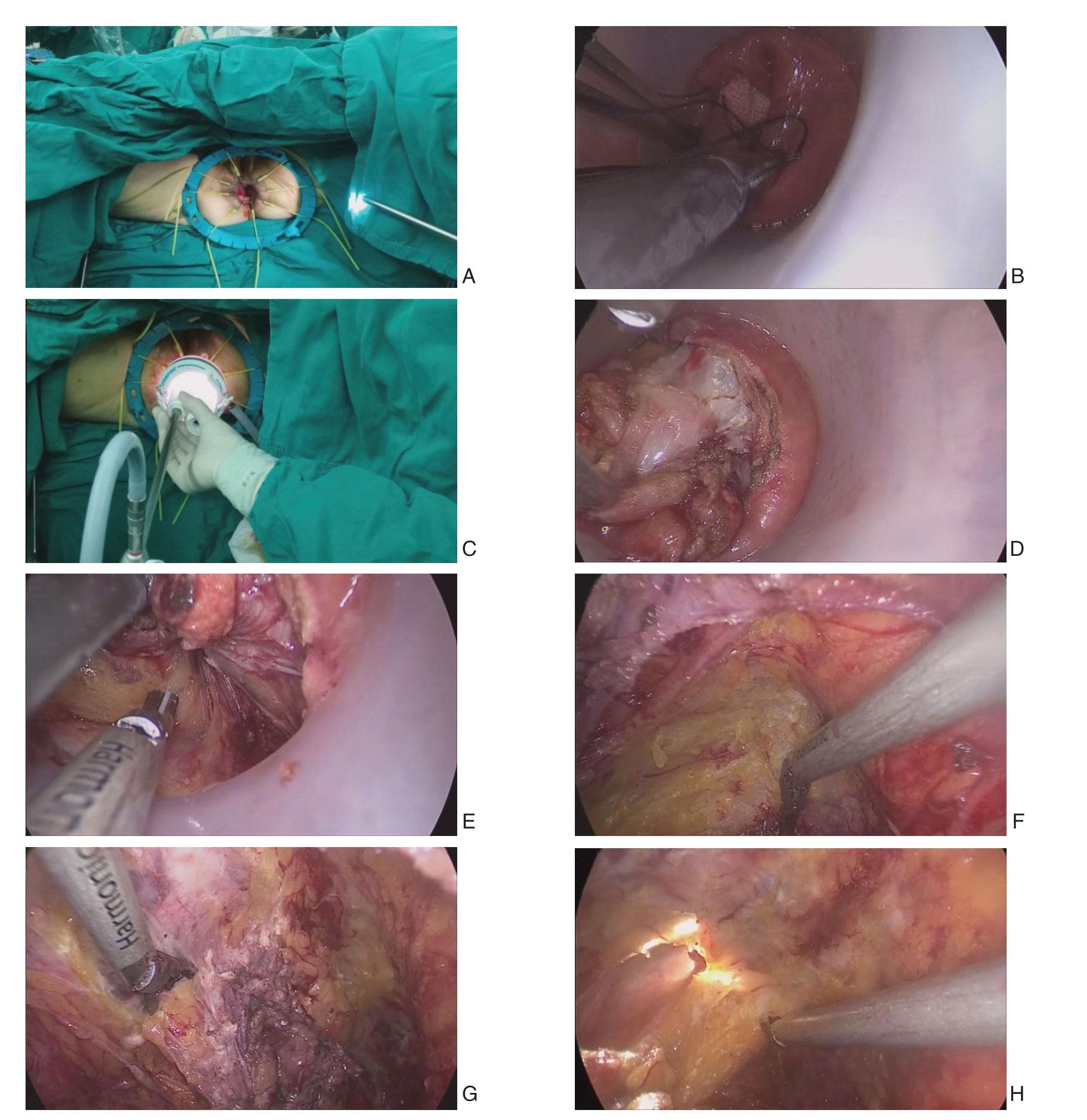
图1 腹腔镜辅助TaTME术中照片 A:环形肛门拉钩充分暴露肛门;B:荷包缝合闭合肠腔;C:建立经肛平台(STARPORT);D:切开直肠肠壁;E:进入肛提肌间隙;F:侧方游离直肠系膜;G:前方游离直肠系膜;H:与经腹方汇合
Figure1 Intraoperative views of laparoscopic-assisted TaTME A:Sufficient Exposure of the anal canal by the anal retractor;B:Closure of the lumen of the rectum with purse-string suture;C:Creation of a transanal platform (STARPORT);D:Incision of the wall of the rectum;E:Entering into the space of the levator ani muscle;F:Lateral dissociation of the mesorectum;G:Anterior dissociation of the mesorectum;H:Meeting transabdominal side
2 结 果
2.1 手术相关指标和标本情况比较
腹腔镜辅助TaTME组的手术时间比LaTME组手术时间短、出血量更少,差异有统计学意义(均P<0.05)。在预防性造口、淋巴结清扫总数、保肛率、环周切缘阳性率方面两组差异无统计学意义(均P>0.05)(表2)。
2.2 术后并发症及术后恢复情况比较
腹腔镜辅助TaTME术后住院时间较LaTME更短、住院费用更低,差异有统计学意义(均P<0.05)。LaTME发生1例吻合口瘘,但两组的术后总并发症差异无统计学意义(P>0.05)。腹腔镜辅助TaTME组的术后排气时间及全流饮食时间较LaTME组短,但差异均未达统计学意义(均P>0.05)(表3)。
表2 两组患者的手术相关指标与手术标本情况比较
Table2 Comparison of surgical-related indicators and surgical specimens between the two groups of patients
