下肢深静脉血栓形成(deepvenous thrombosis,DVT)是血管外科的常见病,即使经过抗凝治疗仍有20%~50%进展为深静脉血栓后综合征(post-thrombotic syndrome,PTS)[1-2],其中5%~10%可发展为严重PTS[3-5]。对于急性DVT,导管接触性溶栓(catheter-directed thrombolysis,CDT)能有效清除血栓,显著降低PTS的发生率,是临床中广泛应用的溶栓方法[6-9]。腘静脉入路是CDT治疗中最常见的穿刺部位[10-11],但对于混合型DVT,尿激酶无法覆盖膝下病变。小腿深静脉入路体位要求低,尿激酶可以更广泛覆盖血栓部位,提高血栓溶解率,且CDT过程膝关节不受限、提高患者舒适度,不易出现关节屈曲引起穿刺部位渗血[12]。本中心对急性混合型DVT患者由早期浅静脉溶栓、胫后静脉切开置管溶栓逐渐转变为小腿深静脉穿刺置管行CDT治疗,取得良好的效果,报告如下。
1 资料与方法
1.1 一般资料
收集海南省人民医院血管外科2012年1月—2017年12月共172例急性混合型DVT患者的临床资料,其中89例通过小腿深静脉穿刺行CDT治疗(穿刺组);54例通过暴露胫后静脉,直视下穿刺胫后静脉行CDT治疗(切开组);29例行足背浅静脉溶栓(浅静脉组)。穿刺组:男42例,女47 例;左下肢59 条,右下肢30 条。切开组:男31 例,女23 例;左下肢32 条,右下肢22 条。浅静脉组:男13例,女16例;左下肢20条,右下肢9条。172例患者的平均年龄(43±15)岁,病程(5.3±1.2)d,患者危险因素资料见表1。
表1 患者危险因素[n(%)]
Table 1 Risk factors of the patients[n(%)]
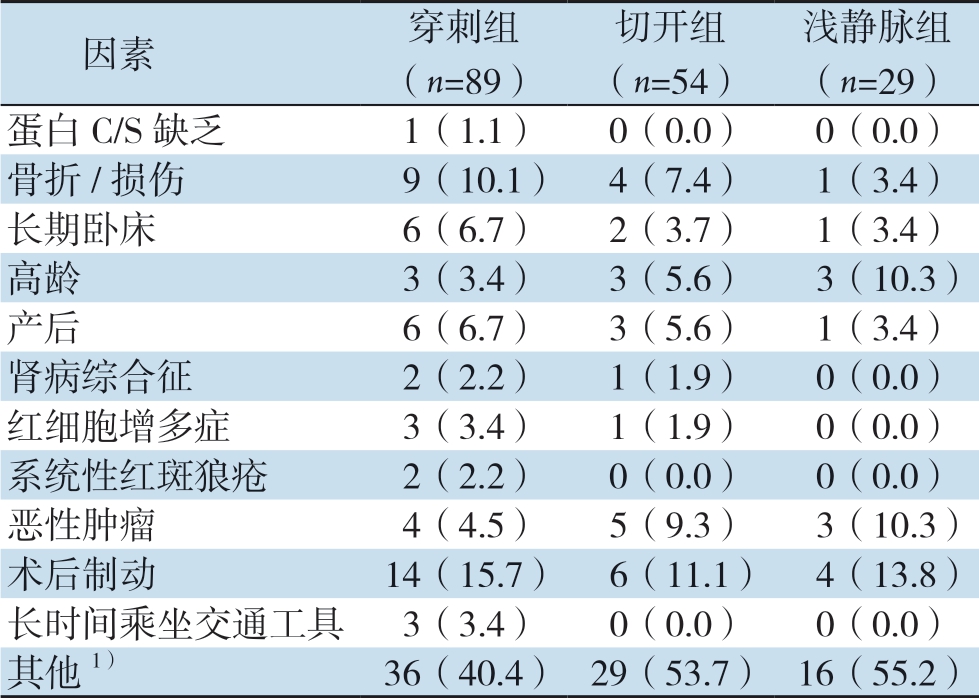
注:1)为疑似危险因素或不明因素
Note:1)The suspicious risk factors or unclear factors
浅静脉组(n=29)蛋白C/S 缺乏1(1.1)0(0.0)0(0.0)骨折/损伤9(10.1) 4(7.4)1(3.4)长期卧床6(6.7)2(3.7)1(3.4)高龄3(3.4)3(5.6)3(10.3)产后6(6.7)3(5.6)1(3.4)肾病综合征2(2.2)1(1.9)0(0.0)红细胞增多症3(3.4)1(1.9)0(0.0)系统性红斑狼疮2(2.2)0(0.0)0(0.0)恶性肿瘤4(4.5)5(9.3)3(10.3)术后制动14(15.7) 6(11.1) 4(13.8)长时间乘坐交通工具3(3.4)0(0.0)0(0.0)其他1)36(40.4) 29(53.7) 16(55.2)因素穿刺组(n=89)切开组(n=54)
纳入标准:经超声明确为混合型DVT;病程<14 d;年龄<75 岁。排除标准:患肢为复发性DVT;下腔静脉闭塞;溶栓药物使用禁忌[6];未能坚持弹力袜压力梯度治疗者;未能按要求服用抗凝药物者;未能定期随访者。
1.2 手术方法
