急性乳腺炎是哺乳期女性的常见疾病,有资料表明,女性产后哺乳期急性乳腺炎的发病率可达9.5%~16%[1],大约3%哺乳期乳腺炎患者发展成为乳腺脓肿[2],而有的文献报道则高达11%[3]。乳腺脓肿形成后,既往常用的治疗方法是及时采取手术切开引流[4],传统的脓肿切开引流手术创伤较大,术后换药时疼痛程度重,换药次数多,切口及创腔愈合时间长,愈合后乳房上遗留下的疤痕明显,美容效果差,70%患者对切开排脓后乳房的美观不满意[5],给患者生理和心理上带来巨大的创伤。另外,脓肿切开引流术后容易出现乳瘘[6],部分患者因乳瘘导致切口长时间不愈合,最后不得不选择使用抑制泌乳药物,终止哺乳[7]。这剥夺了妇女哺乳及婴儿吸食母乳的权力,增加患者经济负担,同时也有悖于世界卫生组织和联合国儿童基金会为保障婴儿健康成长全力向世界推荐的科学育儿方法,现在推荐母乳喂养时间可达到2年[8]。目前,随着微创技术的发展,微创手术以其创伤小、恢复快、术后不遗留明显瘢痕等优点,被广泛应用于乳腺外科的治疗。对于乳腺脓肿,穿刺抽液和置管引流冲洗是近几年临床广泛开展的微创治疗方法。笔者对2012年2月—2018年2月在我院进行就诊并符合入组标准的哺乳期乳腺脓肿患者进行了一种自行探索出的微创腔镜治疗与传统切开引流的临床对比研究,前者显示了显著的临床效果,现将结果现报告如下。
1 资料与方法
1.1 一般资料
选取2012年2月—2018年2月在我院进行就诊的97例哺乳期乳腺脓肿患者作为研究对象。本研究经医院伦理委员会审核通过,且所有患者签署本研究的知情同意书。诊断及入组标准:⑴哺乳期女性乳房肿胀疼痛或伴畏寒、发热;⑵体查患侧乳房出现红、肿、热、痛,触及团块及波动感等炎症表现;⑶血常规白细胞,中性粒细胞增高;⑷乳腺超声提示乳房内混合回声或无回声区>5 cm,探头加压后见其内有液体流动;⑸穿剌抽出脓液。
1.2 方法
1.2.1 患者分组 将达到上述入组标准的患者按照就诊顺序,使用Excel 软件产生随机数字,奇数者入微创腔镜组,偶数者入常规组,微创腔镜组为超声引导下脓腔穿剌腔镜探查冲洗置管引流治疗组,常规组为常规开放切开纱条引流治疗组。
1.2.2 仪器设备 两组患者均使用同一台Mlndray M7Series 彩色多普勒超声诊断仪,探头频率10MHz。微创腔镜组使用德国狼牌F8-9.8 输尿管镜器械,常规组使用常规开放手术器械。
1.2.3 术前准备及麻醉 两组患者均取平卧位,患侧肩背部稍垫小枕,术前超声确定脓肿位置,了解脓肿数目,大小,脓液量,黏稠度,脓腔有无分隔。根据以上信息微创腔镜组设计穿剌点及方向途径,常规组设计手术切口,均进行体表标记。两组患者均釆用静脉复合麻醉,鼻导管鼻咽通气,保持呼吸道通畅。
1.2.4 微创腔镜组手术方法 定位标记,常规消毒,铺巾,将B 超探头涂无菌耦合剂后用无菌保护套包裹备用,用穿剌针在超声引导下按术前标记点及途径穿剌进入脓腔(图1A-B)。拔出针芯,接注射器抽出脓液后确定进入脓腔,脓液送细菌培养(图1C)。从穿剌针内将导丝置入脓腔,退出穿剌针,用16F 扩张器外带套管鞘,在超声引导下沿导丝方向置入脓腔,退出扩张器(图2A),将套管鞘及导丝留置于脓腔内,可见脓液从套管鞘内流出(图2B),从套管鞘内置入输尿管镜(图2C)。在输尿管镜直视下对脓腔进行探查冲洗(图3A),将脓液冲洗干净,必要时可从输尿管镜中置入输尿管镜钳在腔镜监视下协助操作或取组织活检(图3B)。腔镜下探查脓腔冲洗干净后退出腔镜,从套管鞘内向脓腔内置入引流管,退出套管鞘,缝合固定引流管,接引流袋,盖无菌敷料(图3C)。