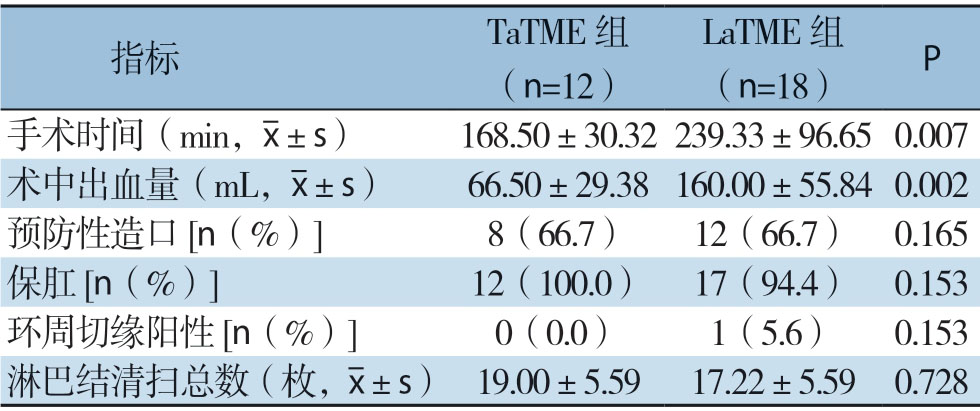
指标 TaTME组(n=12)LaTME组(n=18)P手术时间(min,images/BZ_44_705_2248_734_2291.png±s)168.50±30.32 239.33±96.65 0.007术中出血量(mL,images/BZ_44_705_2248_734_2291.png±s)66.50±29.38 160.00±55.84 0.002预防性造口[n(%)]8(66.7)12(66.7)0.165保肛[n(%)]12(100.0)17(94.4)0.153环周切缘阳性[n(%)]0(0.0)1(5.6)0.153淋巴结清扫总数(枚,images/BZ_44_705_2248_734_2291.png±s)19.00±5.59 17.22±5.59 0.728
表3 两组患者术后并发症与术后恢复情况比较
Table3 Comparison of postoperative complications and postoperative recovery between the two groups
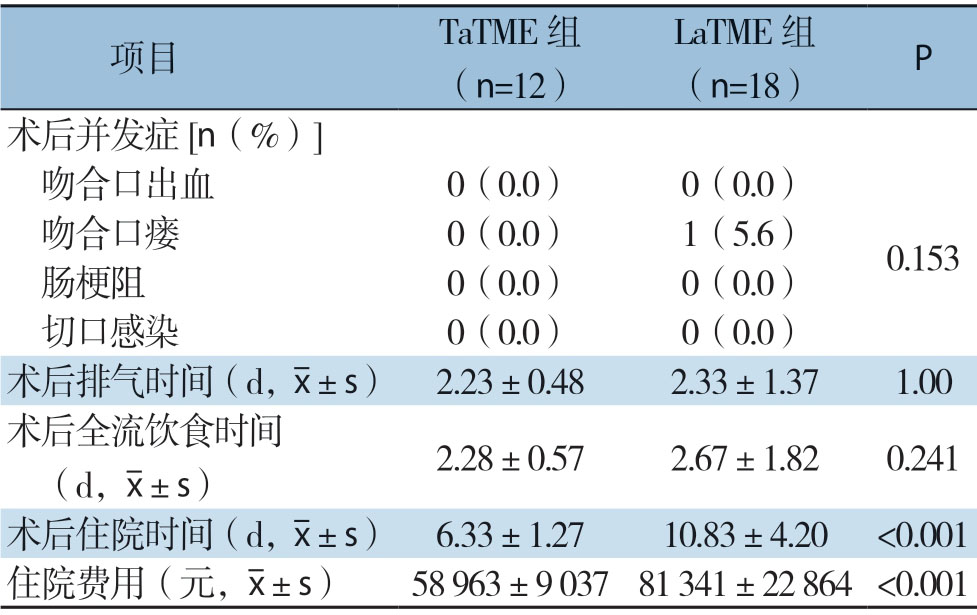
项目 TaTME组(n=12)LaTME组(n=18)P术后并发症[n(%)]吻合口出血 0(0.0)0(0.0)吻合口瘘 0(0.0)1(5.6)0.153 肠梗阻 0(0.0)0(0.0)切口感染 0(0.0)0(0.0)术后排气时间(d,images/BZ_44_705_2248_734_2291.png±s)2.23±0.48 2.33±1.37 1.00术后全流饮食时间(d,images/BZ_44_705_2248_734_2291.png±s)2.28±0.57 2.67±1.82 0.241术后住院时间(d,images/BZ_44_705_2248_734_2291.png±s)6.33±1.27 10.83±4.20<0.001住院费用(元,images/BZ_44_705_2248_734_2291.png±s)58 963±9 037 81 341±22 864<0.001
3 讨 论