穿刺组:患者仰卧位,在足背浅静脉穿刺放置套管针,于踝关节上5 cm、膝关节下5 cm、膝关节上5 cm分别扎1条止血带,使浅静脉注射的对比剂通过穿通支进入深静脉。全下肢消毒、铺巾,助手通过套管针注入30 mL 70%稀释对比剂,同时双手挤压患肢踝部及小腿下段约30 s,使更多对比剂进入深静脉。在DSA辅助下旋转患肢,从不同角度寻找合适的深静脉备穿刺。确定深静脉后5%利多卡因于穿刺点周围局部麻醉,助手固定患肢,同时缓慢、持续注入对比剂。沿静脉走形方向,钢针(导管鞘,中国益心达)以60°~70°进针,穿破静脉时会有突破感,此时静脉血由于肢体内部压力过高大量涌出,固定钢针,取导丝(RADIFOCUS,日本泰尔茂)缓慢进入深静脉,确认后置入4 F血管鞘(图1)。切开组:于内踝后方纵行切开皮肤,暴露胫后静脉,直视下穿刺并置入4 F血管鞘,成功置管后逐层缝合切口。浅静脉组:足背浅静脉溶栓。
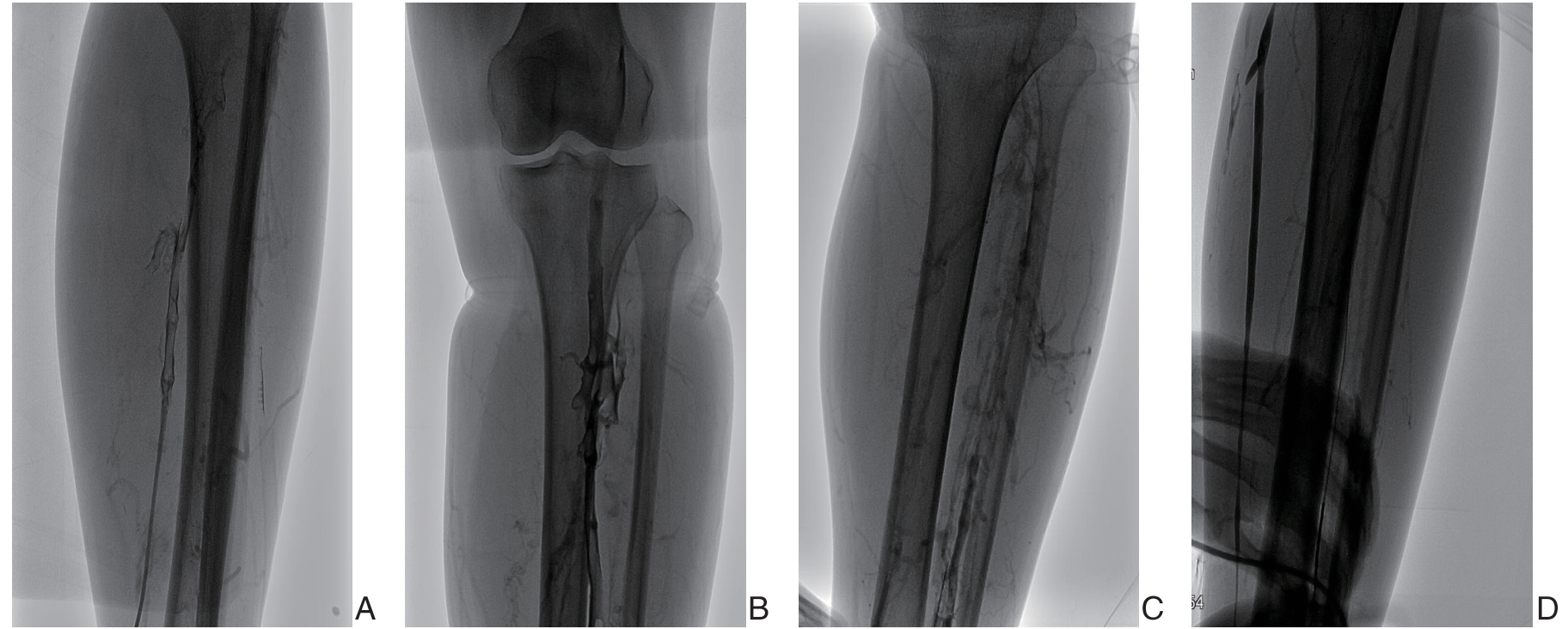
图1 小腿深静脉穿刺 A:穿刺胫后静脉,造影发现静脉大量血栓;B:穿刺腓静脉,造影发现腓静脉、腘静脉大量血栓;C:腓静脉、胫前静脉同时显影,拟穿刺胫前静脉;D:穿刺腓静脉并置入导丝
Figure 1 Deep vein puncture of the lower leg A:Puncture of the posterior tibial vein and angiography showing a large amount of thrombus in the vein;B:Puncture of the peroneal vein,and a large amount of thrombus in the peroneal and popliteal veins revealed by angiography;C:Simultaneous visualization of peroneal vein and anterior tibial vein,and planning to puncture the anterior tibial vein;D:Puncture of the peroneal vein and placement of a guide wire
肝素化(75 U/kg),全程静脉造影明确病变,若髂静脉通畅则放置腔静脉临时滤器,若重度狭窄或者闭塞则不放置临时滤器。4 F猪尾巴导管全程搅栓,同时分段团注共25万U尿激酶,留置Unifuse导管(AngioDynmics,美国)于病变近端持续尿激酶泵入。尿激酶起始剂量为100万U/d,每8 h监测血浆纤维蛋白原(fibrinogen,Fg),Fg<1.5 g/L减少剂量,Fg<1.0 g/L停止溶栓;普通肝素起始剂量为10 U/(kg⋅h),每8 h根据活化部分凝血活酶时间(activated partial thromboplastin time,APTT)调整剂量,使APTT延长在2倍左右。每天复查DSA造影并调整Unifuse导管,血栓清除后若有髂静脉压迫则给予球囊扩张/支架植入术。术后利伐沙班抗凝6个月,支架植入者在抗凝基础上同时服用阿司匹林/氯吡格雷3个月[13-14],长期穿弹力袜压力梯度治疗。
1.3 评价标准
参考Vedantham等[15]提出的溶栓评估标准,根据血栓溶解率将疗效分为3级,I级:<50%溶解;II级:50%~95%溶解;III级95%~100%溶解。疗效评价标准:有效:血栓溶解≥50%;无效:血栓溶解<50%。
1.4 随访
术后6、12、18、24个月通过门诊随访。临床症状、体征通过Villalta评分统计,0~4分:无PTS;5~9分:轻度PTS;10~14分:中度PTS;≥15分或有溃疡:重度PTS。慢性静脉功能不全生活质量问卷调查表(construction and validation of a quality of life questionnaire in chronic lower limb venous insufficiency,CIVID-2),分为无、较轻、一般、较重、严重5个等级,对应1、2、3、4、5分,分数越高,生活质量越差,反之亦然。
