胰腺癌主要是原发于胰腺的一种恶性肿瘤,近年来其发病率呈不断上升趋势,严重威胁人类健 康[1-3]。胰头癌是最常见的一种胰头癌类型,占胰腺恶性肿瘤的70%~80%,具有不易早期发现、发展迅速及恶性程度高等特点,导致其预后不良[4-5]。目前,手术仍为治疗胰头癌主要治疗手段,其中胰十二指肠切除术(pancreaticoduodenectomy,PD)是最有效的治疗方法。尽管近年来PD术的围手术期病死率已经显著降低,但术后并发症发生率高、患者恢复情况较差、术后住院时间长仍是困扰外科医生的重要问题[6-8]。加速康复外科(enhanced recovery after surgery,ERAS)理念近年来在多种外科领域应用,可降低术后并发症,促进术后恢复[9-10]。因此,本文研究探讨ERAS对胰头癌行PD术患者术后恢复及效果的影响,从而评价其临床应用价值。
1 资料与方法
1.1 一般资料
选择我院于2015年5月—2019年5月期间行PD术的胰头癌患者62例。纳入标准:(1) 术前经增强CT或MRI检查证实为胰头占位,且术后病理证实为胰头癌;(2) 术前评估肿瘤可根治性切除术,且患者均行PD;(3)术前未接受过放疗、化疗等手术治疗;(4) 获得知情同意,签署知情同意书。排除标准:(1) 肿瘤存在远处转移;(2) 合并其他恶性肿瘤者;(3)严重营养不良者;(4) 合并心肺、肝肾功能严重异常者;(5) 精神疾病者;⑹ 手术或麻醉禁忌者。采用随机数字表法随机分为ERAS组31例与对照组31例。ERAS组31例中,男22例,女9例;年龄38~71岁,平均年龄(54.38± 6.57)岁;平均肿瘤直径(3.51±0.65)cm;合并基础疾病:高血压4例,糖尿病2例,冠心病 2例。对照组31例中,男21例,女10例;年龄41~70岁,平均年龄(55.61±5.89)岁;平均肿瘤直径(3.48±0.51)cm;合并基础疾病:高血压5例,糖尿病3例,冠心病1例。两组患者一般资料比较差异无统计学意义(均P>0.05)。
1.2 方法
两组患者均行PD治疗,ERAS组患者围手术期采用ERAS为指导的系统有序地干预措施,对照组患者则采用传统的围手术期管理方案。两组患者具体围术期处理方法见表1。
表1 ERAS 组与对照组围术期处理方法
Table 1 Perioperative management methods in ERAS group and control group
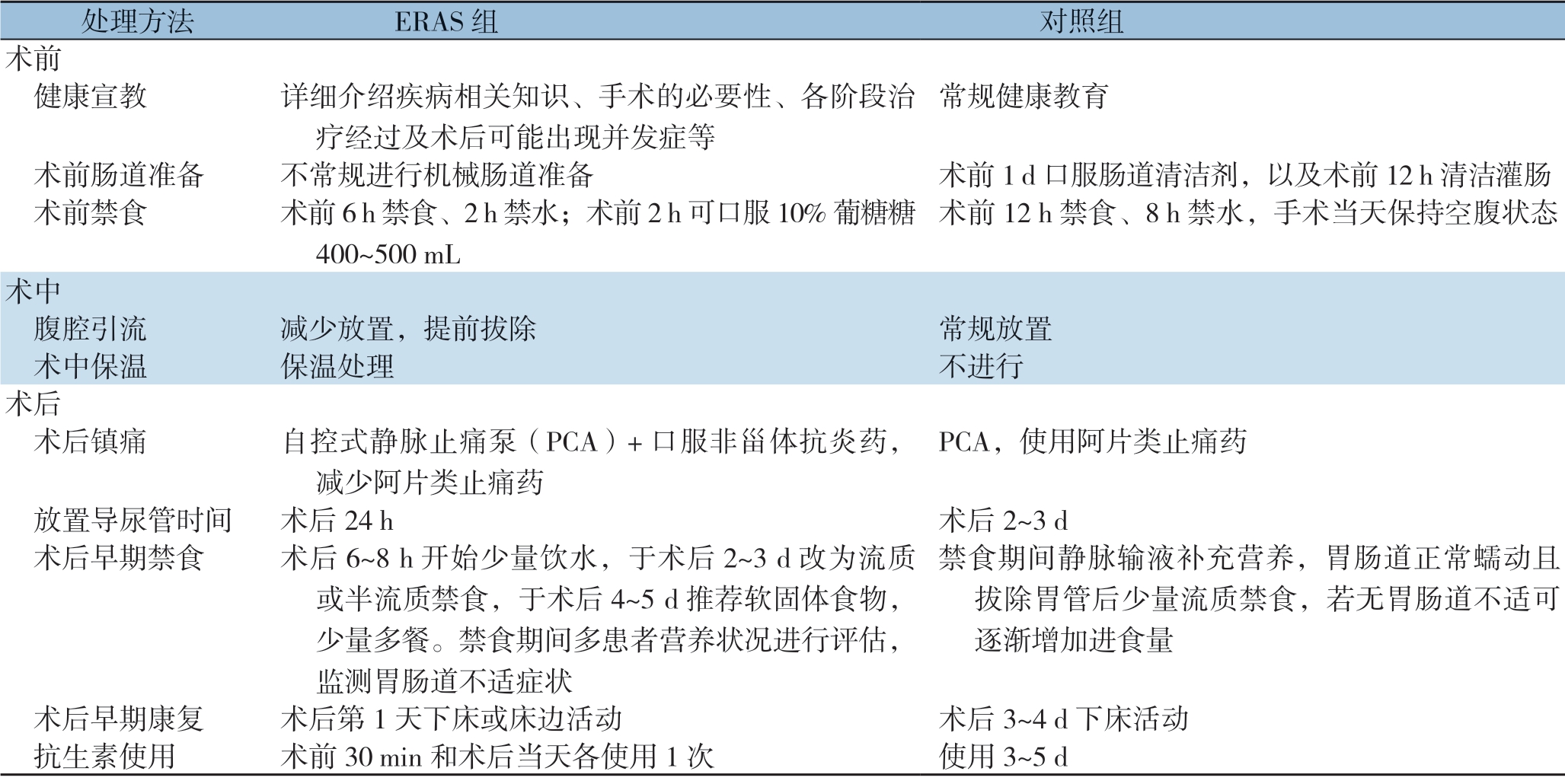
处理方法 ERAS 组 对照组术前 健康宣教 详细介绍疾病相关知识、手术的必要性、各阶段治疗经过及术后可能出现并发症等常规健康教育 术前肠道准备 不常规进行机械肠道准备 术前1 d 口服肠道清洁剂,以及术前12 h 清洁灌肠 术前禁食 术前6 h 禁食、2 h 禁水;术前2 h 可口服10%葡糖糖400~500 mL术前12 h 禁食、8 h 禁水,手术当天保持空腹状态术中 腹腔引流 减少放置,提前拔除 常规放置 术中保温 保温处理 不进行术后 术后镇痛 自控式静脉止痛泵(PCA)+口服非甾体抗炎药,减少阿片类止痛药PCA,使用阿片类止痛药 放置导尿管时间 术后24 h 术后2~3 d 术后早期禁食 术后6~8 h 开始少量饮水,于术后2~3 d 改为流质或半流质禁食,于术后4~5 d 推荐软固体食物,少量多餐。禁食期间多患者营养状况进行评估,监测胃肠道不适症状禁食期间静脉输液补充营养,胃肠道正常蠕动且拔除胃管后少量流质禁食,若无胃肠道不适可逐渐增加进食量 术后早期康复 术后第1 天下床或床边活动 术后3~4 d 下床活动 抗生素使用 术前30 min 和术后当天各使用1 次 使用3~5 d
