多形性未分化肉瘤(undifferentiated pleomorphic sarcoma,UPS),既往称为恶性纤维组织细胞瘤(malignant fibrous histiocytoma,MFH)是一种间叶源性恶性肿瘤,占所有软组织肉瘤的20%以上,多发生于四肢、躯干及腹膜后[1]。发生于胰腺的UPS极为罕见。国内、外虽有报道,但多以个案形式报道,缺少大宗病例资料进行分析。现就内蒙古医科大学附属医院肝胆外科收治的1例胰腺UPS并结合国内外文献以探讨其诊疗与预后。
1 资料与方法
1.1 病例资料
患者 男 42岁,既往体健,以“反复上腹部疼痛2月余”入院。入院辅助检查:肿瘤标记物:CEA 0.60 ng/mL,CA1-99 24.46 ng/mL,CA-125 7.00 ng/mL,入院时血红蛋白,凝血,生化,肝功正常。腹部增强CT(图1A):胰腺体部占位,考虑良性可能。上腹部MRI(图1B-C)提示:胰腺颈部可见一类圆形长T1、混杂T2信号影,DWI呈不均匀高信号影,大小约3.4 cm×3.1 cm,病变边界尚清,增强扫描:病变成轻度不均匀强化。主胰管通畅,未见扩张。
完善术前准备后于2018年3月13日行剖腹探查及肿瘤切除术,术中超声刀离断胃结肠韧带后,胰腺上方第17组淋巴结肿大,直径约为1.5 cm,完整切除后送病理。肠系膜上动脉 左侧胰腺中段实质可见肿物,直径约3.5 cm,胰腺肿物远侧胰腺实质质硬,考虑为胰腺炎所致,胰头处实质质软,未触及异常。距肿物近、远端1 cm处完整切除肿物后送快速冰冻切片2次 ,均考虑为交界性肿瘤,术中与家属沟通后,行胰腺中段切除术、胰肠双吻合术[2](图2) 。术后淋巴结石蜡切片及免疫组化显示:(第17组淋巴结)淋巴组织增生,部分结构有破坏。苏木精-伊红染色法(HE)(图3A)及免疫组化结果支持UPS诊断,并侵袭神经纤维。 考虑患者年轻、肿瘤恶性程度高,加之其他方式方法缺乏或效果不明确,与家属沟通后,加行手术区域扩大切除术。于术后1个月再次行胰体尾联合脾脏切除术,二次术后4个月因肿瘤复发转移死亡(图3B)。
1.2 文献回顾
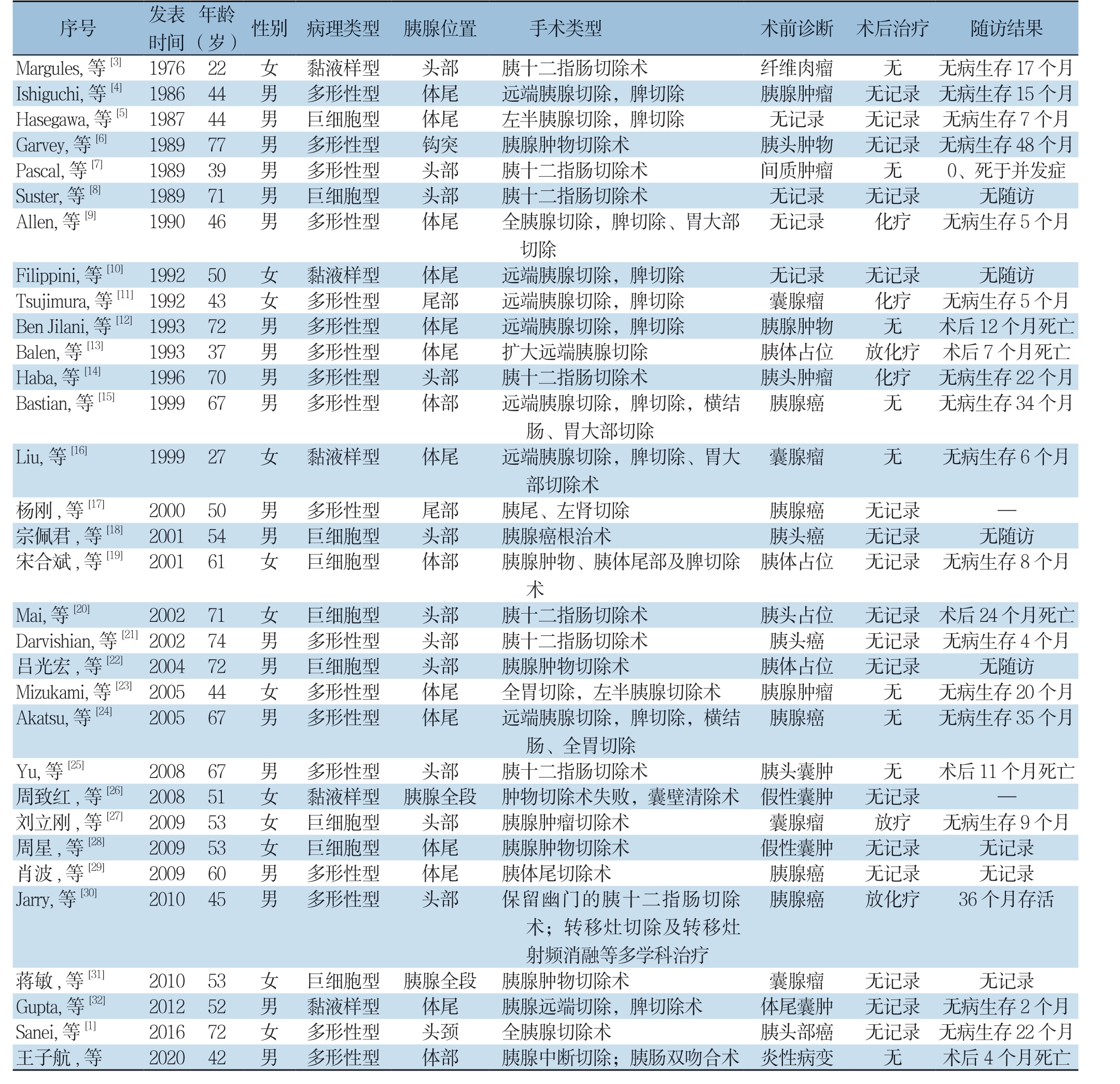
检索Pubmed、万方数据库,以“胰腺”、“恶性纤维组织细胞瘤或多形性未分化肉瘤”为检索词,经过查重,剩余31篇[1, 3-32]。其中男19例,女12例;中位年龄55.1岁,按病理类型分为:巨细胞型9例,黏液型5例,多形性型17例。按发生部位则分为:胰头1 3 例,胰体尾1 2 例,胰体2 例,胰尾2 例,全胰腺2 例(表1)。其临床表现大多表现为软组织肿块进行性增大,进展较快,常伴有压迫症状,可伴有恶心呕吐,上腹部不适、腹胀,体质量减轻;根据肿瘤的发生部位,可伴有黄疸。
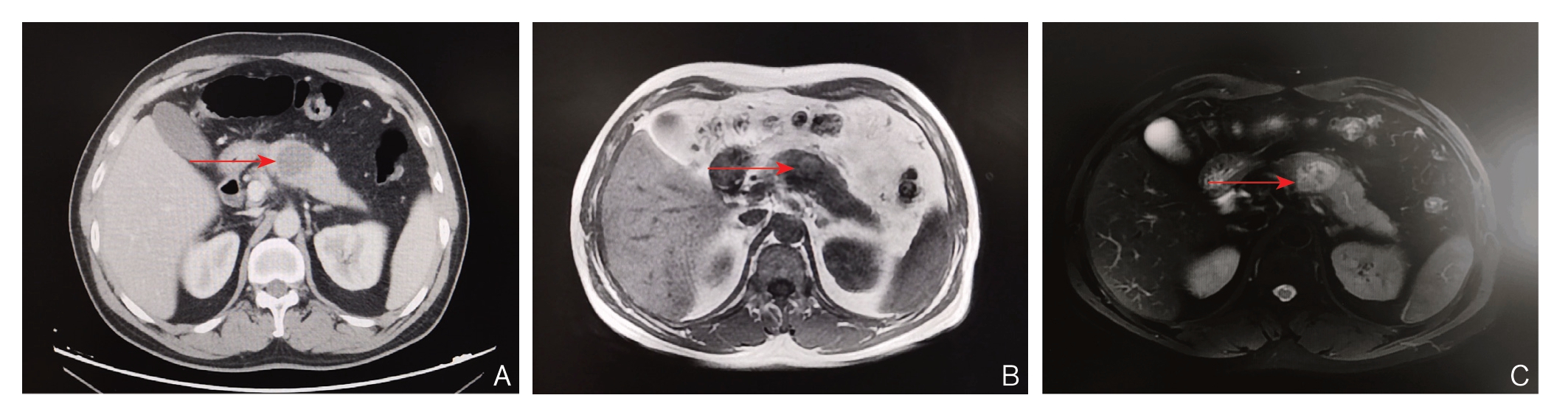
图1 术前影像学资料 A:上腹部CT 示胰腺体部占位,考虑良性可能(红色箭头示肿瘤位置);B:T1WI 可见胰颈部一类圆形病变,边界尚清(红色箭头示肿瘤位置);C:T2WI 可见胰颈部一类圆形病变,边界尚清,增强扫描呈不均匀强化的占位(红色箭头示肿瘤位置)