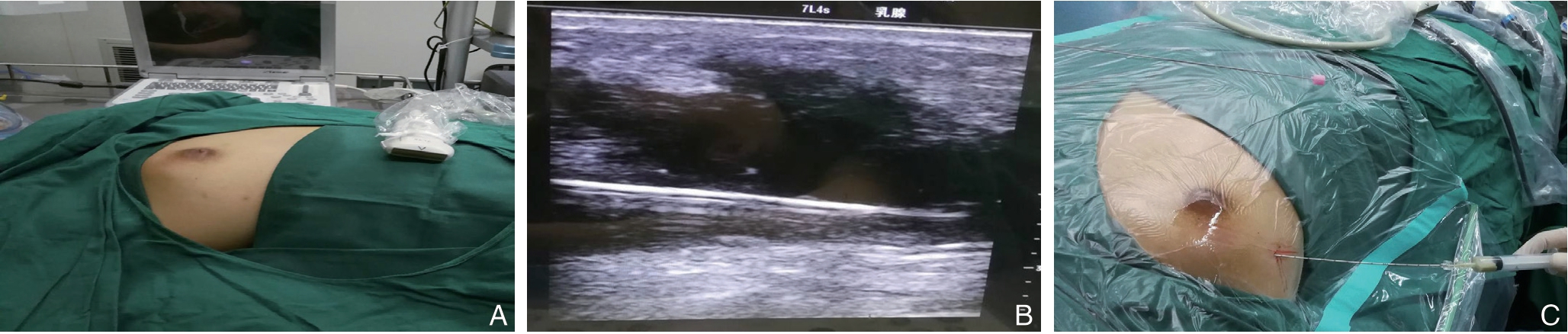
图1 术中照片1 A:穿刺点定位标记;B:超声引导下置入穿刺针;C:注射器抽取脓液
Figure 1 Intraoperative view 1 A:Positioning and marking the puncture point;B:Placement of the needle under ultrasound guidance;C:Pus aspiration using a syringe
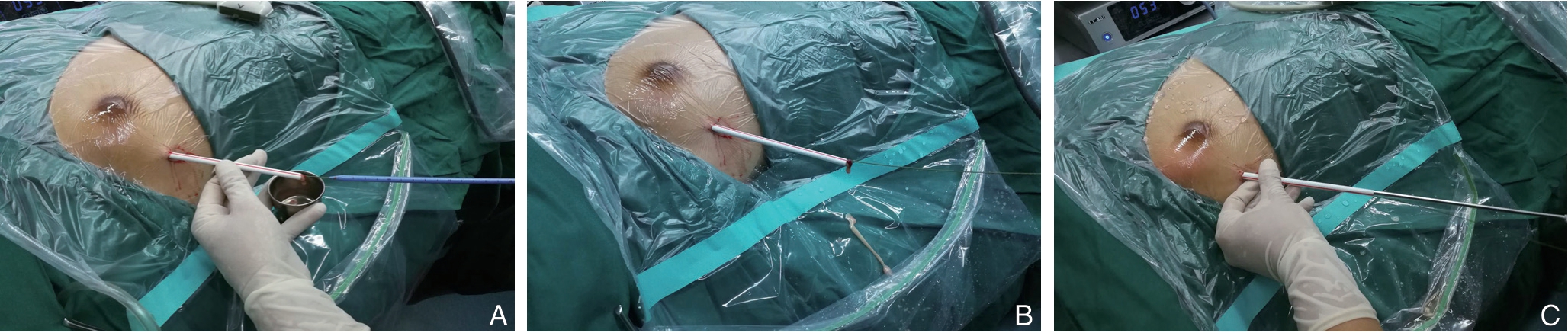
图2 术中照片2 A:沿导丝置入套管鞘,退出扩张器;B:留置导丝及套管鞘,确认套管位置;C:置入输尿管镜
Figure 2 Intraoperative view 2 A:Insertion of the cannula sheath along the guide wire and withdrawal of the dilator;B:Indwelling the guide wire and cannula sheath to confirm cannula position;C:Placement of the ureteroscopy
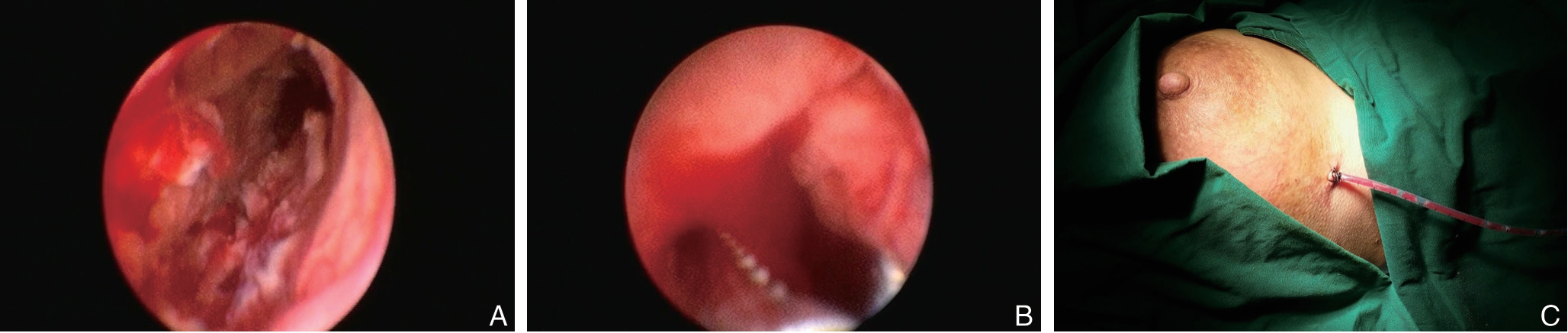
图3 术中照片3 A:输尿管镜直视下脓腔探查冲洗;B:输尿管镜直视下钳夹脓腔组织;C:留置、固定脓腔引流管
Figure 3 Intraoperative view 3 A:Exploration and irrigation of the abscess cavity under direct ureteroscopic vision;B:Clamping the tissue in the abscess cavity under direct ureteroscopic vision;C:Indwelling and fixing drainage tube in the abscess cavity
1.2.5 常规组手术方法 常规组在乳腺超声定位引导下根据脓腔位置,取脓腔表面波动感最明显处作放射状切口,乳晕下脓肿沿乳晕边缘作弧形切口,深部脓肿或乳房后脓肿沿乳房下缘作弧形切口,脓腔较大时在脓肿最低部位另加作切口作对口引流[9],依次切开皮肤,皮下组织,用血管钳钝性进入脓腔,用手指伸入脓腔探查,消除脓腔内分隔,充分排出脓液及坏死组织,用生理盐水反复冲洗脓腔至清亮,脓腔内置入生理盐水纱布引流,盖无菌敷料并固定。
1.2.6 全身治疗 两组患者均给予全身抗感染治疗,首次抗生素的选择依据经验性用药,选择青霉素类,以美洛西林钠3.0 g 加入0.9% 氯化钠注射液100 mL 中静脉滴注,2 次/d,根据细菌培养及药敏试验结果调整用药,并根据患者症状、局部体征、体温以及血象情况适时停用抗生素[10-11]。
1.3 观察指标