1.3 观察指标
观察两组术中指标变化,包括术中失血量、术中输液量和手术时间;观察两组术后恢复指标变化,包括首次肛门排气时间、排便时间和下床活动时间;观察两组术后并发症发生情况;观察两组术前1 d和术后3 d营养状况指标变化,包括转铁蛋白(TRE)、前清蛋白(PAB)和白蛋白(ALB)(于术前1 d和术后3 d分别抽取肘静脉血,以离心半径10 cm,离心10 min,分离血清,于-20 ℃下保存待测,采用免疫比浊法测定TRE、PAB和ALB含量)。
1.4 统计学处理
应用SPSS 19.0统计软件处理。正态分布的计量资料采用均数±标准差( ±s)表示,组间比较采用t检验;计数资料采用例数(百分比)[n(%)]表示,组间比较采用χ2检验。P<0.05为差异有统计学意义。
±s)表示,组间比较采用t检验;计数资料采用例数(百分比)[n(%)]表示,组间比较采用χ2检验。P<0.05为差异有统计学意义。
2 结 果
2.1 两组术中指标比较
ERAS组术中失血量为(273.14±45.62)mL,术中输液量(1612.32±238.98)mL,手术时间(297.49±37.51)min;对照组术中失血量为(291.53±68.1 8)m L,术中输液量 (1639.87±374.25)mL,手术时间(307.84±32.14)min。两组术中失血量、术中输液量和手术时间比较差异均统计学意义(均P >0.0 5) (表2)。
表2 两组术中指标比较(n=31, ±s)
±s)
Table 2 Comparison of intraoperative index between the two groups (n=31,  ±s)
±s)
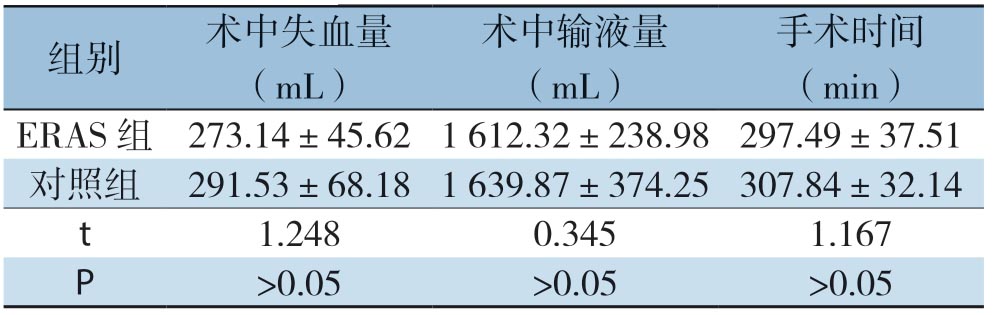
组别 术中失血量(mL)术中输液量(mL)手术时间(min)ERAS 组 273.14±45.62 1 612.32±238.98 297.49±37.51对照组 291.53±68.18 1 639.87±374.25 307.84±32.14 t 1.248 0.345 1.167 P >0.05 >0.05 >0.05
2.2 两组术后恢复指标比较
ERAS组首次肛门排气时间(2.93±0.53)d,首次肛门排便时间(4.2 1±0.8 9)d,下床活动时间(2.6 3±0.6 5)d;对照组首次肛门排气时间(5.1 3±1.2 9)d,首次肛门排便时间(6.10±1.32)d,下床活动时间(5.78±1.26)d。ERAS组首次肛门排气时间、首次肛门排便时间和下床活动时间均明显优于对照组 (均<0.05)(表3)。
2.3 两组术后并发症比较