TaTME根据是否有腹腔镜的辅助可分为完全TaTME(Pure-NOTES TaTME)和腹腔镜辅助TaTME。完全TaTME 手术虽然在技术上是可行的,且更加符合NOTES理念;但是完全TaTME的缺点也很明显:第一,中转开腹和术中并发症高[6];如盆腔周围的损伤、盆腔感染;第二,直肠肠腔狭窄,操作困难,容易进入错误的间隙,一旦出血难以控制[7];第三,经肛难以保证直肠系膜的完整切除,导致术后患者的局部复发[8];更为主要的是,完全TaTME手术由于“先处理肿瘤再离断血管”,且无法彻底探查腹腔,有悖于直肠癌根治手术的基本原则;完全TaTME为逆向操作,手术难度大,学习曲线长[9]。腹腔镜辅助TaTME既能发挥经肛门入路的优势,操作难度又比完全经肛门入路进行全直肠系膜切除低,比后者更适合在当前情况下先行开展,目前绝大多数学者均倾向于使用联合腹腔镜辅助完成TaTME[10]。LaTME在治疗中低位直肠癌尤其是“困难骨盆”,包括肥胖男性、骨盆狭窄、前列腺肥大、直肠系膜肥厚等的患者,游离直肠远端往往变得非常困难,经常导致TME完整性受损、切缘阳性风险增加[11-12]。TaTME采用经肛门入路的方式,不仅可以克服腹腔镜下操作困难的问题,还可以通过腹腔镜的放大作用获得更好的视野,在直视下精确地确定肿瘤的下缘,降低远端直肠的游离难度,提高TME的质量,降低CRM的阳性率,降低局部复发率[13-15]。
CRM和直肠系膜的完整性是影响直肠癌术后局部复发重要指标[16-18]。一项国际多中心随机试验[19]提示,TaTME的CRM阳性率低于LaTME;一项纳入7个研究[20],包括573例患者(TaTME组270例;LaTME组303例)的Meta分析表明,与laTME相比,TaTME的直肠系膜标本完整度更高(OR=1.75,95% CI=1.02~3.01,P=0.04)和更低的CRM阳性率(阳性CRM:OR=0.39,95% CI= 0.17~0.86,P=0.02)。而Marks等[21]对TaTME和LaTME在直肠系膜完整性和CRM阳性等方面进行了系统回顾和Meta分析,结果显示两者差异无统计学意义。多项临床数据分析[21-23]表明,TaTME与LaTME在TME质量、CRM阳性率、淋巴结总数等方面比较差异无统计学意义。笔者中心TaTME与LaTME的CRM阳性率和淋巴结清扫总数差异无统计学意义,但在手术标本的TME质量缺乏有效的数据分析,有待下一步的临床研究证实。