由未参与本研究诊疗工作的医疗人员对所有患者的以下指标进行观察统计:⑴换药次数;⑵治愈时间;⑶治疗费用;⑷术后切口长度;⑸术后乳瘘率;⑹术后回乳率;⑺术后疼痛。疼痛评分:采用疼痛数字评分法(VAS),用0~10分表示不同程度的疼痛。0分表示无痛;1~3分表示有轻微的疼痛,能忍受;4~6分表示患者疼痛并影响睡眠,尚能忍受;7~10分表示患者有渐强烈的疼痛,疼痛难忍,影响食欲及睡眠。微创腔镜组患者在术后每次行伤口引流管冲洗换药后评估患者疼痛程度,取平均分作为最后得分。常规组患者在术后每次行伤口局部处理后(清理脓腔并更换纱条)评估患者疼痛程度,取平均分作为最后得分。
1.4 治愈标准及随访
⑴乳房疼痛缓解消失;⑵体温持续正常,患侧乳房无红、肿、热、痛等炎症表现,无明显压痛;⑶体查未触及波动感;⑷血常规正常;⑸复查乳腺B超无乳房内无混合回声或无回声区。出院后对所有患者随访12个月,当症状、体征无反复时判断定为临床治愈。
1.5 统计学处理
应用SPSS20.0统计软件进行统计分析,计数资料采用χ2检验,计量资料以均数±标准差( ±s)表示,采用两独立样本t检验,P<0.05为差异有统计学意义。
±s)表示,采用两独立样本t检验,P<0.05为差异有统计学意义。
2 结果
2.1 两组患者治疗前一般资料比较
共纳入符合入组条件的患者共97 例,其中微创腔镜组49例,常规组48例,所有患者均为女性。对两组患者的发病年龄、哺乳经验、产后病程、脓肿所在位置进行比较,差异性均无统计学意义(均P>0.05)(表1),具有可比性。
表1 微创腔镜组与常规组患者基本资料比较
Table 1 Comparison of the general data of patients in minimally invasive endoscopic group and conventional group
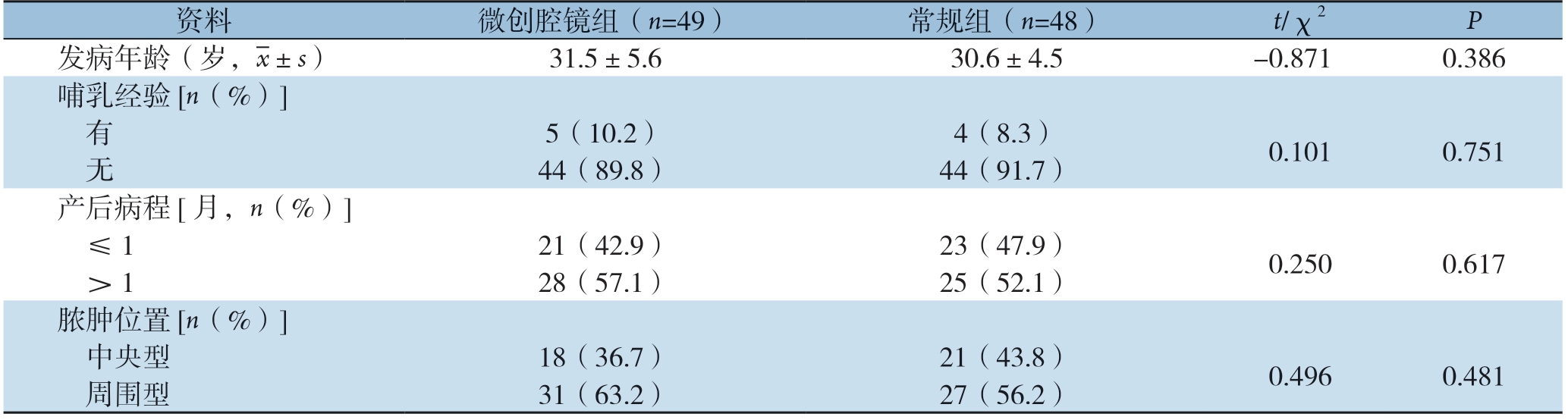
资料微创腔镜组(n=49)常规组(n=48) t/χ2P发病年龄(岁,images/BZ_33_832_2465_870_2506.png±s)31.5±5.630.6±4.5-0.8710.386哺乳经验[n(%)]有5(10.2)4(8.3)0.1010.751无44(89.8)44(91.7)产后病程[月,n(%)]≤121(42.9)23(47.9)0.2500.617>128(57.1)25(52.1)脓肿位置[n(%)]中央型18(36.7)21(43.8)0.4960.481周围型31(63.2)27(56.2)
2.2 两组患者治疗后相关指标比较
两组患者的疗效情况对比结果显示,微创腔镜组患者在换药次数、治愈时间、治疗费用方面要明显优于常规组,差异具有统计学意义(均P<0.05)。微创腔镜组患者的手术创伤(切口长度)(图4)、术后疼痛程度以及乳瘘、回乳等并发症发生率方面明显低于常规组,差异具有统计学意义(均P<0.05)(表2)。两组治疗后均无复发情况。
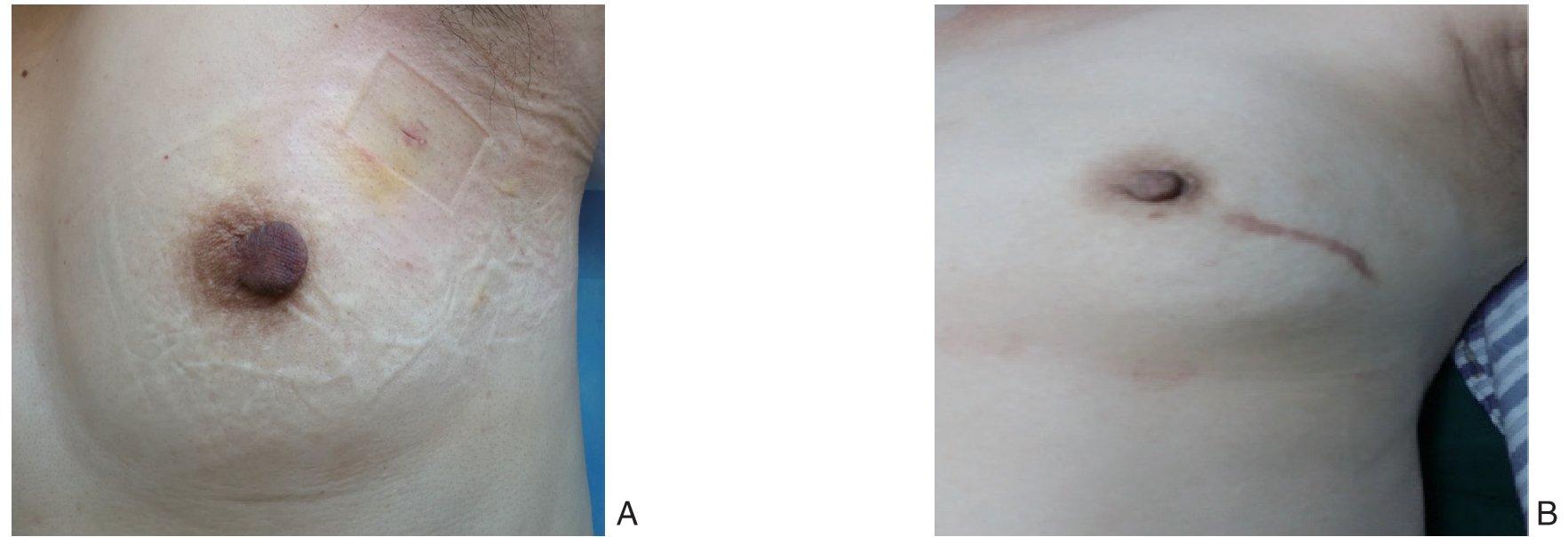
图4 术后照片 A:腔镜手术切口愈合情况;B:传统手术切口愈合情况