ERAS组术后出现胰漏1例,吻合口瘘1例;对照组术后出现胰漏4例,感染2例,吻合口瘘 2例,胃排空延迟2例。两组并发症的发生率均无统计学差异(均P>0.05),但术后总并发症的发生率ERAS组低于对照组(6.45% vs.32.26%,P<0.05)(表4)。
表3 两组术后恢复指标比较(n=31, ±s)
±s)
Table 3 Comparison of postoperative recovery parameters between the two groups (n=31, ±s)
±s)
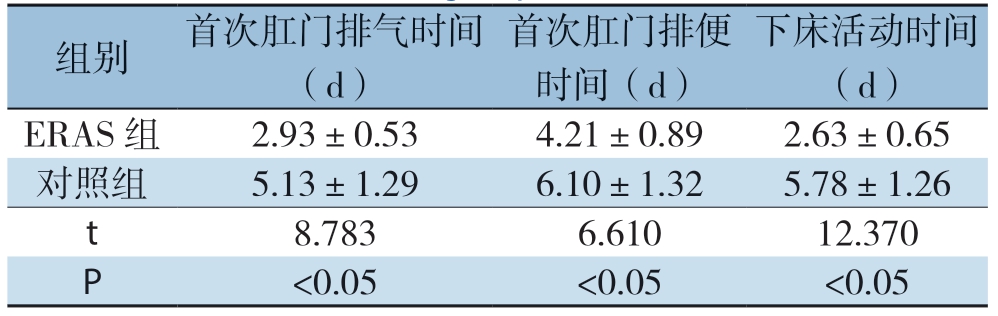
组别 首次肛门排气时间(d)首次肛门排便时间(d)下床活动时间(d)ERAS 组 2.93±0.53 4.21±0.89 2.63±0.65对照组 5.13±1.29 6.10±1.32 5.78±1.26 t 8.783 6.610 12.370 P <0.05 <0.05 <0.05
表4 两组术后并发症比较[n=31,n(%)]
Table 4 Comparison of postoperative complications between the two groups [n=31, n (%)]
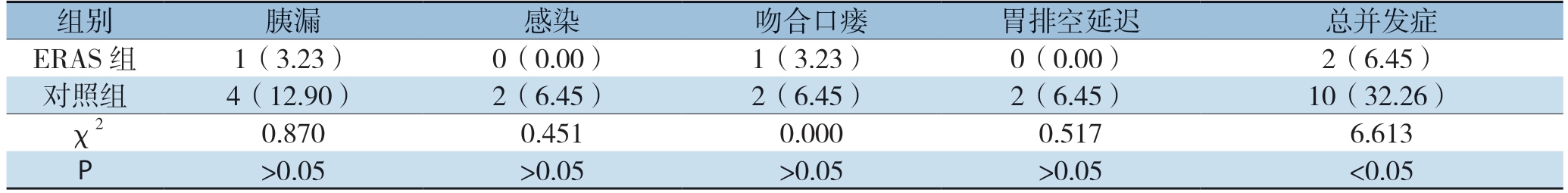
组别 胰漏 感染 吻合口瘘 胃排空延迟 总并发症ERAS 组 1(3.23) 0(0.00) 1(3.23) 0(0.00) 2(6.45)对照组 4(12.90) 2(6.45) 2(6.45) 2(6.45) 10(32.26)χ2 0.870 0.451 0.000 0.517 6.613 P >0.05 >0.05 >0.05 >0.05 <0.05
2.4 两组营养状况指标变化比较
两组术前1 d血清TRE、PAB和ALB水平比较差异无统计学意义(均P>0.05);两组术后3 d血清TRE、PAB和ALB水平均较术前1 d降低(均P<0.05),但ERAS组术后3 d血清TRE、PAB和ALB水平降低程度小于对照组(均P<0.05)(表5)。
表5 两组术前与术后营养状况指标变化比较(n=31, ±s)
±s)
Table 5 Comparison of nutritional status indexes between the two groups before and after operation (n=31,  ±s)
±s)

注:1)与术前1 d 比较,P<0.05
Note: 1) P<0.05 vs.preoperative value
组别 TRE(g/L) PAB(g/L) ALB(g/L)术前1 d 术后3 d 术前1 d 术后3 d 术前1 d 术后3 d ERAS 组 2.26±0.37 1.92±0.251) 0.25±0.04 0.19±0.051) 38.71±1.89 36.21±1.421)对照组 2.30±0.41 1.46±0.281) 0.26±0.07 0.12±0.031) 38.54±1.56 33.27±1.201)t 0.403 6.823 0.691 6.684 0.386 8.805 P >0.05 <0.05 >0.05 <0.05 >0.05 <0.05
3 讨 论