Figure 1 Preoperative imaging data A: Upper abdominal CT scan showing occupying lesion in the body of the pancreas, which considered to be a benign lesion (the red arrow showing the tumor); B: A round-like lesion in the neck of pancreas from T1WI, with a relatively clear boundary (the red arrow showing the tumor); C: A round-like lesion in the neck of pancreas from T2WI, with a relatively clear boundary, and heterogeneous enhancement displayed by the enhanced scanning (the red arrow showing the tumor)
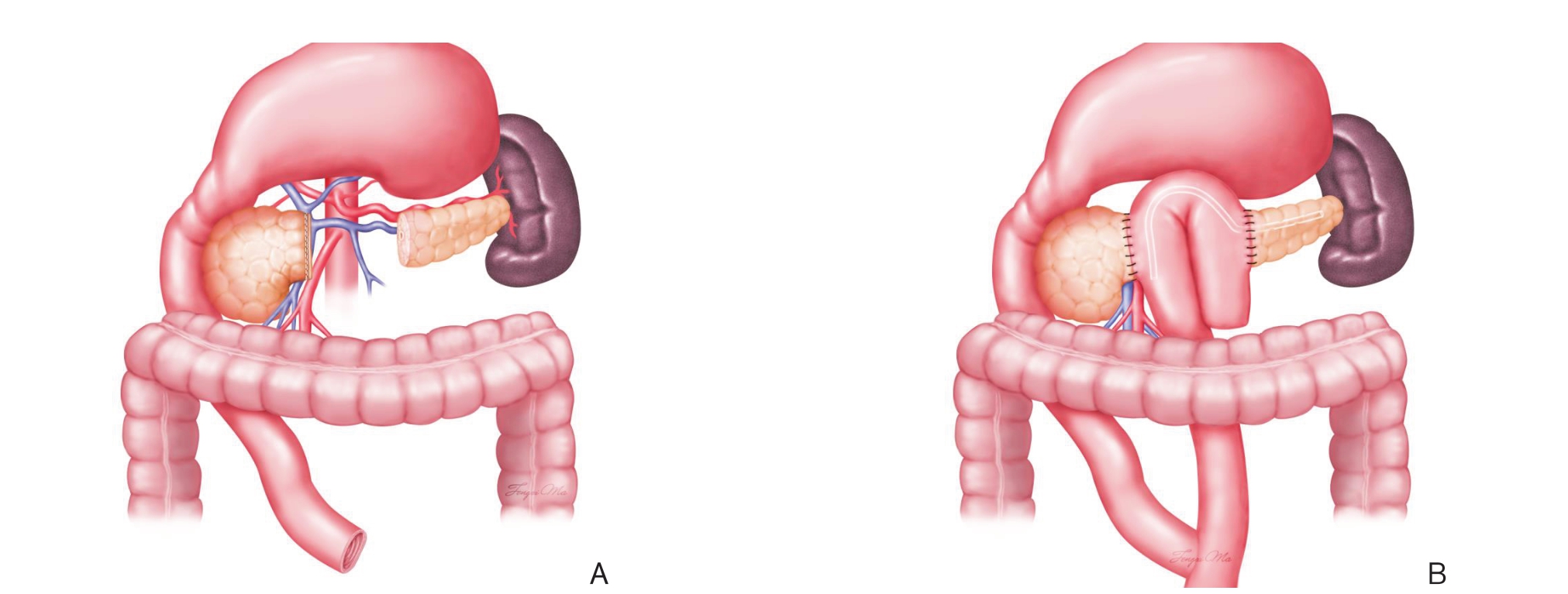
图2 手术方法示意图 A:胰腺中段切除术;B:胰肠双吻合术
Figure 2 Schematic pictures of the procedure A: Middle segment pancreatectomy; B: Side-to-side anastomosis of the jejunal loop with the remaining pancreatic head and pancreatic body
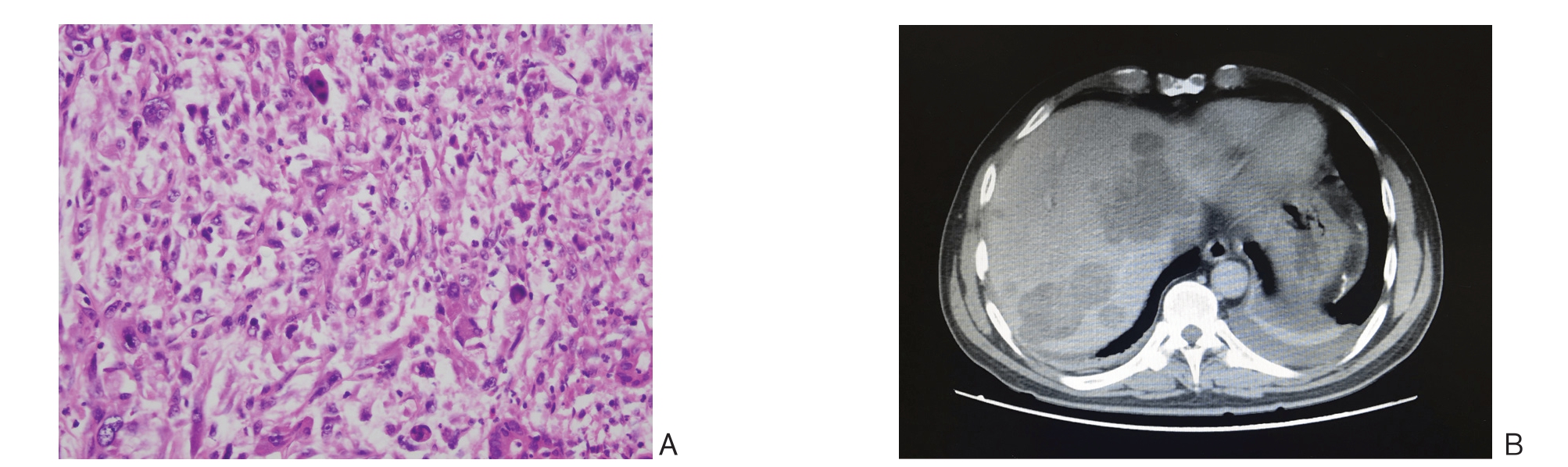
图3 术后资料 A:胰腺病理切片(HE×400);B:肝脏的多发转移瘤
Figure 3 Postoperative data A: Pathological section of pancreatic tissue (HE ×400); B: Multiple liver metastases
表1 32 例胰腺UPS 患者的临床资料
Table 1 Clinical data of the 32 patients with pancreatic UPS
M I H G P S A s u a h a l a a l s s r s i e r c t v g g e neaeu gu r,ly c a,序l,等 , e h w等 等s等i a号,, ,[等9等 [[8]等7[ ]6] ] [[34 []]5 ] 发时1 1 1 1 1 1 1 9 9 9 9 9 9 9表间7 8 8 8 8 8 9 6 6 7 9 9 9 0 (年岁2 4 4 7 3 7 4龄2 4 4 7 9 1 6) 性 女男男男男男男别 病 黏多巨多多巨多理 液形细形形细形类 样性胞性性胞性型 型型型型型型型 胰腺头体体钩头头体位 部尾尾突部部尾置 胰远左胰胰胰全 十端半腺十十胰手 二胰胰肿二二腺术 指腺腺物指指切类 肠切切切肠肠除型 切除除除切切, 