Figure 4 Postoperative view A:Wound healing after endoscopic surgery;B:Wound healing after traditional surgery
表2 微创腔镜组与常规组患者治疗后相关指标比较
Table 2 Comparison of relevant variables of patients in minimally invasive endoscopic group and conventional group after treatment
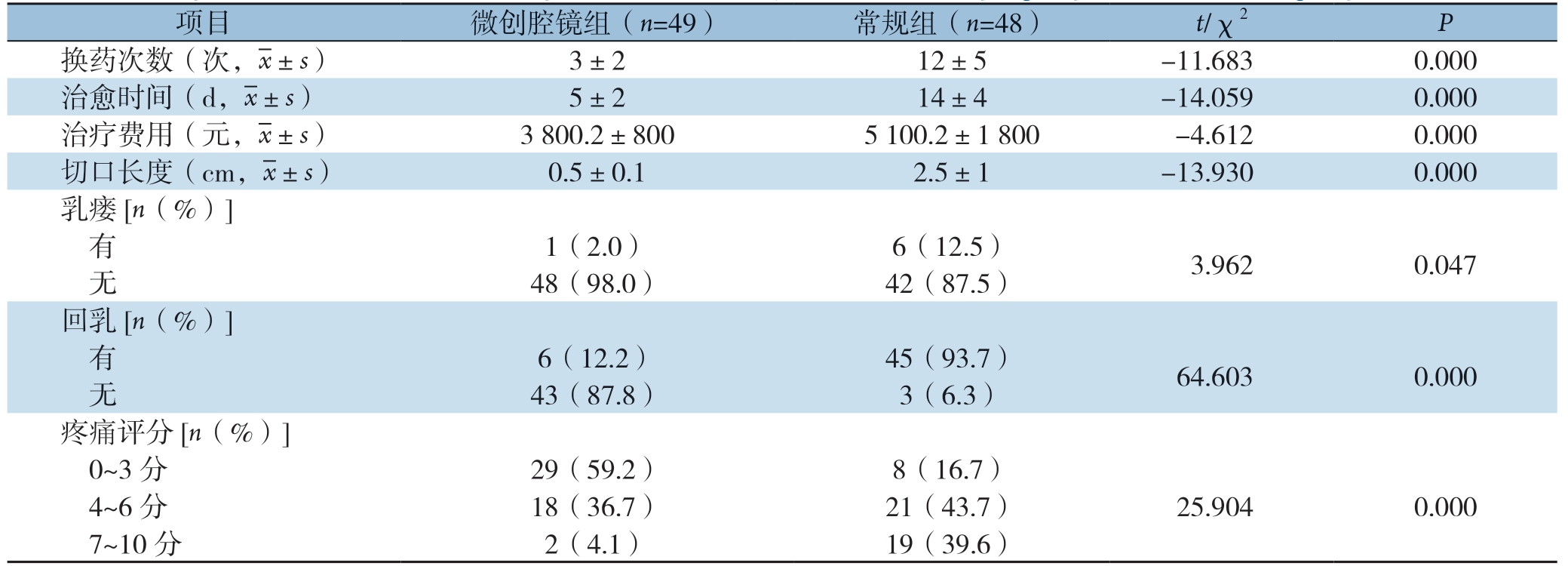
项目微创腔镜组(n=49)常规组(n=48)t/χ2P换药次数(次,images/BZ_33_832_2465_870_2506.png±s)3±212±5-11.6830.000治愈时间(d,images/BZ_33_832_2465_870_2506.png±s)5±214±4-14.0590.000治疗费用(元,images/BZ_33_832_2465_870_2506.png±s)3800.2±8005100.2±1800-4.6120.000切口长度(cm,images/BZ_33_832_2465_870_2506.png±s)0.5±0.12.5±1-13.9300.000乳瘘[n(%)]有1(2.0)6(12.5)3.9620.047无48(98.0)42(87.5)回乳[n(%)]有6(12.2)45(93.7)64.6030.000无43(87.8)3(6.3)疼痛评分[n(%)]0~3 分29(59.2)8(16.7)4~6 分18(36.7)21(43.7)25.9040.0007~10 分2(4.1)19(39.6)
3 讨论
哺乳期乳腺炎常常在乳汁淤积基础上诱发的急性乳房炎症,一般由细菌感染所致,也可不伴细菌感染,常在短期内形成脓肿,多由金黄色葡萄球菌或链球菌从乳头破口或皲裂处侵入,也可直接侵入引起感染。临床表现为乳房皮肤出现红、肿、热、痛感染症状,可伴寒战、发热,以初产妇更为多见[12]。哺乳期乳腺炎多见于哺乳期1个月内,其发生与脓肿形成可能与乳头损伤细菌侵入,乳头内陷皲裂,乳房外伤,导管先天性不通畅,产妇授乳结验不足所致乳汁淤积,母婴分离,患者机体免疫力下降等因素有关[13-16]。
哺乳期乳腺炎早期可通过保守治疗处理,如使用抗生素、中医中药、局部理疗等,而其治疗重点是有效排出淤积的乳汁,促进炎症消散[17-19]。当乳腺脓肿形成以后治疗方法是及时手术切开引流[20],这种方法简单有效,对医疗设备及医师的要求不高,便于基层医疗机构开展。但是,术后前期渗出量较大,需每天换药1~2次,每次换药需取出创腔内引流纱条,清除坏死组织,清洗创腔,重新置入纱条引流,整个换药过程持续时间长,给患者带来的疼痛程度重,部分患者因此对术后换药产生恐惧甚至排斥换药。创腔内置入纱条目的在于引流,同时引流物作为一种创腔内的异物存在,影响创腔愈合的速度,治疗时间长,愈合后疤痕明显,对乳房外观造成明显影响,给患者在生理和心理带来巨大的创伤。并且乳瘘发生率高,很多患者因此终止母乳喂养。既增加患者术后并发症和经济负担,亦大大增加医疗材料使用量和医务人员工作量。