吻合口瘘是直肠癌术后是最常见的并发症之一,直肠癌术后吻合口瘘的发生率居高不下[24-25]。同时,吻合口瘘还会增加直肠癌局部复发率,降低患者长期生存率[26-28]。有研究[29-30]表明,TaTME在直视下切开直肠壁各层组织,避免了用直切切割闭合器离断直肠,可能会降低吻合口瘘的发生率。此外,TaTME手术在直视下缝合加固吻合口,可以降低吻合口瘘和出血的风险[31-32]。而 Lacy等[33]发表的一项纳入140例TaTME治疗直肠癌的研究结果表明,与他的LaTME相比,TaTME术后吻合口瘘的发生率并没有显著降低(8.2% vs.7.3%)。另一项Meta分析也表明TaTME和LaTME在吻合瘘等术后并发症方面无差异[20]。笔者中心腹腔镜辅助TaTME采用的直视下手工行结肠直肠端端吻合、加强吻合口缝合、吻合口充气测漏试验等对降低术后吻合口瘘的发生也起到一定的作用。
腹腔镜辅助TaTME经腹与经肛门手术同时进行,两者相互指引、帮助,可以缩短手术时间。近期的一项病例配对研究[34]比较了LaTME手术和TaTME手术的安全性,结果表明,TaTME组在手术时间(比LaTME减少37 min)和住院时间(比LaTME减少2.2 d)方面均有明显优势。Ma等[20]发表的一项Meta分析提示,TaTME组的手术时间较LaTME短。但是,腹腔镜辅助TaTME也存在一些弊端:TaTME经腹手术和经肛门手术同时进行,不仅增加一组手术人员和器械护士,还需要增加一份手术器械,提高了手术的成本和费用;本中心采用经肛门脱出直肠,手工离断肠管近端,在直视下行手工下结肠直肠端端缝合,减少了手术器械的使用,节约了手术成本;同时,腹腔镜辅助TaTME 经肛和经腹手术同时进行来优化时间,比LaTME手术更短。此外,即便腹腔镜辅助TaTME虽然避免了经腹取出手术标本,但是仍然存在腹部切口疼痛、瘢痕,甚至导致切口疝等并发症的发生[35]。
本研究也存在一些不足;第一,TaTME病例开展较少,技术尚未成熟;其次,未能记录手术标本TME质量及患者肛门功能;最后,患者的远期生存状况仍需进一步的数据证实。
总之,腹腔镜辅助TaTME治疗低位直肠癌与laTME的短期疗效相当,甚至在某些方面具有一定优势,是安全可行的,值得临床进一步研究与探索。
[1]Siegel RL,Miller KD,Jemal A.Cancer statistics,2015[J].CA Cancer J Clin,2015,65(1):5-29.doi:10.3322/caac.21254.