除,,术除除脾 术脾脾 术术切 切切 除 除除 、 胃 大 部术 纤胰 胰间无 无无前 维腺 头质记 记记诊 肉肿 肿肿录 录录断 瘤瘤 物瘤 术 无无无 无后化无记记记无记治疗录录录 录 疗 无无 无 无无0 、病病 病病 病随死生生 生生 无生访于存存 存存 随存结并访1 1 47 5果7 5 8发 个个 个个 个症月 月月月 月F T B B H B i s e a aa l u n l s i b e p j t a i i nJ p a m,i,i n l 等n u a等,i n r,等a i等[,,[1 1 4等等3][] 1 5[1]0 [[1]1 21]] 1 1 1 1 1 1 9 9 9 9 9 9 9 9 9 9 9 9 2 2 3 3 6 9 5 4 7 3 7 6 0 3 2 7 0 7 女女男男男男 黏多多多多多液形形形形形样性性性性性型型型型型型 体尾体体头体尾部尾尾部部 远远远扩胰远切端端端大十端除胰胰胰远二胰腺腺腺端指腺切切切胰肠切除除除腺切除,,,切除,脾脾脾除术脾切切切 切除除除 除 ,横 结胰胰胰无囊 胰腺体头记腺 腺肿占肿录瘤 癌物位瘤 无放化化记 无化 无疗 疗录 疗 术 无无 无 术后 病病病 后生生无生1 72 存存随存 个个访 月2 3月5 2 4 个 死 死 个个月 亡亡 月月Liu,等[16] 1999 27 女 黏液样型 体尾 远端肠胰、腺胃切大除部,切脾除切除、胃大 囊腺瘤 无 无病生存6 个月杨宗宋刚佩合君斌, 等,, 等等[17] [[1189]] 2 2 20 0 00 0 00 1 1 5 5 60 4 1 男男女 多巨巨形细细性胞胞型型型 尾头体部部部 胰胰胰尾腺腺部、癌肿切左根物除肾治、术切术胰除 体 尾 部 及脾切除 胰胰胰体腺头占癌癌位 无无无记记记录录录 无病无生—随存访8 个月M D吕M A a k a i光zr a i v u,t i sk等 宏s uah,m i等[a,2 i 0 n等,] ,等 [2等4[] 2 2[2][ 32]1 ]2 2 2 2 2 0 0 0 0 0 0 0 0 0 0 2 2 4 5 5 7 7 7 4 6 1 4 2 4 7 女男男女男 巨多巨多多细形细形形胞性胞性性型型型型型 头头头体体部部部尾尾 胰胰胰全远十十腺胃端术二二肿切胰指指物除腺肠肠切,切切切除左除除除术半,术术 胰 脾腺 切 切除 除,术横 结 胰 胰胰胰 胰头 体腺头 腺占 占肿癌 癌位 位瘤 无无无记记记无无录录录 术 无无 无后 病病病 生生生无24存存 存随个 访2 3月4 0 5 个 死 个个月亡 月月Y周刘周肖J a u r致立星波r, y等,红刚 ,,等 等等[2,,5 ][等等3 [[022]89 ]] [[2267 ]] 2 2 2 2 2 2 0 0 0 0 0 0 0 0 0 0 0 1 8 8 9 9 9 0 6 5 5 5 6 4 7 1 3 3 0 5 男女女女男男 多黏巨巨多多形液细细形形性样胞胞性性型型型型型型 胰头腺头体体头部全部尾尾部段 胰肿胰胰胰保十物腺腺体留肠二切肿肿尾幽、指除瘤物切门全肠术切切除胃的切失除除术切胰除败术术 除十术, 二囊 指壁 肠清切除术除 