当哺乳期乳腺脓肿形成,有学者[21-23]认为可借助超声引导下行细针穿剌抽脓,这一术式曾一度取代切开排脓成为一线乳腺脓肿的治疗方案。Eryilmaz等[24]认为,脓肿最大径<5.0 cm者适合采用超声引导下反复细针穿剌抽液治疗,并可保持最佳的乳房外观。但对于直径>5.0 cm的脓肿及形成时间较长的脓肿细针穿剌抽脓效果不佳[25-26]。还有研究[27-28]提示,脓肿直径>5.0 cm,多腔脓肿,脓肿持续时间较长的患者均建议首选传统手术治疗。
近年来,超声引导下真空辅助乳腺微创旋切活检系统治疗乳腺脓肿被逐渐推广。该术式切口长约0.3 cm,疤痕不明显,手术过程中通过超声引导,脓肿周围组织结构清楚,手术操作对正常乳腺组织损伤小,术后切口局部干燥,清洁,便于管理,乳瘘发生率有所下降,但是旋切刀费用高,会大大增加患者经济负担,在临床运用上有较大的局限性[29-31]。
本研究中微创腔镜组患者先在超声引导下行脓腔穿剌置鞘,再行腔镜探查冲洗置管引流。术中通过微创单孔即可置入输尿管镜,并可借助输尿管镜钳实现直视下坏死组织的清除,必要时可夹取组织活检。术中通过腔镜的画面放大效应,操作视野更清晰,因此优于传统手术的手术视野。通过输尿管镜的冲洗通道可以对所有脓腔可实现彻底冲洗,避免脓腔残留,有利于术后炎症的吸收,加速创腔的愈合,从而缩短病程。本研究中两组患者手术时间不长,均采用静脉麻醉,术中无疼痛感,疼痛主要发生在术后换药。微创腔镜组患者术毕经套管鞘向脓腔内留置16F引流管1根,能够实现术后的充分引流。并且引流管对创腔剌激性相对较小,术后渗液从引流管流入引流袋,每2~3天换药1次即可,每次换药仅需冲洗消毒引流管及周围皮肤更换敷料,对患者剌激不大,几乎无疼痛感,因此在疼痛感受方面也明显优于传统手术。本研究中微创腔镜组患者的换药次数、治愈时间及住院费用均明显少于常规组患者,表明微创腔镜技术治疗乳腺脓肿恢复更快。此外,通过引流管可观察引流量及性质,了解有无乳瘘发生。当术后引流量逐渐减少,5 d左右可拔除引流管,切口愈合后出院。微创腔镜组患者的手术切口长度在0.5 cm左右,明显小于传统手术切口,愈合后疤痕不明显,乳房外观及美容效果满意。
微创腔镜组患者术中在超声引导按预定途经进入脓腔,并借助腔镜实现术中可视化操作,因此乳腺导管损伤可能性小,术后乳瘘发生率低。本组患者中仅有1例出现乳瘘,6例回乳患者均因个人原因,并非术后乳瘘不得已而使用抑制泌乳药物终止哺乳。术中脓腔冲洗彻底,无明显切口暴露,术后乳房局部红、肿、热、痛等症迅速得到控制,体温下降正常,可以减少抗生素药物使用的时间。与丁松涛等[32]认为哺乳期乳腺炎,尤其是乳腺脓肿阶段,不可盲目滥用抗生素观点一致。患者因受抗生素药物影响较小,暂停哺乳时间短甚至无需停止哺乳,术后恢复快,病程短,治疗费用低,患者很快可以恢复正常哺乳,而母乳喂养是既经济又利于母婴健康的方法。术后随访两组患者12个月,两组均无复发病例,表明微创腔镜手术在治疗乳腺脓肿中能够获得与传统手术相似的临床效果。