1.5 统计学处理
计量资料用均数±标准差( ±s)表示,计数资料用百分比表示。采用SPSS 25.0软件进行统计学分析,两组计量资料比较采用t检验,多组资料比较采用方差分析,两组计数资料比较采用χ2检验,P<0.05为差异有统计学意义。
±s)表示,计数资料用百分比表示。采用SPSS 25.0软件进行统计学分析,两组计量资料比较采用t检验,多组资料比较采用方差分析,两组计数资料比较采用χ2检验,P<0.05为差异有统计学意义。
2 结果
2.1 手术结果
本研究无症状性肺栓塞发生,共有57例患者放置腔静脉临时滤器,平均放置时间(7.4±1.2)d,均成功回收。46 例患者共放置52 枚支架。穿刺组3 例患者因小腿深静脉均未显影改穿腘静脉,技术成功率96.6%,其中胫后静脉37 例,腓静脉21 例,胫前静脉28 例。切开组技术成功率100%。穿刺组手术时长(51.6±11.4)min,切开组(127.4±22.9)min,差异有统计学意义(P<0.001)。CDT溶栓通畅率穿刺组为86.5%(77/89),切开组为59.3%(32/54),差异具有统计学意义(P=0.034)。
2.2 临床结果
切开组溶栓过程出现伤口渗血,31 例因伤口渗血减少尿激酶用量,其中5 例出血过多停止溶栓,3例消化道出血;穿刺组2例消化道出血,2例脑出血,其中1例死亡;浅静脉组1例消化道出血,组间差异无统计学意义(P>0.05)。穿刺组大腿周径减少值(7.9±0.5)c m,切开组(7.7±0.3)cm,浅静脉组(7.6±0.4)cm,组间差异有统计学意义(F=4.878,P=0.009);穿刺组小腿周径减少值(4.5±0.3)cm,切开组(4.6±0.2)cm,浅静脉组(4.6±0.3)cm,组间差异无统计学意义(F=1.152,P=0.320);穿刺组尿激酶用量(390.4±34.3)万U,切开组(285.1±49.7)万U,浅静脉组(339.6±72.5)万U,组间差异具有统计学意义(F= 50 .737 ,P<0.001)。大腿周径减少值、尿激酶用量多重比较见表2。
表2 大腿周径减少值、尿激酶用量多重比较结果
Table 2 Results multiple comparisons of the reduction of thigh circumference and doses of urokinase used
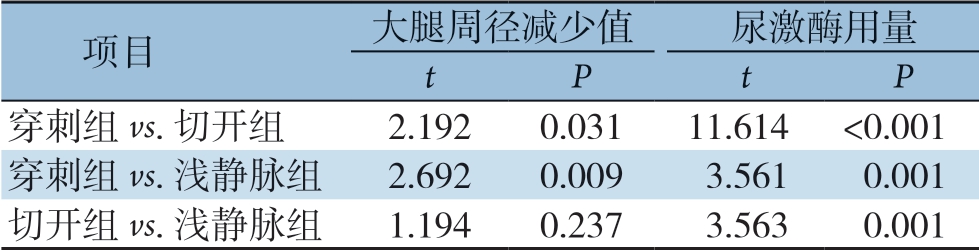
项目大腿周径减少值尿激酶用量tP tP穿刺组vs.切开组2.1920.03111.614 <0.001穿刺组vs.浅静脉组2.6920.0093.5610.001切开组vs.浅静脉组1.1940.2373.5630.001
2.3 随访结果
随访11~36个月,24个月随访完成率83.1%。12个月支架一期通畅率80.8%,二期支架通畅率90.0%。术后6个月,穿刺组轻中度PTS发生率为29.2%,切开组为31.5%,浅静脉组为34.5%,组间差异无统计学意义(χ2=0.301,P=0.860);术后12个月,穿刺组为29.9%,切开组为33.3%,浅静脉组为39.3%,组间差异无统计学意义(χ2=0.875,P=0.646);术后18个月,穿刺组为33.3%,切开组为36.1%,浅静脉组为51.9%,组间差异无统计学意义(χ2=3.010,P=0.222);术后24个月,穿刺组为34.2%,切开组为41.9%,浅静脉组为58.3%,组间差异无统计学意义(χ2=4.446,P=0.108)。各组均无重度PTS发生。