[2]中华医学会外科学分会结直肠外科学组,中华医学会外科学分会腹腔镜与内镜外科学组.直肠癌经肛全直肠系膜切除专家共识及手术操作指南(2017版)[J].中国实用外科杂志,2017,37(9):978-984.doi:10.19538/j.cjps.issn1005-2208.2017.09.12.
Colorectal Surgery Group of Surgery Branch of Chinese Medical Association,Laparoscopic and Endoscopic Surgery Group of Surgery Branch of Chinese Medical Association.Transanal total mesorectal excision for rectal cancer:expert consensus and operation guidelines (2017 edition)[J].Chinese Journal of Practical Surgery,2017,37(9):978-984.doi:10.19538/j.cjps.issn1005-2208.2017.09.12.
[3]Benson AB 3rd,Venook AP,Cederquist L,et al.Colon Cancer,Version 1.2017,NCCN Clinical Practice Guidelines in Oncology[J].J Natl Compr Canc Netw,2017,15(3):370-398.doi:10.6004/jnccn.2017.0036.
[4]郑民华.腹腔镜低位直肠癌根治术[J].中华普外科手术学杂志:电子版,2013,7(2):99.doi:10.3877/cma.j.issn.1674-3946.2013.02.025.
Zheng MH.Improved therapeutic level of standardized laparoscopic surgery for rectal cancer[J].Chinese Journal of Operative Procedures of General Surgery:Electronic Version,2013,7(2):99.doi:10.3877/cma.j.issn.1674-3946.2013.02.025.
[5]池畔.腹腔镜低位直肠癌根治术[J].中国实用外科杂志,2011,31(9):867-870.
Chi P.Laparoscopic radical resection of low rectal cancer[J].Chinese Journal of Practical Surgery,2011,31(9):867-870.
[6]Penna M,Hompes R,Arnold S,et al.Transanal Total Mesorectal Excision:International Registry Results of the First 720 Cases[J].Ann Surg,2017,266(1):111-117.doi:10.1097/SLA.0000000000001948.
[7]Tuech JJ,Karoui M,Lelong B,et al.A step toward NOTES total mesorectal excision for rectal cancer:endoscopic transanal proctectomy[J].Ann Surg,2015,261(2):228-233.doi:10.1097/SLA.0000000000000994.
[8]Chi P,Chen Z,Lu X.Transanal Total Mesorectal Excision:Can it Achieve the Standard of TME?[J].Ann Surg,2017,266(6):e87-88.doi:10.1097/SLA.0000000000001735.
[9]Wolthuis AM,Bislenghi G,de Buck van Overstraeten A,et al.Transanal total mesorectal excision:Towards standardization of technique[J].World J Gastroenterol,2015,21(44):12686-12695.doi:10.3748/wjg.v21.i44.12686.
[10]康亮,陈文豪,蔡永华,等.单孔腹腔镜辅助经肛门全直肠系膜切除临床应用价值及展望[J].中国实用外科杂志,2016,36(1):71-74.doi:10.7504/CJPS.ISSN1005-2208.2016.01.21.
Kang L,Chen WH,Cai YH,et al.Clinical application and prospect of single-port laparoscopic assisted transanal total mesorectal excision[J].Chinese Journal of Practical Surgery,2016,36(1):71-74.doi:10.7504/CJPS.ISSN1005-2208.2016.01.21.