当然,开展此项微创腔镜技术也存在一定的局限性:对于乳腺脓肿直径<5 cm的患者不适用。手术操作需要配置术中超声设备、微创器械及腔镜系统,术者要有一定的超声和腔镜操作技术基础,对于腔镜设备配置不高,会导致图像视野不佳,增加操作难度,脓腔坏死组织清除不彻底等缺点。对于基层医院医生开展此项技术,建议进行适当培训。此项微创腔镜技术,术中需使用超声、腔镜等设备,单从手术费而言高于传统切开排脓手术。但此项技术术后换药次数少,并发症发生率低,缩短住院时间。目前统计数据显示总体治疗费用优于切开排脓手术组,且有很好的美容效果,在实际应用中可以根据医院设备条件及患者的意愿需求进行选择。
综上所述,微创腔镜技术在直径>5.0 cm哺乳期乳腺脓肿中治疗效果显著,能够减轻术后疼痛,减少换药次数,缩短治疗时间,减少治疗费用,减少乳瘘发生率,手术切口小,微创美容。该术式提高了临床治疗效果,减少了临床并发症的发生,因此值得临床推广及应用。
[1]Schoenfeld EM,McKay MP.Mastitis and methicillinresistant Staphylococcus aureus(MRSA):the calm before the storm?[J].JEmerg Med,2010,38(4):e31–34.doi:10.1016/j.jemermed.2008.11.021.
[2]Academy of Breastfeeding Medicine Protocol Committee ABM clinical protocol #4:mastitis.Revision,May 2008[J].Breastfeed Med,2008,3(3):177–180.doi:10.1089/bfm.2008.9993.
[3]Amir LH,Forster D,McLachlan H,et al.Incidence of breast abscess in lactating women:report from an Australian cohort[J].BJOG,2004,111(12):1378–1381.doi:10.1111/j.1471–0528.2004.00272.x.
[4]黎介寿,吴孟超,黄志强.普通外科手术学[M].第2版.北京:人民军医出版社,2005:332.
Li JS,Wu MC,Huang ZQ.Operative General Surgery[M].2nd Ed.Beijing:People's Military Medical Press,2005:332.
[5]姜军.现代乳腺外科学[M].北京:人民卫生出版社,2014:214.Jiang J.Modern Breast Surgery[M].Beijing:People's Medical Publishing House,2014:214.
[6]赵志全,黄汉源.乳腺导管瘘的诊断和治疗[J].中华普通外科杂志,1998,13(4):252–253.
Zhao ZQ,Huang HY.Diagnosis and treatment of mammary ductal fistula[J].Zhong Hua Pu Tong Wai Ke Za Zhi,1998,13(4):252–253.
[7]中国妇幼保健协会乳腺保健专业委员会乳腺炎防治与促进母乳喂养学组.中国哺乳期乳腺炎诊治指南[J].中华乳腺病杂志:电子版,2020,14(1):10–14.doi:10.3877/cma.j.issn.1674–0807.2020.01.005.