术后6个月,穿刺组Villalta评分为2.7±1.5,切开组为3.3±1.6,浅静脉组为2.5±1.3,组间差异无统计学意义(F=1.177,P=0.302);穿刺组CIVID-2评分为21.8±1.0,切开组为21.6±0.8,浅静脉组为22.3±1.1,组间差异有统计学意义(F=4.117,P=0.019)。术后12个月,穿刺组Villalta 评分为3.0±1.6,切开组为3.6±1.7,浅静脉组为4.7±1.6,组间差异有统计学意义(F=10.005,P<0.001);穿刺组CIVID-2评分为22.1±1.3,切开组为22.6±0.8,浅静脉组为23.3±0.7,组间差异有统计学意义(F=12.341,P<0.001)。术后18 个月,穿刺组Villalta 评分为3.5±1.7,切开组为4.1±1.4,浅静脉组为4.9±1.0,组间差异有统计学意义(F=9.790,P<0.001);穿刺组CIVID-2评分为23.1±1.3,切开组为23.7±0.7,浅静脉组为24.2±1.3,组间差异有统计学意义(F=9.032,P<0.001)。术后24个月,穿刺组Villalta评分为4.4±1.4,切开组为5.1±1.2,浅静脉组为6.3±1.6,组间差异有统计学意义(F=18.624,P<0.001);穿刺组CIVID-2评分为23.9±1.4,切开组为25.0±1.0,浅静脉组为24.8±1.4,组间差异有统计学意义(F=9.747,P<0.001)。术后各阶段Villalta评分、CIVID-2评分差异具有统计学意义的多重比较见表3。
表3 Villalta 评分、CIVID-2 评分多重比较结果
Table 3 Results multiple comparisons of Villalta scores and CIVID-2 scores
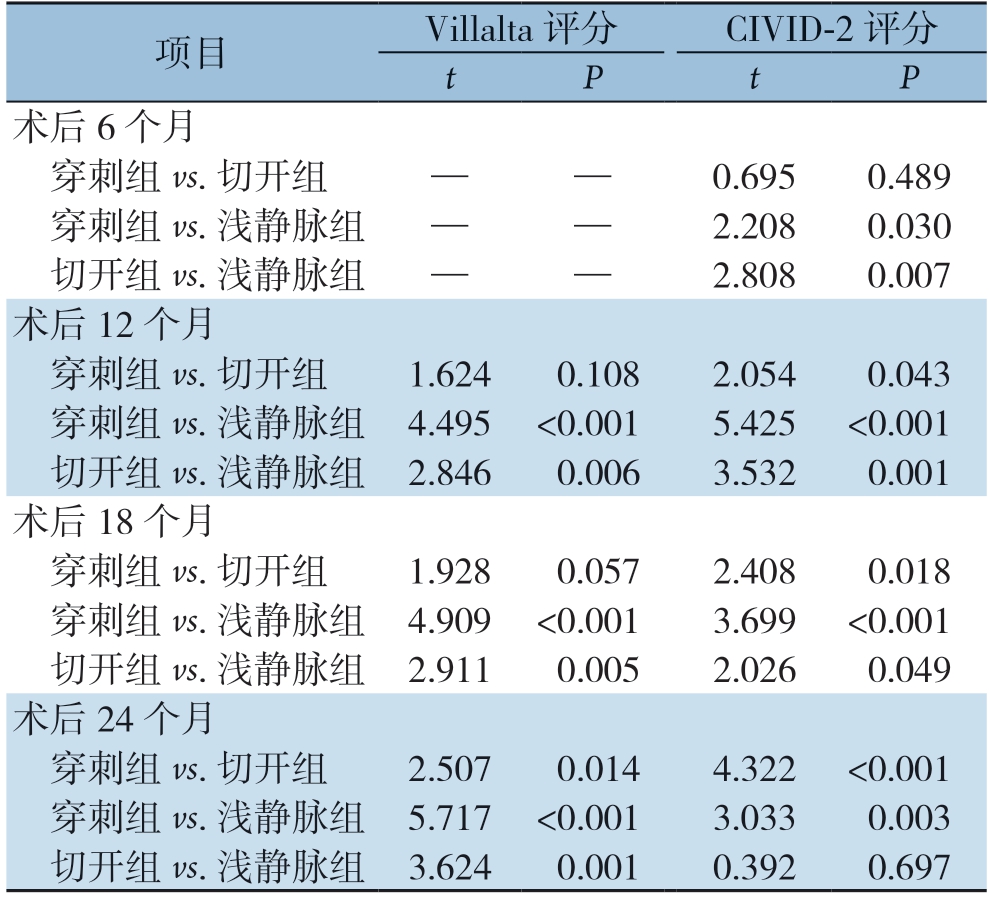
项目Villalta 评分CIVID-2 评分tP tP术后6 个月穿刺组vs.切开组——0.6950.489穿刺组vs.浅静脉组——2.2080.030切开组vs.浅静脉组——2.8080.007术后12 个月穿刺组vs.切开组1.6240.1082.0540.043穿刺组vs.浅静脉组 4.495 <0.0015.425 <0.001切开组vs.浅静脉组 2.8460.0063.5320.001术后18 个月穿刺组vs.切开组1.9280.0572.4080.018穿刺组vs.浅静脉组 4.909 <0.0013.699 <0.001切开组vs.浅静脉组 2.9110.0052.0260.049术后24 个月穿刺组vs.切开组2.5070.0144.322 <0.001穿刺组vs.浅静脉组 5.717 <0.0013.0330.003切开组vs.浅静脉组 3.6240.0010.3920.697
3 讨论