P D 是普通外科创伤最大、最复杂的一种手术,并发症和病死率较高,不仅要求医师具有精湛的手术技术,且对围术期患者病情观察及康复具有较高要求[11-16]。ERAS理念主要是指在循证医学证据支持下围术期采用一系列优化手段,能够最大限度地降低患者生理功能的干扰,同时还可减少患者心理及生理的创伤,减少并发症,从而加快恢复机体生理机能的目的[17-21]。ERAS理念主要提倡更充分术前准备,包括术前沟通、胃肠道准备、良好的营养支持等,通过加强术前宣教和交流减轻负性情绪及应激损伤;常规置管可缓解腹胀,降低吻合口瘘发生[22-23]。ERAS理念强调精准操作,减少术中出血和创伤,注意术中保温,采取术中保温可降低术后应激反应,从而有利于减少机体的分解代谢,进一步促进患者康复[24-25]。ERAS理念术后早期进食和下床活动,可促进肠蠕动恢复,增加抵抗力,促进切口愈合;同时还可减少术后输液量,避免由于输液过多导致肺顺应性降低、肺间质水肿,影响胃肠功能恢复;此外ERAS理念还可减轻手术创伤造成的免疫抑制且减少术后并发症发生[26-27]。刘力婕等[28]报道显示,快速康复外科应用于胰腺癌术后患者,可明显减轻术后炎症反应,改善免疫抑制,从而加速术后康复。本研究表明,ERAS组首次肛门排气时间、首次肛门排便时间和下床活动时间快于对照组,提示ERAS可促进胃肠功能恢复;ERAS组术后并发症低于对照组,提示ERAS可减少术后并发症 发生。
营养不良会影响免疫系统内的各个环节,同时还可影响细胞免疫功能的表达,从而降低细胞因子、补体和免疫球蛋白的合成,导致机体对肿瘤的免疫抑制减弱,以及术后微残留病灶较早出现的转移复发,进一步影响远期预后[29]。此外,营养不良会引起术后切口愈合缓慢,甚至发生吻合口瘘等并发症,故而改善机体术后营养状况对胃癌患者具有重要意义[30]。血清生化学指标中,可用来评价患者营养状况主要包括TRE、PAB和ALB等。目前,临床上尚无有关快速康复外科应用于胰腺癌术后患者方面研究。而本文研究表明,ERAS组术后3 d血清TRE、PAB和ALB水平高于对照组,提示ERAS可改善患者营养状况。
综上所述,ERAS对胰头癌行PD术患者应用效果良好,可加快术后恢复,改善患者营养状况,减少术后并发症。本文研究仍存在一些局限之处,纳入样本量小,且术后观察时间存在缺陷,还需在后续中进一步补充术后相关指标的动态变化,以及增加样本量,进一步深入研究,提供可靠的临床参考价值。
[1] Jang JY, Kang JS, Han Y, et al.Long-term outcomes and recurrence patterns of standard versus extended pancreatectomy for pancreatic head cancer: a multicenter prospective randomized controlled study[J].J Hepatobiliary Pancreat Sci, 2017, 24(7):426-433.doi:10.1002/jhbp.465.