Prevention and Treatment of Mastitis and Breastfeeding Promotion Group,Professional Committee of Breast Health,China Maternal and Child Health Association.Chinese guidelines for prevention and treatment of mastitis[J].Chinese Journal of Breast Disease:Electronic Version,2020,14(1):10–14.doi:10.3877/cma.j.issn.1674–0807.2020.01.005.
[8]World Health Organization.Report of the expert consultation of the optimal duration of exclusive breastfeeding,Geneva,Switzerland,28–30March 2001.https://apps.who.int/iris/handle/10665/67219.
[9]陈孝平,汪建平.外科学[M].北京:人民卫生出版社,2013:253–254.
Chen XP,Wang JP.Surgery[M].Beijing:People's Medical Publishing House,2013:253–254.
[10]闫智清,马祥君,王青,等.哺乳期急性乳腺炎的致病菌分布及其药敏特点[J].中国综合临床,2014,30(7):732–734.doi:10.3760/cma.j.issn.1008–6315.2014.07.022.
Yan ZQ,Ma XJ,Wang Q,et al.Pathogenic bacteria distribution and drug susceptibility characteristics of the patients with lactation acute mammitis[J].Clinical Medicine of China,2014,30(7):732–734.doi:10.3760/cma.j.issn.1008–6315.2014.07.022.
[11]宁平,刘泽宇,陈军,等.哺乳期乳腺炎临床分型及个体化治疗策略的探讨[J].中华乳腺病杂志:电子版,2013,7(4):7–11.doi:10.3877/cma.j.issn.1674–0807.2013.04.002.
Ning P,Liu ZY,Chen J,et al.Clinical classification of lactational mastitis and strategies of individualized therapy[J].Chinese Journal of Breast Disease:Electronic Version,2013,7(4):7–11.doi:10.3877/cma.j.issn.1674–0807.2013.04.002.
[12]Amir LH,Academy of Breastfeeding Medicine Protocol Committee.ABM clinical protocol #4:mastitis,revised March 2014[J].Breastfeed Med,2014,9(5):239–243.doi:10.1089/bfm.2014.9984.
[13]何湘萍,马祥君,赵银珠,等.行为方式与哺乳期急性乳腺炎发病的相关性分析[J].中华乳腺病杂志:电子版,2013,7(1):35–38.doi:10.3877/cma.j.issn.1674–0807.2013.01.009.
He XP,Ma XJ,Zhao YZ,et al.Correlation analysis between the patients' behaviors and acute lactational mastitis[J].Chinese Journal of Breast Disease:Electronic Version,2013,7(1):35–38.doi:10.3877/cma.j.issn.1674–0807.2013.01.009.
[14]贺青卿,单礼成,范西红,等.末端输乳管扩张术治疗早期急性乳腺炎[J].中国普通外科杂志,1999,8(5):376.
He QQ,Shan LC,Fan XH,et al.Dilation of terminal lactiferous duct in treatment of early acute mastitis[J].Chinese Journal of General Surgery,1999,8(5):376.
[15]Branch-Elliman W,Golen TH,Gold HS,et al.Risk factors for Staphylococcus aureus postpartum breast abscess[J].Clin Infect Dis,2012,54(1):71–77.doi:10.1093/cid/cir751.
[16]Pérez A,Orta L,Padilla E,et al.CA-MRSA puerperal mastitis and breast abscess:a potential problem emerging in Europe with many unanswered questions[J].JMatern Fetal Neonatal Med,2013,26(9):949–951.doi:10.3109/14767058.2013.766700.
[17]马祥君,汪洁,孔令伟,等.哺乳期急性乳腺炎四级预防方案的可行性[J].中国妇幼保健,2010,25(17):2335–2338.
Ma XJ,Wang J,Kong LW,et al.Feasibility of four grades prevention strategy for acute mastitis during lactation[J].Maternal&Child Health Care of China,2010,25(17):2335–2338.
[18]何湘萍,马祥君,陈颖,等.哺乳期急性乳腺炎发病初期非抗生素治疗研究[J].中华乳腺病杂志:电子版,2012,6(6):691–694.doi:10.3877/cma.j.issn.1674–0807.2012.06.015.
He XP,Ma XJ,Chen Y,et al.Study of nonantibiotic therapy for acute mastitis in lactation at initial stage of onset[J].Chinese Journal of Breast Disease:Electronic Version,2012,6(6):691–694.doi:10.3877/cma.j.issn.1674–0807.2012.06.015.
[19]何湘萍,马祥君,汪洁,等.中药联合综合物理治疗在哺乳期急性乳腺炎发病初期的应用研究[J].新中医,2013,45(2):80–82.
He XP,Ma XJ,Wang J,et al.Application of Chinese Medicine Combined with Integrated Physical Therapy in Early Stage of Acute Mastitis During Lactation Period[J].Journal of New Chinese Medicine,2013,45(2):80–82.
[20]高雅军,马祥君,何湘萍,等.哺乳期急性乳腺炎发展成乳腺脓肿的相关因素分析[J].中华乳腺病杂志:电子版,2015,9(1):35–38.doi:10.3877/cma.j.issn.1674–0807.2015.01.008.
Gao YJ,Ma XJ,He XP,et al.Related factor analysis in breast abscess developed from acute lactation mastitis[J].Chinese Journal of Breast Disease:Electronic Version,2015,9(1):35–38.doi:10.3877/cma.j.issn.1674–0807.2015.01.008.