胰假 假囊 胰胰头性 性腺 腺腺囊囊 囊瘤 癌癌肿肿 肿 无 无无放放无记 记记化疗录 录录疗 术 无后3病6 生无无1个1 —存记记月个 录录存月9 个活死 月亡术;转移灶切除及转移灶蒋G S a u n敏p et ia,,, 等等等[1[[33] 12]] 2 2 20 0 01 1 10 2 6 5 5 73 2 2 女男女 巨黏多细液形胞样性型型型 胰腺体头全尾颈段 胰胰全腺腺胰射肿远腺频物端切消切切除融除除术等术, 多脾 学 切 科除治术疗 体胰囊尾头腺囊部瘤肿癌 无无无记记记录录录 无 无病病生无生存记存录22 2 个 个月月王子航, 等 2020 42 男 多形性型 体部 胰腺中断切除;胰肠双吻合术 炎性病变 无 术后4 个月死亡
2 讨 论
UPS曾被称为MFH,指具有席纹状或车辐状排列生长方式的、由组织细胞分化而来的一组软组织肿瘤[33]。发生在胰腺上的UPS罕见。正如前言所述,大多以个案报道形式展现,通过检索权威数据库,加上我院病例共有32例,其起源、发病机制至今不明,相信随着病例数积累,会逐渐揭开UPS的神秘面纱。
原发于胰腺的UPS病理特征与机体其他部位的UPS的相同。大多数病例多以多形性肿瘤为主,以细胞学和细胞核多形性为特征。其中多形性,纤维母细胞,组织细胞样细胞和异型巨细胞以不同比例混合存在[3 0]。2 0 0 2 世界卫生组织将M F H在病理学上分为3类:⑴ 多形性型;⑵ 炎性型;⑶ 巨细胞型,并将黏液样型从中剔除[34]。本组数据显示,多形性型18例(56%),巨细胞型9例(28%),黏液样型5例(16%)。胰腺UPS临床表现多样,无特异性,这已在发表的文献里得到支持。影像学检查尤其是腹部CT检查和腹部MRI的检查有助于肿块的定位,其他检查如B超、X线等应用受限,纵观文献报道,结合本院病例,影像学表现是无特征性的,影响疾病的正确诊断,32例患者中术前无1例考虑胰腺UPS。我院腹部增强CT:胰腺体部占位,考虑良性。上腹部MRI提示:考虑胰颈部囊腺瘤。而文献回顾每一个病例都有个各自的影像学特点。所以,胰腺UPS在没有获取组织前诊断较为困难,这也可能和其他成分复杂、比例不同有关。
病理组织学检查仍是确诊该病的金标准,B超引导下穿刺活检术可提高术前诊断的准确性[35]。但为防止肿瘤的扩散和针头植入,不建议常规进行术前活检。对于不能手术,需要放疗或化疗的患者,可进行穿刺行病理学检查[36] 。免疫组织化学检查主要作用是帮助排除其他常见肉瘤。主要与原发于胰腺的UPS相做鉴别[24, 35, 37-38]:⑴ 脂肪肉瘤;⑵ 平滑肌肉瘤;⑶ 神经母细胞瘤。上述的肿瘤均有特异性的标志物,可以通过免疫组化相作鉴别。对于免疫组化有必要指出的是,波形蛋白(vimentin)为间叶细胞的肿瘤标记物,而组织细胞性标志物(如a1-AT、lysozyme、CD68)对UPS诊断帮助意义则不大[35]。然而陈涛等[39]在报道指出了,对于波形蛋白及巨噬细胞(CD68)则是诊断UPS的极为重要的标志物,结合我院该患者免疫组化波形蛋白(弥漫3+)及CD68均显示为阳性,也支持陈等的观点。