DVT急性期静脉血突然回流受阻,在静脉压力持续增高和血管炎症刺激的双重作用下,静脉瓣膜容易受损,血液倒流,导致下肢出现水肿、疼痛、静脉曲张以及淤滞性溃疡等症状,即PTS。根据“开放静脉学说”原理[16-20],积极清除急性血栓可能会保留静脉功能并预防PTS[21-22]。CDT是在浸润的作用下将纤维蛋白降解物输送到血栓中,尽快恢复血管通畅,降低PTS风险,同时较大程度地减少出血风险[23-24]。而有一项研究[8]显示,CDT及机械性除栓不能有效降低远期PTS发生率,同时增加出血风险。该研究治疗组336例中24个月内有157例(47.0%)进展为PTS,抗凝组355例中有171例(48%)进展为PTS,差异无统计学意义;而10 d内大出血风险治疗组6例,抗凝组1例(1.7% vs.0.3%,P=0.049)。但该结果需慎重看待:该研究使用阿替普酶,与常用的尿激酶不同;失访的80例患者中2/3是抗凝组,数据可能有差异;存在出血风险的患者未被入选治疗组,可能导致治疗效果被低估;该研究长达5年,治疗理念和方法可能存在变化,且CDT和机械性除栓没有单独分析,很难判断CDT的优劣性。现已有多中心临床研究证实[16-19,25],CDT能有效清除血栓,保护静脉瓣膜功能,降低远期PTS的发生率。多数中心通过腘静脉入路治疗中央型DVT,Enden等[16]研究指出,急性DVT血栓清除越多,远期PTS风险越低。针对混合型DVT,腘静脉入路难以覆盖全部病变,小腿部分血栓只能依靠血栓自溶[26],而笔者中心选择小腿深静脉入路行CDT治疗,通过小腿穿通支达到最大程度清除血栓。
足背静脉注射对比剂后,小腿3条主干深静脉可能部分显影,也可能全部显影,取决于血栓堵塞程度和穿通支静脉开放情况。依次显影的顺序也不尽相同,笔者的经验是腓静脉最容易显影,胫前静脉其次,胫后静脉显影最少。穿刺难易程度与静脉直径相关,胫后静脉最粗,较容易穿刺成功,胫前静脉其次,腓静脉最细,最难穿刺。小腿正位时,胫前静脉和腓静脉位于胫腓骨之间,在小腿远端1/3处较难区分,选择直径较粗的静脉穿刺,成功置管后通过DSA造影进行辨别:腓静脉远端较细,上半部分由于接受几条较大的比目鱼肌支而变粗;胫前静脉在小腿中段稍偏外侧,小腿上段处向内侧靠拢并于骨间膜上缘与胫后静脉汇合形成腘静脉,而腓静脉走形相对较笔直。小腿外旋下较易穿刺胫后静脉,若胫后静脉显影建议优先穿刺:一是直径较粗,技术成功率高;二是此处出血容易压迫止血。笔者早期穿刺针选用泰尔茂,技术成功率较低,可能存在以下因素:静脉壁软而薄,针芯过细,穿刺过程中无突破感;静脉压力低,血管腔内大量血栓充盈,同时针套又细,即使用注射器负压回抽也难以判断针套是否在静脉腔内;穿刺过程中步骤太多,针套容易滑出。现改用钢针,穿刺过程中有突破感,由于小腿压力增加,钢针刺破静脉后会有大量血液涌出,固定钢针后再用泰尔茂套件的导丝缓慢进入静脉。确认进入血管后钢针和导丝需同时退出,直到钢针完全退出体外,因为导丝和钢针不是一整个套件,且钢针容易切割导丝,强行退钢针可能使导丝碎片遗留体内。
小腿穿刺入路的主要并发症是误穿动脉出血,是在静脉穿刺过程中误穿伴行动脉,此时只要快速拔出穿刺针并压迫小腿5 min即可继续静脉穿刺。本研究3例误穿动脉患者均顺利完成CDT治疗,无出血相关并发症发生。随着经验的积累,多数患者都是1~2次穿刺成功,即使患者经过多次静脉穿刺,亦无相关静脉出血并发症发生。Palareti等[27]研究结果显示,周围型DVT患者经过抗凝治疗其小腿静脉血栓自溶率高达90%,但Yoon等[28]发现周围型DVT患者远期发生PTS概率为20%~80%,本研究患者经过CDT治疗,患者小腿深静脉基本通畅,总体有效率为81.9%,为了使混合型DVT患者更多获益,相对风险较低的并发症是可以接受的。小腿深静脉直径偏细,对于需要开通髂静脉的患者,笔者一般选择患肢股静脉穿刺,70例患者接受股静脉穿刺行球囊扩张/支架植入术,术前和术后反复经超声、DSA证实,无穿刺相关并发症发生。