[11]Rouanet P,Mourregot A,Azar CC,et al.Transanal endoscopic proctectomy:an innovative procedure for difficult resection of rectal tumors in men with narrow pelvis[J].Dis Colon Rectum,2013,56(4):408-415.doi:10.1097/DCR.0b013e3182756fa0.
[12]Bondeven P,Hagemann-Madsen RH,Laurberg S,et al.Extent and completeness of mesorectal excision evaluated by postoperative magnetic resonance imaging[J].Br J Surg,2013,100(10):1357-1367.doi:10.1002/bjs.9225.
[13]Kang L,Chen WH,Luo SL,et al.Transanal total mesorectal excision for rectal cancer:a preliminary report[J].Surg Endosc,2016,30(6):2552-2562.doi:10.1007/s00464-015-4521-2.
[14]Park SJ,Lee KY,Choi SI,et al.Pure NOTES rectosigmoid resection:transgastric endoscopic IMA dissection and transanal rectal mobilization in animal models[J].J Laparoendosc Adv Surg Tech A,2013,23(7):592-595.doi:10.1089/lap.2012.0551.
[15]韩加刚,王振军.低位直肠癌保肛手术方式选择[J].中国实用外科杂志,2019,39(7):676-680.
Han JG,Wang ZJ.Selection of anal preservation surgery of low rectal cancer[J].Chinese Journal of Practical Surgery,2019,39(7):676-680.
[16]Nagtegaal ID,Quirke P.What is the role for the circumferential margin in the modern treatment of rectal cancer?[J].J Clin Oncol,2008,26(2):303-312.doi:10.1200/JCO.2007.12.7027.
[17]Quirke P,Steele R,Monson J,et al.Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer:a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial[J].Lancet,2009,373(9666):821-828.doi:10.1016/S0140-6736(09)60485-2.
[18]张仕林,韦国祥,彭厚坤.腹腔镜根治术与传统开腹手术治疗结直肠癌的近期疗效及远期生存的比较[J].中国普通外科杂志,2019,28(7):897-902.doi:10.7659/j.issn.1005-6947.2019.07.018.
Zhang SL,Wei GX,Peng HK.Comparison of short-term therapeutic effect and long-term survival of laparoscopic radical resection and conventional laparotomy operation for treatment of colorectal cancer[J].Chinese Journal of General Surgery,2019,28(7):897-902.doi:10.7659/j.issn.1005-6947.2019.07.018.
[19]Deijen CL,Velthuis S,Tsai A,et al.COLOR III:a multicentre randomised clinical trial comparing transanal TME versus laparoscopic TME for mid and low rectal cancer[J].Surg Endosc,2016,30(8):3210-3215.doi:10.1007/s00464-015-4615-x.
[20]Ma B,Gao P,Song Y,et al.Transanal total mesorectal excision (taTME) for rectal cancer:a systematic review and meta-analysis of oncological and perioperative outcomes compared with laparoscopic total mesorectal excision[J].BMC Cancer,2016,16:380.doi:10.1186/s12885-016-2428-5.
[21]Marks JH,Montenegro GA,Salem JF,et al.Transanal TATA/TME:a case-matched study of taTME versus laparoscopic TME surgery for rectal cancer[J].Tech Coloproctol,2016,20(7):467-473.doi:10.1007/s10151-016-1482-y.
[22]Rasulov AO,Mamedli ZZ,Gordeyev SS,et al.Short-term outcomes after transanal and laparoscopic total mesorectal excision for rectal cancer[J].Tech Coloproctol,2016,20(4):227-234.doi:10.1007/s10151-015-1421-3.
[23]Araujo SE,Perez RO,Seid VE,et al.Laparo-endoscopic Transanal Total Mesorectal Excision (TATME):evidence of a novel technique[J].Minim Invasive Ther Allied Technol,2016,25(5):278-287.doi:10.1080/13645706.2016.1199435.