[2] Looijen GA, Pranger BK, de Jong KP, et al.The Additional Value of Laparoscopic Ultrasound to Staging Laparoscopy in Patients with Suspected Pancreatic Head Cancer[J].J Gastrointest Surg, 2018, 22(7):1186-1192.doi: 10.1007/s11605-018-3726-9.
[3] Sugiura T, Okamura Y, Ito T, et al.Impact of Patient Age on the Postoperative Survival in Pancreatic Head Cancer[J].Ann Surg Oncol, 2017, 24(11):3220-3228.doi: 10.1245/s10434-017-5994-0.
[4] 柯能文, 刘续宝.胰十二指肠切除术在胰头癌治疗中的应用与进展[J].中国普外基础与临床杂志, 2019, 26(4):385-388.
KeNW, LiuXB.ApplIC ationand progress of pancreaticoduo denectomy in pancreatic head cancer[J].Chinese Journal of Bases and Clinics in General Surgery, 2019, 26(4):385-388.
[5] 杨雨, 吴宝强, 蔡辉华, 等.保留幽门的胰十二指肠切除术与传统胰十二指肠切除术治疗胰腺疾病及壶腹周围癌的术后恢复情况对比分析[J].南京医科大学学报: 自然科学版, 2018, 38(10):1435-1438.DOI:10.7655/NYDXBNS20181023.
Yang Y, Wu BQ, Cai HH, et al.Comparison of postoperative recoveries between pylorus-preserving pancreaticoduodenectomy and traditional pancreaticoduodenectomy in treatment of pancreatic diseases and periampullary cancer[J].Journal of Nanjing Medical University, 2018, 38(10):1435-1438.DOI:10.7655/NYDXBNS20181023.
[6] Kohga A, Yamamoto Y, Sugiura T, et al.Bile duct angulation and tumor vascularity are useful radiographic features for differentiating pancreatic head cancer and intrapancreatic bile duct cancer[J].Surg Today, 2018, 48(7):673-679.doi: 10.1007/s00595-018-1642-y.
[7] 李洋, 田艳涛.快速康复外科在胃癌外科的应用与展望[J].国际外科学杂志, 2017, 44(5):357-360.doi:10.3760/cma.j.issn.1673-4203.2017.05.021.