[21]张云微,王娇.彩超引导下脓肿穿刺置管引流术治疗哺乳期乳腺炎[J].中国现代普通外科进展,2021,24(3):229–230.doi:10.3969/j.issn.1009–9905.2021.03.016.
Zhang YW,Wang J.Abscess drainage by puncture and catheterization under guidance of color ultrasound for lactational mastitis[J].Chinese Journal of Current Advances in General Surgery,2021,24(3):229–230.doi:10.3969/j.issn.1009–9905.2021.03.016.
[22]何湘萍,陈颖,马祥君,等.哺乳期乳腺脓肿患者经超声引导下细针穿刺冲洗术后回乳的影响因素分析[J].中华乳腺病杂志:电子版,2019,13(5):286–289.doi:10.3877/cma.j.issn.1674–0807.2019.05.006.
He XP,Chen Y,Ma XJ,et al.Factors influencing delactation in lactational breast abscess patients treated by ultrasound-guided aspiration and irrigation[J].Chinese Journal of Breast Disease:Electronic Version,2019,13(5):286–289.doi:10.3877/cma.j.issn.1674–0807.2019.05.006.
[23]丁韬,魏涧.不同引流方法治疗哺乳期乳腺脓肿的效果对比[J].中华乳腺病杂志:电子版,2019,13(3):177–178.doi:10.3877/cma.j.issn.1674–0807.2019.03.008.
Ding T,Wei J.Efficacy comparison of different drainage methods in treatment of lactational breast abscess[J].Chinese Journal of Breast Disease:Electronic Version,2019,13(3):177–178.doi:10.3877/cma.j.issn.1674–0807.2019.03.008.
[24]Eryilmaz R,Sahin M,Hakan Tekelioglu M,et al.Management of lactational breast abscesses[J].Breast,2005,14(5):375–379.doi:10.1016/j.breast.2004.12.001.
[25]程顺舟,王吉荣,王海燕.哺乳期乳腺脓肿行穿刺抽吸及切开引流的对比分析[J].江苏医药,2016,42(24):2749–2750.
Cheng SZ,Wang JR,Wang HY.Comparison of needle aspiration and open surgery drainage in treatment of lactational breast abscesses[J].Jiangsu Medical Journal,2016,42(24):2749–2750.
[26]唐铁雷,蒋亚茹,李有怀,等.哺乳期乳腺脓肿微创穿刺治疗的临床应用[J].中国妇幼保健,2018,33(19):4534–4536.doi:10.7620/zgfybj.j.issn.1001–4411.2018.19.71.
Tang TL,Jiang YR,Li YH,et al.Clinical application of minimall y invasive puncture in treatment of lactational breast abscesses[J].Maternal &Child Health Care of China,2018,33(19):4534–4536.doi:10.7620/zgfybj.j.issn.1001–4411.2018.19.71.
[27]Lam E,Chan T,Wiseman SM.Breast abscess:evidence based management recommendations[J].Expert Rev Anti lnfect Ther,2014,12(7):753–762.doi:10.1586/14787210.2014.913982.
[28]刘娟,李青国,王金星,等.哺乳期乳腺脓肿外科治疗的临床分析[J].中华全科医师杂志,2019,18(5):473–475.doi:10.3760/cma.j.issn.1671–7368.2019.05.015.
Liu J,Li QG,Wang JX,et al.Clinical analysis on surgical treatment of breast abscess during lactation[J].Chinese Journal of General Practitioners,2019,18(5):473–475.doi:10.3760/cma.j.issn.1671–7368.2019.05.015.
[29]续哲莉,边学海,王瑞庆,等.Mammotome微创旋切系统治疗乳腺脓肿:附53例报告[J].中国普通外科杂志,2007,16(11):1063–1065.doi:10.3969/j.issn.1005–6947.2007.11.010.
Xu ZL,Bian XH,Wang RQ,et al.Mammotome minimally invasive system in the treatment of breast abscess:a report of 53 cases[J].Chinese Journal of General Surgery,2007,16(11):1063–1065.doi:10.3969/j.issn.1005–6947.2007.11.010.
[30]刘远坤,黄晓宇,翁玉英,等.麦默通微创旋切术在乳腺深部脓肿治疗中的应用[J].中国普通外科杂志,2015,24(11):1601–1604.doi:10.3978/j.issn.1005–6947.2015.11.020.
Liu YK,Huang XY,Weng YY,et al.Application of Mammotome rotation cutting in treatment of deep breast abscess[J].Chinese Journal of General Surgery,2015,24(11):1601–1604.doi:10.3978/j.issn.1005–6947.2015.11.020.
[31]Chen C,Luo L,Gao D,et al.Surgical drainage of lactational breast abscess with ultrasound-guided Encor vacuum-assisted breast biopsy system[J].Breast J,2019,25(5):889–897.doi:10.1111/tbj.13350.
[32]丁松涛,何湘萍,马祥君,等.超声引导下脓肿穿刺术治疗哺乳期乳腺脓肿的临床分析[J].中华乳腺病杂志:电子版,2017,11(3):157–161.doi:10.3877/cma.j.issn.1674–0807.2017.03.007.
Ding ST,He XP,Ma XJ,et al.Clinical analysis of lactational breast abscess treated by ultrasound-guided aspirationChinese Journal of Breast Disease:Electronic Version,2017,11(3):157–161.doi:10.3877/cma.j.issn.1674–0807.2017.03.007.