PTS的临床表现各异,以互补的方式评估了它的存在和严重性。Villalta评分表通过对主观症状和客观体征进行量化评估,是目前评价PTS最广为应用的评估标准[29-30]。随访期各阶段各组患者PTS发生率差异均无统计学意义,但穿刺组发生率均低于同期切开组,切开组发生率均低于同期浅静脉组。从各阶段Villalta评分和CIVID-2评分多重比较结果分析:⑴两种评分结果并非完全同步;⑵穿刺组治疗效果最优,切开组其次,浅静脉组最差;⑶即使少数差异无统计学意义,但其数值大致符合上述结果。造成以上结果的差异,笔者认为是使用CDT治疗和尿激酶剂量不同。有研究[31]指出,CDT过程中随着尿激酶用量增长,血栓溶解率提高,降低PTS发生率。本研究切开组患者溶栓过程中由于伤口不同程度渗血导致尿激酶减量,其用量明显少于穿刺组,导致穿刺组血栓溶解率优于切开组。重大出血事件上,穿刺组4例(4.5%),切开组3例(5.6%),差异无统计学意义。研究中也存在一些缺陷:患者随访基本都在上午执行,其PTS症状相对较轻,可能导致结果偏差;部分患者失访,造成结果偏差;海南患者工作节奏较慢,生活相对安逸,降低因久站、久坐引起PTS概率。
综上所述,小腿深静脉穿刺行CDT治疗较暴露深静脉置管溶栓、浅静脉溶栓具有更高血栓溶解率,同时没有增加重大出血事件。目前下肢DVT患者行CDT治疗的主流入路是腘静脉,但对于混合型DVT及一些体位要求无法行腘静脉入路的患者,小腿深静脉穿刺入路是一种可选择的治疗方式。
[1]Schleimer K,Barbati ME,Grommes J,et al.Update on diagnosis and treatment strategies in patients with post-thrombotic syndrome due to chronic venous obstruction and role of endovenous recanalization[J].J Vasc Surg Venous Lymphat Disord,2019,7(4):592-600.doi:10.1016/j.jvsv.2019.01.062.
[2]Chait J,Alsheekh A,Aurshina A,et al.Effect of venous access site on postintervention stent thrombosis for nonthrombotic iliac vein stenting[J].J Vasc Surg Venous Lymphat Disord,2020,8(1):84-88.doi:10.1016/j.jvsv.2019.03.014.
[3]Liu G,Qin J,Cui C,et al.Comparison of direct iliofemoral stenting following angiojet rheolytic thrombectomy vs staged stenting after angiojet rheolytic thrombectomy plus catheter-directed thrombolysis in patients with acute deep vein thrombosis[J].J Endovasc Ther,2018,25(1):133-139.doi:10.1177/1526602817714570.