Li Y, Tian YT.Application and prospect of fast-track surgery in gastric cancer[J].International Journal of Surgery, 2017, 44(5):357-360.doi:10.3760/cma.j.issn.1673-4203.2017.05.021.
[8] 王伟, 陶京, 汤志刚, 等.胰十二指肠切除术中扩大淋巴结清扫与标准淋巴结清扫治疗胰头癌的临床研究[J].中国肿瘤外科杂志, 2019, 11(6):429-432.doi:10.3969/j.issn.1674-4136.2019.06.008.
Wang W, Tao J, Tang ZG, et al.Efficacies of Extended Versus Standard Lymphadenectomy in Pancreatoduodenectomy for Pancreatic Head Adenocarcinoma[J].Chinese Journal of Surgical Oncology, 2019, 11(6):429-432.doi:10.3969/j.issn.1674-4136.2019.06.008.
[9] 吐洪卡热·牙生, 肖永彪, 黄宽军.ERAS理念对II~III期结直肠癌围术期患者的临床疗效、免疫应激反应及生活质量的影响分析[J].实用癌症杂志, 2019, 34(3):444-446.doi:10.3969/j.issn.1001-5930.2019.03.027.
Tuhongkare YS, Xiao YB, Huang KJ.RAS on Clinical Effect, Immunological Stress Response and Living Quality of Patients with Colorectal Cancer of II-III Stages[J].The Practical Journal of Cancer, 2019, 34(3):444-446.doi:10.3969/j.issn.1001-5930.2019.03.027.
[10] 刘艳, 高蓓蕾, 葛国梅.胰腺癌快速康复外科护理研究现状[J].全科护理, 2017, 15(8):911-913.doi:10.3969/j.issn.1674-4748.2017.08.006.
Liu Y, Gao BL, Ge GM.Research status of enhanced recovery after surgery nursing for pancreatic cancer[J].Chinese General Practice Nursing, 2017, 15(8):911-913.doi:10.3969/j.issn.1674-4748.2017.08.006.
[11] 金继宽, 熊光冰, 朱峰, 等.腹腔镜与开腹胰十二指肠切除术治疗胰头癌的近期疗效分析[J].中华消化外科杂志, 2018, 17(7):718-723.doi:10.3760/cma.j.issn.1673-9752.2018.07.015.
Jin JK, Xiong GB, Zhu F, et al.Short-term outcome analysis of laparoscopic and open pancreaticoduodenectomy for pancreatic head cancer[J].Chinese Journal of Digestive Surgery, 2018, 17(7):718-723.doi:10.3760/cma.j.issn.1673-9752.2018.07.015.
[12] 刘学青, 邢中强, 秦建章, 等.腹腔镜胰十二指肠切除术联合腹腔热灌注治疗胰头癌[J].中华肝胆外科杂志, 2019, 25(10):778-780.doi:10.3760/cma.j.issn.1007-8118.2019.10.015.
Liu XQ, Xing ZQ, QinJZ,etal.LaparoscopIC pancreatoduodenectomy with intraperitoneal hyperthermic perfusion for pancreatic head cancer[J].Chinese Journal of Hepatobiliary Surgery, 2019, 25(10):778-780.doi:10.3760/cma.j.issn.1007-8118.2019.10.015.
[13] 董圣杰, 霍新合, 张泽峰, 等.胰十二指肠切除术治疗胰头癌伴壶腹周围癌的近远期疗效及安全性[J].现代生物医学进展, 2017, 17(23):4537-4540.doi:10.13241/j.cnki.pmb.2017.23.032.
Dong SJ, Huo XH, Zhang ZF, et al.Short- and Long-Term Efficacy and Safety of Pancreaticoduodenectomy for Pancreatic Head Carcinoma and Periampullary Carcinoma[J].Progress in Modern Biomedicine, 2017, 17(23):4537-4540.doi:10.13241/j.cnki.pmb.2017.23.032.
[14] 唐荣, 郑辉, 陈杰, 等.腹腔镜胰十二指肠切除术对胰头癌术后并发症及预后的影响分析[J].中国医学前沿杂志:电子版, 2017, 9(2):84-87.doi:10.12037/YXQY.2017.02-17.