国内外对于手术切除方式、术后是否进行放化疗及放化疗的疗效如何也未有相关的报道。有研究[40]认为:UPS属于软组织肉瘤,其具有局部浸润性生长、容易复发、区域淋巴结和血行转移相对较少的独特生物学行为,而在胰腺原发UPS可遵循软组织肉瘤的治疗原则,但我们从现有的病例发现,胰腺UPS可能恶性程度更高于其他部位的,这可能与胰腺本身环境有关。现有病例生存期最短4个月,是来自笔者单位患者,该患者生存时间较短的原因,笔者考虑由于以下几点因素造成:⑴ 未在术前行内镜超声引导穿刺病检,肿瘤型不类明确;⑵ 术中肿瘤的肉眼观及冰冻结果无法准确辨别肿瘤类型;⑶ 首次手术不彻底,未进行根治性切除;⑷ 二次手术前未进行详细的评估是否全身治疗或多学科讨论。手术选择的方式根据肿物所在的位置而定,位于胰头部选择胰腺十二指肠切除,位于胰体尾部选择胰体尾联合脾脏切除,全胰腺都有应选择全胰切除。笔者角度,不建议肿物局部切除,早期、完整切除,对于非胰头肿瘤以获得R 0切除应是手术治疗的核心。笔者资料中首先采取胰腺中段切除,初衷是考虑患者年轻,保留胰腺功能,加之术前影像学检查、术中2次冷冻快速病检报告支持良性或者低度恶性诊断,故行使胰腺中段切除、胰肠双吻合术。术后石蜡切片、免疫组化确诊时,患者再次手术已然发生转移,给我们留下了过多思考。
对于胰腺UPS治疗,关键在于早期发现,及时治疗。除手术外,有文献报道采用放疗可能对胰腺UPS有一定的疗效,刘立刚等[27]为1例术后患者行放疗,随访周期内未见肿瘤复发。在其他部位发生UPS,有研究[41]发现,无法完整切除肿瘤或者是无法取得切缘阴性的情况下,放疗则是一种重要的辅助治疗手段。放疗也是具有高危复发因素软组织肉瘤有效的辅助治疗手段,可降低肿瘤的局部复发率[42],但由于目前胰腺UPS术后放疗例数非常有限,其他部位UPS治疗是否适用胰腺,尚缺乏大样本数据支持。对于已经转移的胰腺UPS,术后化疗因病例数少加之随访周期短,其效果亦不明确。在其他软组织肉瘤综合治疗方面,术后给予化疗的患者术后生存时间较未化疗的患者普遍延长,并且对于此类患者的化疗方案上查阅文献后,大多数将多柔比星及异环磷酰胺作为一线用药[27, 33, 40, 43],而在胰腺UPS应采取何方案,已有的文献来看,均在探索与尝试。Jarry等[30]在文章中所提患者在第1次手术后11个月发生肝和肺转移,患者接受了化疗、放疗和右肝切除联合术中射频消融术的多学科治疗。在多学科治疗下,患者完全康复,并在术后25个月内保持无病状态,然仅为个案报道。来自其他临床报道并未显示明显优势[9, 11, 13]。
总之,胰腺UPS为高度恶性肿瘤,无明显特异性临床表现,极易发生转移及复发,预后差。完整手术切除治疗为目前最有效的治疗手段,术后给予放化疗可能能够改善患者的生存周期,尚需临床进一步验证。
[1] Sanei B, Kefayat A, Samadi M, et al.Undifferentiated Pleomorphic Sarcoma of Pancreas: A Case Report and Review of the Literature for the Last Updates[J].Case Rep Med, 2018, 2018:1510759.doi:10.1155/2018/1510759.