[4]Scheres LJJ,Lijfering WM,Cannegieter SC.Current and future burden of venous thrombosis:Not simply predictable[J].Res Pract Thromb Haemost,2018,2(2):199-208.doi:org/10.1002/rth2.12101.
[5]Tick LW,Kramer MH,Rosendaal FR,et al.Risk factors for post-thrombotic syndrome in patients with a first deep venous thrombosis[J].J Thromb Haemost,2008,6(12):2075-2081.doi:10.1111/j.1538-7836.2008.03180.x.
[6]中华医学会外科学分会血管外科学组.深静脉血栓形成的诊断和治疗指南(第三版)[J].中国血管外科杂志:电子版,2017,9(4):250-257.doi:10.3969/j.issn.1674-7429.2017.04.003.
Group of Vascular Surgery,Society of Surgery,Chinese Medical Association.Guidelines for diagnosis and treatment of deep venous thrombosis(the third edition)[J].Chinese Journal of Vascular Surgery:Electronic Version,2017,9(4):250-257.doi:10.3969/j.issn.1674-7429.2017.04.003.
[7]Streiff MB,Agnelli G,Connors JM,et al.Guidance for the treatment of deep vein thrombosis and pulmonary embolism[J].J Throm Thrombolysis,2016,41(1):32-67.doi:10.1007/s11239-015-1317-0.
[8]Vedantham S,Goldhaber SZ,Julian JA,et al.Pharmacomechanical catheter-directed thrombolysis for deep-vein thrombosis[J].N Engl J Med,2017,377(23):2240-2252.doi:10.1056/NEJMoa1615066.
[9]李长海,刘祥.吸栓后导管溶栓与单纯导管溶栓对急性混合型下肢深静脉血栓的疗效比较[J].中国普通外科杂志,2018,27(12):1525-1530.doi:10.7659/j.issn.1005-6947.2018.12.005.
Li CH,Liu X.Efficacy comparison of thrombus aspiration plus catheter directed thrombolysis and catheter thrombolysis alone for acute mixed deep venous thrombosis of lower extremities[J].Chinese Journal of General Surgery,2018,27(12):1525-1530.doi:10.7659/j.issn.1005-6947.2018.12.005.
[10]Haig Y,Enden T,Slagsvold CE,et al.Determinants of early an d long-term efficacy of catheter-directed thrombolysis in proximal deep venous thrombosis[J].J Vasc Interv Radiol,2013,24(1):17-24.doi:10.1016/j.jvir.2012.09.023.
[11]Sharafuddin MJ,Sun S,Hoballah JJ,et al.Endovascular management of venous thrombotic and occlusive diseases of the lower extremities[J].J Vasc Interv Radiol,2003,14(4):405-423.doi:10.1097/01.rvi.0000064849.87207.4f.
[12]赵得银,于智勇,张艮龙,等.经腘静脉与膝下静脉入路置管溶栓治疗急性下肢深静脉血栓的效果比较[J].山东医药,2020,60(5):84-87.doi:10.3969/j.issn.1002-266X.2020.05.023.
Zhao DY,Yu ZY,Zhang GL,et al.Catheter-directed thrombolysis via popliteal vein approach versus below-the-knee vein approach in treatment of deep venous thrombosis of the lower limbs[J].Shandong Medical Journal,2020,60(5):84-87.doi:10.3969/j.issn.1002-266X.2020.05.023.
[13]Taha MA,Busuttil A,Bootun R,et al.A systematic review on the use of deep venous stenting for acute venous thrombosis of the lower limb[J].Phlebology,2019,34(2):115-127.doi:10.1177/0268355518772760.
[14]Avgerinos ED,Saadeddin Z,Abou AA,et al.Outcomes and predictors of failure of iliac vein stenting after catheter-directed thrombolysis for acute iliofemoral thrombosis[J].J Vasc Surg Venous Lymphat Disord,2019,7(2):153-161.doi:10.1016/j.jvsv.2018.08.014.
[15]Vedantham S,Grassi CJ,Ferral H,et al.Reporting standards for endovascular treatment of lower extremity deep vein thrombosis[J].J Vasc Interv Radiol,2009,20(7 Suppl):S391-408.doi:10.1016/j.jvir.2009.04.034.
[16]Enden T,Haig Y,Kløw NE,et al.Long-term outcome after additional catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep vein thrombosis(the CaVenT study):a randomised controlled trial[J].Lancet,2012,379(9810):31-38.doi:10.1016/S0140-6736(11)61753-4.
[17]孙万里,温世奇,陈泉,等.重组人尿激酶原经导管溶栓治疗急性髂股深静脉血栓的疗效观察[J].中国普通外科杂志,2019,28(12):1507-1512.doi:10.7659/j.issn.1005-6947.2019.12.010.
Sun WL,Wen SQ,Chen Q,et al.Efficacy observation of catheterdirected thrombolysis with recombinant human prourokinase in treatment of acute iliofemoral deep venous thrombosis[J].Chinese Journal of General Surgery,2019,28(12):1507-1512.doi:10.7659/j.issn.1005-6947.2019.12.010.