Tang R, Zheng H, Chen J, et al.Analysis of postoperative complications and prognosis of patients with pancreatic head cancer treated by laparoscopic pancreaticoduodenectomy[J].Chinese Journal of the Frontiers of Medical Science: Electronic Version, 2017, 9(2):84-87.doi:10.12037/YXQY.2017.02-17.
[15] 王宇, 周俊, 吴晓俊, 等.扩大与标准胰十二指肠切除术对胰头癌患者影响预后的倾向性评分匹配分析[J].浙江医学, 2018, 40(19):2138-2141.doi:10.12056/j.issn.1006-2785.2018.40.19.2017-3062.
Wang Y, Zhou J, Wu XJ, et al.Prognosis of patients with pancreatic head carcinoma undergoing extended versus standard pancreatoduodenectomy: a propensity score matching analysis[J].Zhejiang Medical Journal, 2018, 40(19):2138-2141.doi:10.12056/j.issn.1006-2785.2018.40.19.2017-3062.
[16] 吴文广, 吴向嵩, 李茂岚, 等.胰头癌胰十二指肠切除标本病理规范化处理的方法和意义[J].中华外科杂志, 2017, 55(1):37-40.doi:10.3760/cma.j.issn.0529-5815.2017.01.010.
Wu WG, Wu XS, Li ML, et al.Method and significance of specimens standardized pathological treatment in pancreaticoduodenectomy for pancreatic head cancer[J].Chinese Journal of Surgery, 2017, 55(1):37-40.doi:10.3760/cma.j.issn.0529-5815.2017.01.010.
[17] 陈晓晨.快速康复外科护理干预在结直肠癌患者围手术期中的应用效果观察[J].中国基层医药, 2019, 26(13):1640-1643.doi:10.3760/cma.j.issn.1008-6706.2019.13.028.
Chen XC.Clinical observation of FTS during the operation of colorectal cancer[J].Chinese Journal of Primary Medicine and Pharmacy, 2019, 26(13):1640-1643.doi:10.3760/cma.j.issn.1008-6706.2019.13.028.
[18] 郝世柱, 张晋冀.快速康复外科理念在结直肠癌患者行腹腔镜经自然腔道标本取出手术中的应用价值[J].中华肿瘤杂志, 2019, 41(10):796-800.doi:10.3760/cma.j.issn.0253?3766.2019.10.014.
Hao SZ, Zhang JJ.The application value of concept of enhanced recovery after surgery in patients with colorectal carcinoma after natural orifice specimen extraction surgery[J].Chinese Journal of Oncology, 2019, 41(10):796-800.doi:10.3760/cma.j.issn.0253?3766.2019.10.014.
[19] 金仙红.老年结直肠癌围术期护理中快速康复外科理念的应用效果[J].中国药物与临床, 2019, 19(24):4404-4406.doi:10.11655/zgywylc2019.24.089.
Jin XH.Application efficacy of ERAS in perioperative management of old patients with colorectal cancer[J].Chinese Remedies & Clinics, 2019, 19(24):4404-4406.doi:10.11655/zgywylc2019.24.089.
[20] 陈焕伟, 雷秋成.加速康复外科在肝切除围手术期中的应用现状及经验介绍[J].中华肝脏外科手术学电子杂志, 2019, 8(2):96-100.doi:10.3877/cma.j.issn.2095-3232.2019.02.004.
Chen HW, Lei QC.Application status and experience introduction of using enhanced recovery after surgery in perioperative period of hepatectomy[J].Chinese Journal of Hepatic Surgery, 2019, 8(2):96-100.doi:10.3877/cma.j.issn.2095-3232.2019.02.004.
[21] 郭程, 叶进.快速康复外科理念在头颈部肿瘤手术围手术期中的应用[J].中国耳鼻咽喉颅底外科杂志, 2019, 25(5):561-566.doi:10.11798/j.issn.1007-1520.201905024.
Guo C, Ye J.The application of the concept of enhanced recovery after surgery in perioperative period of head and neck tumors[J].Chinese Journal of Otorhinolaryngology-skull Base Surgery, 2019, 25(5):561-566.doi:10.11798/j.issn.1007-1520.201905024.
[22] 姜彪, 齐万里, 冷向阳, 等.快速康复外科理念在围手术期的应用及展望[J].长春中医药大学学报, 2018, 34(4):812-815.doi:10.13463/j.cnki.cczyy.2018.04.063.