[2] 孟兴凯, 王慧君, 田全发, 等.胰肠双吻合预防胰腺中段切除术后胰瘘发生的初步研究[J].中华内分泌外科杂志, 2019, 13(6):488-491.doi:10.3760/cma.j.issn.1674-6090.2019.06.010.Meng XK, Wang HJ, Tian QF, et al.Preliminary study of double pancreaticojejunostomy for prevention of pancreatic fistulas after central pancreatectomy[J].Journal of Endocrine Surgery, 2019,13(6):488-491.doi:10.3760/cma.j.issn.1674-6090.2019.06.010.
[3] Margules RM, Allen RE, Dunphy JE.Pancreatic Tumor of Mesenchymal Origin Presenting as Obstructive Jaundice[J].Am J Surg, 1976, 131(3):357-359.doi: 10.1016/0002-9610(76)90131-8.
[4] Ishiguchi T, Shimamoto K, Kaii O, et al.Malignant fibrous histiocytoma of the pancreas[J].Rinsho Hoshasen, 1986, 31(5):655-658.
[5] Hasegawa S, Kawachi H, Kurosawa H, et al.Malignant fibrous histiocytoma in the ileum associated with intussusception[J].Dig Dis Sci, 2004, 49(7/8):1156-1160.doi: 10.1023/b:ddas.0000037804.91628.8d.
[6] Garvey JF, Ng A, England JF, et al.Malignant fibrous histiocytoma of the pancreas[J].HPB Surgery, 1989, 1(3):233-237.doi:10.1155/1989/60313.
[7] Pascal RR, Sullivan L, Hauser L, et al.Primary malignant fibrous histiocytoma of the pancreas[J].Hum Pathol, 1989, 20(12):1215-1217.doi: 10.1016/s0046-8177(89)80015-2.
[8] Suster S, Phillips M, Robinson MJ.Malignant fibrous histiocytoma(giant cell type) of the pancreas.A distinctive variant of osteoclasttype giant cell tumor of the pancreas[J].Cancer, 1989, 64(11):2303-2308.doi: 10.1002/1097-0142(19891201)64:11<2303::aidcncr2820641120>3.0.co;2-s.
[9] Allen KB, Skandalakis LJ, Brown BC, et al.Malignant fibrous histiocytoma of the pancreas[J].Am Surg, 1990, 56(6):364-368.
[10] Filippini A, Lucci S, Berni A, et al.Malignant fibrous histiocytoma of the pancreas[J].G Chir, 1992, 13(10):485-488.
[11] Tsujimura T, Kawano K, Taniguchi M, et al.Malignant fibrous histiocytoma coexistent with mucinous cystadenoma of the pancreas[J].Cancer, 1992, 70(12):2792-2796.doi: 10.1002/1097-0142(19921215)70:12<2792::aidcncr2820701211>3.0.co;2-n.
[12] Ben Jilani S, el Mezni F, Dziri C, et al.Primary malignant histiocytofibroma of the pancreas.Apropos of a case[J].Arch Anat Cytol Pathol, 1993, 41(3-4):167-170.
[13] Balén EM, De Villa VH, Cienfuegos JA, et al.Malignant fibrous histiocytoma of the pancreas[J].Rev Esp Enferm Dig, 1993,83(6):475-480.
[14] Haba R, Kobayashi S, Hirakawa E, et al.Malignant fibrous histiocytoma of the pancreas[J].Pathol Int, 1996, 46(7):515-519.doi: 10.1111/j.1440-1827.1996.tb03647.x.
[15] Bastian D, Ramaswamy A, Barth PJ, et al.Malignant fibrous histiocytoma of the pancreas: a case report with genetic analysis[J].Cancer, 1999, 85(11):2352-2358.doi: 10.1002/(sici)1097-0142(19990601)85:11<2352::aid-cncr9>3.0.co;2-7.
[16] Liu DM, Jeffrey RB Jr, Mindelzun RE.Malignant fibrous histiocytoma presenting as cystic pancreatic mass[J].Abdom Imaging, 1999, 24(3):299-300.doi: 10.1007/s002619900500.
[17] 杨刚.酷似胰腺癌的恶性纤维组织细胞瘤1例[J].现代医用影像学, 2000, 9(6):284-285.Yang G.Malignant fibrous histiocytoma extremely similar to pancreatic cancer in one case[J].Modern Medical Imagelogy, 2000,9(6):284-285.