[18]任贤英.深静脉给药治疗下肢深静脉血栓形成[J].中国普通外科杂志,2007,16(12):1217-1218.doi:10.3969/j.issn.1005-6947.2007.12.028.
Ren XY.Deep venous thrombosis of lower extremities treated by drug administration into the deep veins[J].Chinese Journal of General Surgery,2007,16(12):1217-1218.doi:10.3969/j.issn.1005-6947.2007.12.028.
[19]Akhtar OS,Lakhter V,Zack CJ,et a1.Contemporary Trends and Comparative Outcomes With Adjunctive Inferior Vena Cava Filter Placement in Patients Undergoing Catheter-Directed Thrombolysis for Deep Vein Thrombosis in the United States:Insights From the National Inpatient Sample[J].JACC Cardiovasc Interv,2018,11(14):1390-1397.doi:10.1016/j.jcin.2018.04.048.
[20]Watson L,Broderick C,Armon MP.Thrombolysis for acute deep vein thrombosis[J].Cochrane Database Syst Rev,2016,11:CD002783.doi:10.1002/14651858.CD002783.
[21]Ghanima W,Wik HS,Tavoly M,et al.Late consequences of venous thromboembolism:Measuring quality of life after deep vein thrombosis and pulmonary embolism[J].Thromb Res,2018,164:170-176.doi:10.1016/j.thromres.2017.07.025.
[22]刘飒华,肖占祥,戚悠飞,等.DSA引导下胫后/胫前静脉穿刺置管碎栓/溶栓治疗急性下肢深静脉血栓形成[J].中国普通外科杂志,2017,26(6):758-763.doi:10.3978/j.issn.1005-6947.2017.06.014.
Liu SH,Xiao ZX,Qi YF,et al.DSA-guided posterior/anterior tibial vein puncture and catheter-directed clot fragmentation/thrombolysis for acute lower extremity deep venous thrombosis[J].Chinese Journal of General Surgery,2017,26(6):758-763.doi:10.3978/j.issn.1005-6947.2017.06.014.
[23]Cynamon J,Stein EG,Dym RJ,et al.A new method for aggressive management of deep vein thrombosis:retrospective study of the power pulse technique[J].J Vasc Interv Radiol,2006,17(6):1043-1049.doi:10.1097/01.RVI.0000221085.25333.40.
[24]Hilleman DE,Razavi MK.Clinical and economic evaluation of the Trellis-8 infusion catheter for deep vein thrombosis[J].J Vasc Interv Radiol,2008,19(3):377-383.doi:10.1016/j.jvir.2007.10.027.
[25]Alhazmi L,Moustafa A,Mangi MA,et al.Efficacy and safety of catheter-directed thrombolysis in preventing post-thrombotic syndrome:a meta-analysis[J].Cureus,2019,11(2):e4152.doi:10.7759/cureus.4152.
[26]Bendix SD,Nolan R,Banipal S,et al.Posterior tibial vein approach to catheter-directed thrombolysis for iliofemoral deep venous thrombosis[J].J Vasc Surg Venous Lymphat Disord,2019,7(5):629-634.doi:10.1016/j.jvsv.2019.01.064.
[27]Palareti G,Cosmi B,Lessiani G,et al.Evolution of untreated calf deep-vein thrombosis in high risk symptomatic outpatients:the blind,prospective CALTHRO study[J].Thromb Haemost,2010,104(5):1063-1070.doi:10.1160/TH10-06-0351.
[28]Yoon DY,Riaz,A,Teter K,et al.Surveillance,anticoagulation,or filter in calf vein thrombosis[J].J Vasc Surg Venous Lymphat Disord,2017,5(1):25-32.doi:10.1016/j.jvsv.2016.08.007.
[29]Kalan SR,Partsch H,Vedantham S,et al.Definition of post thrombotic syndrome of the leg for use in clinical investigations:a recommendation for standardization[J].J Thromb Haemost,2009,7(5):879-883.doi:10.1111/j.1538-7836.2009.03294.x.
[30]Engeseth M,Enden T,Andersen MH,et al.Does the Villalta scale capture the essence of postthrombotic syndrome?A qualitative study of patient experience and expert opinion[J].J Thromb Haemost,2019,17(10):1707-1714.doi:10.1111/jth.14557.
[31]董波,王暐,王夕栩,等.不同剂量尿激酶经导管溶栓治疗下肢深静脉血栓形成的疗效[J].中国现代普通外科进展,2018,21(5):360-364.doi:10.3969/j.issn.1009-9905.2018.05.006.
Dong B,Wang W,Wang XX,et al.Curative effect of different dosage of urokinase for catheter-directed thrombolysis of deep venous thrombosis[J].Chinese Journal of Current Advances in General Surgery,2018,21(5):360-364.doi:10.3969/j.issn.1009-9905.2018.05.006.