Jiang B, Qi WL, Leng XY, et al.Application and prospect of rapid rehabilitation surgery in perioperative period[J].Journal of Changchun University of Traditional Chinese Medicine, 2018, 34(4):812-815.doi:10.13463/j.cnki.cczyy.2018.04.063.
[23] 姜晓娟, 林丽.探讨快速康复外科理念对宫颈癌围术期患者临床康复及生活质量的影响[J].中国性科学, 2019, 28(11):153-156.doi:10.3969/j.issn.1672-1993.2019.11.041.
Jiang XJ, Lin L.Exploration on the effect of rapid rehabilitation surgery concept on clinical rehabilitation and quality of life of patients with cervical cancer during perioperative period[J].Chinese Journal of Human Sexuality, 2019, 28(11):153-156.doi:10.3969/j.issn.1672-1993.2019.11.041.
[24] 王琼, 方瑜, 刘卓越.快速康复外科护理理念在甲状腺癌围手术期护理效果分析[J].贵州医药, 2019, 43(11):1825-1826.
Wang Q, Fang Y, Liu ZY.Analysis of application efficacy of enhanced recovery after surgery in perioperative nursing for thyroid cancer[J].Guizhou Medical Journal, 2019, 43(11):1825-1826.
[25] 李桂芩, 杨大雍.快速康复外科护理在外科领域中的系统评 价[J].锦州医科大学学报, 2018, 39(3):88-90.
Li GQ, Yang DY.Systematic Evaluation of Fast Track Surgery Nursing in Field of Surgery[J].Journal of Liaoning Medical University, 2018, 39(3):88-90.
[26] 许国定, 孙兴, 刘锦新, 等.快速康复治疗在胃肠道恶性肿瘤中的应用[J].微创医学, 2017, 12(1):57-60.doi:10.11864/j.issn.1673.2017.01.17.
Xu GD, Sun X, Liu JX, et al.Study on the application of minimally invasive surgery and fast-track surgery in gastrointestinal malignant tumor[J].Journal of Minimally Invasive Medicine, 2017, 12(1):57-60.doi:10.11864/j.issn.1673.2017.01.17.
[27] 吴琼, 沙永生.快速康复理念在外科护理中的应用现状及进 展[J].护士进修杂志, 2018, 33(20):1850-1853.doi:10.16821/j.cnki.hsjx.2018.20.008.
Wu Q, Sha YS.Application status and progress of enhanced recovery after surgery in surgical nursing[J].Journal of Nurses Training, 2018, 33(20):1850-1853.doi:10.16821/j.cnki.hsjx.2018.20.008.
[28] 刘力婕, 邹艳玲, 薛志芳, 等.快速康复外科在胰腺癌术后对血清IL-6、IL-10、TNF-α水平的影响[J].重庆医学, 2015, 44(19):2635-2637.doi:10.3969/j.issn.1671-8348.2015.19.015.
Liu LJ, Zou YL, Xue ZF, et al.The influence of fast track surgery on the concentrations of serum IL-6,IL-10 and TNF-α in pancreatic cancer patients[J].Chongqing Medicine, 2015, 44(19):2635-2637.doi:10.3969/j.issn.1671-8348.2015.19.015.
[29] 陈娟, 杜成, 丁震宇, 等.恶性肿瘤患者营养状况及相关影响因素分析[J].现代肿瘤医学, 2018, 26(1):91-94.doi:10.3969/j.issn.1672-4992.2018.01.024.
Chen J, Du C, Ding ZY, et al.The analysis of cancer patients' nutritional status and related factors analysis[J].Journal of Modern Oncology, 2018, 26(1):91-94.doi:10.3969/j.issn.1672-4992.2018.01.024.
[30] 应丽美, 陈芳芳, 陈艺丹, 等.国内肿瘤患者的营养风险及营养不良研究现状分析[J].肿瘤代谢与营养电子杂志, 2017, 4(2):226-231.doi:10.16689/j.cnki.cn11-9349/r.2017.02.020.
Ying LM, Chen FF, Chen YD, et al.Current research situation analysis of nutritional risk and malnutrition of tumor patients in China[J].Electronic Journal of Metabolism and Nutrition of Cancer, 2017, 4(2):226-231.doi:10.16689/j.cnki.cn11-9349/r.2017.02.020.