[18] 宗佩君, 刘爱珍.胰腺恶性纤维组织细胞瘤一例[J].中华普通外科杂志, 2001, 16(6):380.doi:10.3760/j.issn:1007-631X.2001.06.038.Zong PJ, Liu AZ.Malignant fibrous histiocytoma of the pancreas:a report of one case[J].Zhong Hua Pu Tong Wai Ke Za Zhi, 2001,16(6):380.doi:10.3760/j.issn:1007-631X.2001.06.038.
[19] 宋合斌, 郭丽娜, 刘彤华.胰腺多房性粘液性囊腺瘤癌变合并巨细胞型恶性纤维组织细胞瘤一例[J].中华病理学杂志, 2001,30(4):311-312.doi:10.3760/j.issn:0529-5807.2001.04.029.Song HB, Guo LN, Liu TH.Canceration of multiloculated mucinous cystadenoma of the pancreas with concomitant malignant fibrous himocytorna in one case[J].Chinese Journal of Pathology,2001, 30(4):311-312.doi:10.3760/j.issn:0529-5807.2001.04.029.
[20] Mai G, Baer HU, Mittler M, et al.Malignant fibrous histiocytoma of the pancreas[J].Pancreas, 2002, 25(3):320-324.doi:10.1097/00006676-200210000-00018.
[21] Darvishian F, Sullivan J, Teichberg S, et al.Carcinosarcoma of the pancreas: a case report and review of the literature[J].Arch Pathol Lab Med, 2002, 126(9):1114-1117.doi:10.1043/0003-9985(2002)126<1114:COTP>2.0.CO;2.
[22] 吕光宏, 潘江峰, 董科, 等.胰腺恶性纤维组织细胞瘤一例[J].临床放射学杂志, 2004, 23(1):85.doi:10.3969/j.issn.1001-9324.2004.01.035.Lu GH, Pan JF, Dong K, et al.Malignant fibrous histiocytoma of the pancreas in one case[J].Journal of Clinical Radiology, 2004,23(1):85.doi:10.3969/j.issn.1001-9324.2004.01.035.
[23] Mizukami H, Yajima N, Wada R, et al.Pancreatic malignant fibrous histiocytoma, inflammatory myofibroblastic tumor, and inflammatory pseudotumor related to autoimmune pancreatitis:characterization and differential diagnosis[J].Virchows Arch, 2006,448(5):552-560.doi: 10.1007/s00428-006-0157-x.
[24] Akatsu T, Tsugita M, Ro S, et al.Primary malignant fibrous histiocytoma of the pancreas: a case with K-ras mutation and a review of the literature[J].Dig Dis Sci, 2005, 50(12):2214-2217.doi: 10.1007/s10620-005-3037-3.
[25] Yu RS, Wang JW, Chen Y, et al.A case of primary malignant fibrous histiocytoma of the pancreas: CT and MRI findings[J].World J Gastroenterol, 2008, 14(18):2942-2945.doi: 10.3748/wjg.14.2942.
[26] 周致红, 曲金龙.胰腺假性囊肿内引流术后胰腺囊肿恶性纤维组织细胞瘤1例[J].中国普通外科杂志, 2008, 17(7):705-705.doi:10.3969/j.issn.1005-6947.2008.07.034.Zhou ZH, Qu JL.Malignant fibrous histiocytoma following internal drainage of the pancreatic pseudocyst: a report of one case[J].Chinese Journal of General Surgery, 2008, 17(7):705-705.doi:10.3969/j.issn.1005-6947.2008.07.034.
[27] 刘立刚, 何晓东, 李玉民, 等.胰腺恶性纤维组织细胞瘤的诊治(附1例报道并文献复习)[J].中国普外基础与临床杂志, 2009,16(8):658-660.Liu LG, He XD, Li YM, et al.Diagnosis and Treatment of Pancreatic Malignant Fibrous Histiocytoma (with a Case Report and Literature Review)[J].Chinese Journal of General Surgery, 2009,16 (8): 658-660.
[28] 周星, 张皓, 周怀琪, 等.胰腺恶性纤维组织细胞瘤1例[J].中国临床医学影像杂志, 2009, 20(6):500-501.doi:10.3969/j.issn.1008-1062.2009.06.034.Zhou X, Zhang H, Zhou HQ, et al.Primary malignant fibrous histiocytoma of the pancreas: report of one case[J].Journal of China Clinic Medical Imaging, 2009, 20(6):500-501.doi:10.3969/j.issn.1008-1062.2009.06.034.
[29] 肖波, 张小明, 曾南林, 等.胰腺原发性恶性纤维组织细胞瘤1例[J].中国医学影像技术, 2009, 25(8):1511.doi:10.3321/j.issn:1003-3289.2009.08.071.Xiao B, Zhang XM, Zeng NL, et al.Primary malignant fibrous histiocytoma of pancreas: case report[J].Chinese Journal Of Medical Imaging Technology, 2009, 25(8):1511.doi:10.3321/j.issn:1003-3289.2009.08.071.
[30] Jarry J, Belleannee G, Laurent C, et al.Primary Malignant Fibrous Histiocytoma, of the Pancreas: Benefit of the Multidisciplinary Approach[J].European Journal of Gastroenterology & Hepatology,2010, 22(6):765-768.