[24]Qu H,Liu Y,Bi DS.Clinical risk factors for anastomotic leakage after laparoscopic anterior resection for rectal cancer:a systematic review and meta-analysis[J].Surg Endosc,2015,29(12):3608-3617.doi:10.1007/s00464-015-4117-x.
[25]韩彩文,闫沛静,蔡辉,等.机器人辅助和腹腔镜手术治疗直肠癌疗效与安全性比较的Meta分析[J].中国普通外科杂志,2019,28(4):399-406.doi:10.7659/j.issn.1005-6947.2019.04.004.
Han CW,Yan PJ,Cai H,et al.Efficacy and safety of roboticassisted versus conventional laparoscopic proctectomy:a Metaanalysis[J].Chinese Journal of General Surgery,2019,28(4):399-406.doi:10.7659/j.issn.1005-6947.2019.04.004.
[26]Snijders HS,Wouters MW,van Leersum NJ,et al.Meta-analysis of the risk for anastomotic leakage,the postoperative mortality caused by leakage in relation to the overall postoperative mortality[J].Eur J Surg Oncol,2012,38(11):1013-1019.doi:10.1016/j.ejso.2012.07.111.
[27]Takahashi H,Haraguchi N,Nishimura J,et al.The Severity of Anastomotic Leakage May Negatively Impact the Longterm Prognosis of Colorectal Cancer[J].Anticancer Res,2018,38(1):533-539.doi:10.21873/anticanres.12255.
[28]Guillou PJ,Quirke P,Thorpe H,et al.Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial):multicentre,randomised controlled trial[J].Lancet,2005,365(9472):1718-1726.doi:10.1016/S0140-6736(05)66545-2.
[29]Park JS,Choi GS,Kim SH,et al.Multicenter analysis of risk factors for anastomotic leakage after laparoscopic rectal cancer excision:the Korean laparoscopic colorectal surgery study group[J].Ann Surg,2013,257(4):665-671.doi:10.1097/SLA.0b013e31827b8ed9.
[30]Kawada K,Hasegawa S,Hida K,et al.Risk factors for anastomotic leakage after laparoscopic low anterior resection with DST anastomosis[J].Surg Endosc,2014,28(10):2988-2995.doi:10.1007/s00464-014-3564-0.
[31]Braunschmid T,Hartig N,Baumann L,et al.Influence of multiple stapler firings used for rectal division on colorectal anastomotic leak rate[J].Surg Endosc,2017,31(12):5318-5326.doi:10.1007/s00464-017-5611-0.
[32]童卫东,赖晓东.经肛门全直肠系膜切除术技术平台的建立与面临的问题[J].中华胃肠外科杂志,2015,18(5):430-432.doi:10.3760/cma.j.issn.1671-0274.2015.05.007.
Tong WD,Lai XD.Transanal total mesorectal excision:the operative platform and potential issues[J].Chinese Journal of Gastrointestinal Surgery,2015,18(5):430-432.doi:10.3760/cma.j.issn.1671-0274.2015.05.007.
[33]Lacy AM,Tasende MM,Delgado S,et al.Transanal Total Mesorectal Excision for Rectal Cancer:Outcomes after 140 Patients[J].J Am Coll Surg,2015,221(2):415-423.doi:10.1016/j.jamcollsurg.2015.03.046.
[34]Fernández-Hevia M,Delgado S,Castells A,et al.Transanal total mesorectal excision in rectal cancer:short-term outcomes in comparison with laparoscopic surgery[J].Ann Surg,2015,261(2):221-227.doi:10.1097/SLA.0000000000000865.
[35]Chen WH,Kang L,Luo SL,et al.Transanal total mesorectal excision assisted by single-port laparoscopic surgery for low rectal cancer[J].Tech Coloproctol,2015,19(9):527-534.doi:10.1007/s10151-015-1342-1.