[31] 蒋敏, 朱骏, 王晓梅, 等.胰腺未分化多形性肉瘤临床病理观察[J].甘肃科技, 2010, 26(9):143-145.doi:10.3969/j.issn.1000-0952.2010.09.052.Jiang M, Zhu J, Wang XM, et al.Clinicopathologic Observation of Undifferentiated Pleomorphic Sarcoma with Giant Cell in Pancreas[J].Gansu Science and Technology, 2010, 26(9):143-145.doi:10.3969/j.issn.1000-0952.2010.09.052.
[32] Gupta P, Behari A, Jain M.A Case of Primary Myxoid Malignant Fibrous Histiocytoma of the Pancreas: Clinical, Histopathology, and Immunohistochemistry Findings[J].J Gastrointest Cancer, 2012,43(Suppl 1):S16-19.doi: 10.1007/s12029-011-9293-x.
[33] Brennan MF, Antonescu CR, Maki RG, et al.Undifferentiated Pleomorphic Sarcoma (UPS) (Malignant Fibrous Histiocytoma(MFH) and Myxofibrosarcoma)[A]//Management of Soft Tissue Sarcoma[M].Springer, 2016:129-136.doi: 10.1007/978-1-4614-5004-7_7.
[34] Fletcher CD.The evolving classification of soft tissue tumoursan update based on the new 2013 WHO classification[J].Histopathology, 2014, 64(1):2-11.doi: 10.1111/his.12267.
[35] 杨小秋, 谈顺.多形性未分化肉瘤的临床病理诊断及分子病理学进展[J].医学综述, 2015, 21(15):2741-2744.doi:10.3969/j.issn.1006-2084.2015.15.019.Yang XQ, Tan S.The Clinical Pathological Diagnosis and Molecular Pathology of Undifferentiated Pleomorphic Sarco-ma[J].Medical Recapitulate, 2015, 21(15):2741-2744.doi:10.3969/j.issn.1006-2084.2015.15.019.
[36] 蒋超, 刘雪岩, 孙大伟, 等.巨大腹膜后平滑肌肉瘤伴出血1例报告并文献复习[J].中国普通外科杂志, 2019, 28(6):737-742.doi:10.7659/j.issn.1005-6947.2019.06.014.Jiang C, Liu XY, Sun DW, et al.Huge retroperitoneal leiomyosarcoma with hemorrhage:an analysis of one case and literature review[J].Chinese Journal of General Surgery, 2019,28(6):737-742.doi:10.7659/j.issn.1005-6947.2019.06.014.
[37] Coindre JM, Mariani O, Chibon F, et al.Most malignant fibrous histiocytomas developed in the retroperitoneum are dedifferentiated liposarcomas: a review of 25 cases initially diagnosed as malignant fibrous histiocytoma[J].Mod Pathol, 2003, 16(3):256-262.doi:10.1097/01.MP.0000056983.78547.77.
[38] Wardelmann E, Schildhaus HU, Merkelbachbruse S, et al.Soft tissue sarcoma: from molecular diagnosis to selection of treatment.Pathological diagnosis of soft tissue sarcoma amid molecular biology and targeted therapies[J].Ann Oncol, 2010, 21(Suppl 7):vii265-269.doi: 10.1093/annonc/mdq381.
[39] 陈涛, 严静东, 雷贞妮.未分化多形性肉瘤的影像诊断与鉴别51例[J].实用医学杂志, 2016, 32(5):789-792.doi:10.3969/j.issn.1006-5725.2016.05.031.Chen T, Yan JD, Lei ZN.Imaging diagnosis and identification of undifferentiated pleomorphic sarcoma: a report of 51 cases[J].The Journal of Practical Medicine, 2016, 32(5):789-792.doi:10.3969/j.issn.1006-5725.2016.05.031.
[40] 石远凯, 郏博.软组织肉瘤治疗进展[J].中国肿瘤临床, 2014,41(24):1556-1560.doi:10.3969/j.issn.1000-8179.20141668.Shi YK, Jia B.Advances in therapy of sarcoma of soft tissue[J].Chinese Journal of Clinical Oncology, 2014, 41(24):1556-1560.doi:10.3969/j.issn.1000-8179.20141668.
[41] Sheplan LJ, Juliano JJ.Use of radiation therapy for patients with soft-tissue and bone sarcomas [J].Cleve Clin J Med, 2010, 77(Suppl 1): S27-29.doi: 10.3949/ccjm.77.s1.06.
[42] 杨婧, 王征, 孔琳, 等.软组织肉瘤的放射治疗:临床实践及进展[J].中国临床医学, 2019, 26(3):326-331.doi:10.12025/j.issn.1008-6358.2019.20190636.Yang J, Wang Z, Kong L, et al.Radiotherapy for soft-tissue sarcoma :clinical practice and progress[J].Chinese Journal of Clinical Medicine, 2019, 26(3):326-331.doi:10.12025/j.issn.1008-6358.2019.20190636.
[43] 高天, 樊征夫, 方志伟.软组织肉瘤分子靶向治疗研究进展[J].中国肿瘤临床, 2017, 44(1):7-13.doi:10.3969/j.issn.1000-8179.2017.01.107.Gao T, Fan ZF, Fang ZW.Advances in molecular targeted therapy for soft tissue sarcomas[J].Chinese Journal of Clinical Oncology,2017, 44(1):7-13.doi:10.3969/j.issn.1000-8179.2017.01.107.
